Abstract
Purpose
Surgical outcomes data for patent ductus arteriosus (PDA) ligation come primarily from single institution case series. The purpose of this study was to evaluate national PDA ligation trends, and to compare outcomes between pediatric general (GEN) and pediatric cardiothoracic (CT) surgeons.
Methods
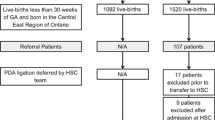
The Pediatric Health Information System database was queried to identify neonates who underwent PDA ligation from 2006 through 2009. Outcomes evaluated included surgical morbidity, in-hospital mortality, length of stay, and total charges. Outcomes were compared between pediatric general and pediatric cardiothoracic surgeons.
Results
The records of 1,482 neonates who underwent PDA ligation were identified and analyzed. Overall mean gestational age was 26 ± 3 weeks and birth weight was 888 ± 428 g. The majority of patients among both surgeons had birth weights of ≤1,000 g (77.2 %) and were born at ≤27-week gestation (81.5 %). Most of the PDA ligations were performed by pediatric CT surgeons (n = 1,196, 80.7 %). The mortality rate did not differ by surgeon subspecialty training (GEN = 5.2 %, CT 7.9 %, p = 0.16). Neonates in the cardiothoracic surgeon cohort showed lower length of stay (p < 0.001–0.05) and total hospital charges (p < 0.05) among patients with birth weight ≤1,200 g. Proxy measures of surgical morbidity—gastrostomy, fundoplication, and tracheostomy—showed no significant differences between the two surgical subspecialists overall or across birth weight subgroups (p > 0.05).
Conclusion
These data provide a contemporary snapshot of PDA ligation outcomes at American children’s hospitals. Pediatric general surgeons achieve comparable outcomes performing PDA ligation compared to pediatric cardiothoracic surgeons.


Similar content being viewed by others
References
Kitterman JA, Edmunds LH, Gregory GA et al (1972) Patent ducts arteriosus in premature infants. Incidence, relation to pulmonary disease and management. N Engl J Med 287:473–477
Investigators of the Vermont-Oxford Trials Network Database Project (1993) The Vermont-Oxford Trials Network: very low birth weight outcomes for 1990. Pediatrics 91(3):540–545
Campbell M (1968) Natural history of persistent ductus arteriosus. Br Heart J 30:4–13
Cotton RB, Stahlman MT, Kovar I et al (1978) Medical management of small preterm infants with symptomatic patent ductus arteriosus. J Pediatr 92:467–473
Hamrick SEG, Hansmann G (2010) Patent ductus arteriosus of the preterm infant. Pediatrics 125:1020–1030
Clyman RI (2000) Ibuprofen and patent ductus arteriosus. N Engl J Med 343:728–730
Van Overmeire B, Smets K, Lecoutere D et al (2000) A comparison of ibuprofen and indomethacin for closure of patent ductus arteriosus. N Engl J Med 343:674–681
Chorne N, Leonard C, Piecuch R et al (2007) Patent ductus arteriosus and its treatment as risk factors for neonatal and neurodevelopmental morbidity. Pediatrics 119:1165–1174
Raval M, Laughon MM, Bose CL et al (2007) Patent ductus arteriosus ligation in premature infants: who really benefits, and at what cost? J Pediatr Surg 42:69–75
Lee L, Tillett A, Tulloh R et al (2006) Outcome following patent ductus arteriosus ligation in premature infants: a retrospective cohort analysis. BMC Pediatr 6:15
Gross R (1944) Complete surgical division of the patent ductus arteriosus: a report of fourteen successful cases. Surg Gynecol Obs 78:36–43
Children’s Hospital Association, Inc. (2012) http://www.childrenshospitals.org/index.html. Accessed 7 Apr 2013
Shackford SR, Kahl JE, Calvo RY et al (2013) Limb salvage after complex repairs of extremity arterial injuries is independent of surgical specialty training. J Trauma Acute Care Surg 74:716–723
Borenstein SH, To T, Wajja A et al (2005) Effect of subspecialty training and volume on outcome after pediatric inguinal hernia repair. J Pediatr Surg 40:75–80
Pranikoff T, Campbell BT, Travis J et al (2002) Differences in outcome with subspecialty care: pyloromyotomy in North Carolina. J Pediatr Surg 37:352–356
Somme S, To T, Langer JC (2007) Effect of subspecialty training on outcome after pediatric appendectomy. J Pediatr Surg 42:221–226
Schipper PH, Diggs BS, Ungerleider RM et al (2009) The influence of surgeon specialty on outcomes in general thoracic surgery: a national sample 1996 to 2005. Ann Thorac Surg 88:1566–1572
Hutchings K, Vasquez A, Price D et al (2013) Outcomes following neonatal patent ductus arteriosus ligation done by pediatric surgeons: a retrospective cohort analysis. J Pediatr Surg 48:915–918
Mandhan P, Brown S, Kukkady A et al (2009) Surgical closure of patent ductus arteriosus in preterm low birth weight infants. Congenit Heart Dis 4:34–37
Zbar RI, Chen a H, Behrendt DM et al (1996) Incidence of vocal fold paralysis in infants undergoing ligation of patent ductus arteriosus. Ann Thorac Surg 61:814–816
Tyson J, Parikh N, Langer J et al (2008) Intensive care for extreme prematurity—moving beyond gestational age. New Engl J Med 358:1672–1681
Best WR, Khuri SF, Phelan M et al (2002) Identifying patient preoperative risk factors and postoperative adverse events in administrative databases: results from the Department of Veterans Affairs National Surgical Quality Improvement Program. J Am Coll Surg 194:257–266
Benjamin JR, Smith PB, Cotten CM et al (2010) Long-term morbidities associated with vocal cord paralysis after surgical closure of a patent ductus arteriosus in extremely low birth weight infants. J Perinatol 30:408–413
Sachdeva R, Hussain E, Moss MM et al (2007) Vocal cord dysfunction and feeding difficulties after pediatric cardiovascular surgery. J Pediatr 151:312–315
Clement WA, El-Hakim H, Phillipos EZ et al (2008) Unilateral vocal cord paralysis following patent ductus arteriosus ligation in extremely low-birth-weight infants. Arch Otolaryngol Head Neck Surg 134:28–33
Pereira KD, Webb BD, Blakely ML et al (2006) Sequelae of recurrent laryngeal nerve injury after patent ductus arteriosus ligation. Int J Pediatr Otorhinolaryngol 70:1609–1612
Herbst MA, Mercer BM, Beazley D et al (2003) Relationship of prenatal care and perinatal morbidity in low-birth-weight infants. Am J Obstet Gynecol 189:930–933
Cotten CM, Oh W, McDonald S et al (2005) Prolonged hospital stay for extremely premature infants: risk factors, center differences, and the impact of mortality on selecting a best-performing center. J Perinatol 25:650–655
Echtler K, Stark K, Lorenz M et al (2010) Platelets contribute to postnatal occlusion of the ductus arteriosus. Nat Med 16:75–82
Rothenberg SS, Chang JH, Toews WH et al (1995) Thoracoscopic closure of patent ductus arteriosus: a less traumatic and more cost-effective technique. J Pediatr Surg 30:1057–1060
Burke RP, Jacobs JP, Cheng W et al (1999) Video-assisted thoracoscopic surgery for patent ductus arteriosus in low birth weight neonates and infants. Pediatrics 104:227–230
Bianchi A, Sowande O, Alizai NK et al (1998) Aesthetics and lateral thoracotomy in the neonate. J Pediatr Surg 33:1798–1800
Vanamo K, Berg E, Kokki H et al (2006) Video-assisted thoracoscopic versus open surgery for persistent ductus arteriosus. J Pediatr Surg 41:1226–1229
Grimes DA, Schulz KF (2002) Descriptive studies: what they can and cannot do. Lancet 359:145–149
Albanese MA, Mejicano G, Mullan P et al (2008) Defining characteristics of educational competencies. Med Educ 42:248–255
Govaerts MJB (2008) Educational competencies or education for professional competence? Med Educ 42:234–236
Poley S, Ricketts T, Belsky D et al (2010) Pediatric surgeons: subspecialists increase faster than generalists. Bull Am Coll Surg 95:35–38
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Markush, D., Briden, K.E., Chung, M. et al. Effect of surgical subspecialty training on patent ductus arteriosus ligation outcomes. Pediatr Surg Int 30, 503–509 (2014). https://doi.org/10.1007/s00383-014-3469-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-014-3469-y