Abstract
Purpose
To evaluate change in the severity of hypoxic-ischemic encephalopathy (HIE) and associated morbidities between pre- and during COVID-19 pandemic periods in Canada.
Methods
We conducted a retrospective cohort study extracting the data from level-3 NICUs participating in Canadian Neonatal Network (CNN). The primary outcome was a composite of death in the first week after birth and/or stage 3 HIE (Sarnat and Sarnat). Secondary outcomes included rate and severity of HIE among admitted neonates, overall mortality, brain injury on magnetic resonance imaging (MRI), neonates requiring resuscitation, organ dysfunction, and therapeutic hypothermia (TH) usage. We included 1591 neonates with gestational age ≥ 36 weeks with HIE during the specified periods: pandemic cohort from April 1st to December 31st of 2020; pre-pandemic cohort between April 1st and December 31st of 2017, 2018, and 2019. We calculated the odds ratio (OR) and confidence intervals (CI).
Results
We observed no significant difference in the primary outcome (15% vs. 16%; OR 1.08; 95%CI 0.78–1.48), mortality in the first week after birth (6% vs. 6%; OR 1.10, 95%CI 0.69–1.75), neonates requiring resuscitation, organ dysfunction, TH usage, or rate of brain injury. In the ad hoc analysis, per 1000 live births, there was an increase in the rate of infants with HIE and TH use.
Conclusions
Severity of HIE, associated morbidities, and mortality were not significantly different during the pandemic lockdown compared to a pre-pandemic period in Canada. Anticipated risks and difficulties in accessing healthcare have not increased the mortality and morbidities in neonates with HIE in Canada.
Similar content being viewed by others
Introduction
Hypoxic-ischemic encephalopathy (HIE) is a devastating disease, leading to mortality and long-term morbidities in many neonates [1,2,3]. Incidence of HIE in developed countries varies between 0.9 and 3.8 per 1000 live births [4, 5]. HIE outcomes in neonates depend on the severity and duration of the initial insult [5, 6]. Some additional risk factors for HIE which warrant immediate attention are prolonged rupture of membranes, meconium-stained amniotic fluid, tight nuchal cord, umbilical cord prolapse, abruptio placenta, uterine rupture, and abnormal cardiotocography [5, 7, 8].
COVID-19 pandemic affected the healthcare services; many aspects are still unknown and unfolding. Visitations to the obstetric triage, high-risk clinics, and ultrasound clinics were delayed and decreased during the pandemic, with a resultant increase in the incidence of acute interventions and instrumental deliveries [9,10,11,12]. Substantial decrease in hospitalization of pregnant women was observed during the COVID-19 pandemic due to the fear of contracting the infection [13]. Although systematic reviews on pregnancy outcomes showed an increased incidence of pre-eclampsia and gestational diabetes mellitus, the incidence of stillbirths was similar, and preterm births were decreased during the COVID-19 pandemic [14, 15].
The publicly funded Canadian healthcare system and provinces have regionalized neonatal care, with some differences in the number of high-acuity neonatal beds [16]. The first case of COVID-19 in Canada was reported on January 25th, 2020, and the lockdown was implemented on March 18th, 2020. The lockdown stringency index in Canada was around 65–70 on a scale of 0–100 (100 being the strictest lockdown), and there was minimal variation between the provinces during 2020 [17,18,19]. This study aimed to compare the severity and outcomes of neonates with HIE admitted to tertiary NICUs in Canada before and during the pandemic.
Methods
Study design
We conducted a population-representative, retrospective cohort study of all neonates diagnosed with HIE admitted to tertiary Canadian Neonatal Network (CNN) centres before and during the pandemic. The pandemic cohort included neonates born during the COVID-19 lockdown between April 1st and December 31st of 2020. The pre-pandemic cohorts included neonates born from April 1st to December 31st of 2017, 2018, and 2019 (the pre-pandemic cohort). We did not include infants born from January to March to reduce the potential bias due to seasonal variation in births and/or outcomes. Seasonality of births is a well-established phenomenon, where the climate, birth month preference, socioeconomic status, and contraceptive practices, among other factors, play a role. [20,21,22] We compared the pandemic cohort with the pre-pandemic cohort and analysed the differences in outcomes over the 4 years. We analysed the outcomes over 4 years to appreciate a general increase in the trends unrelated to the pandemic.
Patients and settings
We included term and near-term neonates (gestational age (GA) ≥ 36 weeks) with a diagnosis of HIE [23], admitted to one of the level 3 neonatal intensive care units (NICU) participating in the CNN during the specified periods. We excluded neonates with birth weight < 1.8 kg, surgical conditions, and major congenital anomalies.
Outcomes
The primary outcome of this study was a composite of death in the first week after birth and/or stage 3 HIE (based on Sarnat and Sarnat) [24]. The secondary outcomes were as follows: number of neonates with HIE of any grade, mortality in the first week after birth, overall mortality, difference in 5- and 10-min APGAR scores, number of neonates requiring chest compressions in the delivery room, seizures, organ dysfunction (cardiac, renal, and hepatic), incidence of brain injury on MRI, and rates of use of therapeutic hypothermia (TH).
We collected the demographic characteristics and outcomes from the CNN database. At each of the 31 sites participating in the CNN, neonatal data are collected from patient charts by trained abstractors according to standard definitions and entered electronically into a customized data entry program with built-in error checks. The database showed very high internal consistency and reliability [25]. Diagnosis of HIE was based on the presence of neonatal encephalopathy on admission, in association with a documented acute perinatal event, and evidence of intrapartum hypoxia (at least one of the following criteria: 10-min Apgar score ≤ 5, ongoing mechanical ventilation or resuscitation at 10 min of birth, or cord pH ≤ 7.00 or postnatal blood gas pH ≤ 7.00 or base deficit ≤ –16 within 60 min of birth) [23]. Seizures were diagnosed clinically or by electroencephalography. Cardiac dysfunction was defined as receiving inotropes or echocardiography findings of cardiac dysfunction. Liver dysfunction was defined as elevated liver enzymes (aspartate transaminase (AST) or alanine transaminase (ALT) > 100 IU) at any time in the first 7 days after birth. Renal failure was diagnosed as urine output < 0.5 ml/kg/h for 6 h or rising creatinine > 100 mmol/l within the first 72 h. Disseminated intravascular coagulation (DIC) was diagnosed based on laboratory or clinical evidence of coagulopathy. Persistent pulmonary hypertension (PPHN) was diagnosed on echocardiography. Evidence of brain injury was defined as signal abnormalities in MRI sequences in the watershed areas, deep gray matter, or a mixed pattern [23, 26,27,28].
Statistical methods
We compared neonates born in the pre-pandemic period to those admitted during the pandemic lockdown for primary analyses. Baseline characteristics were expressed as count and percentages for categorical variables and mean and standard deviation (SD) for continuous variables. Categorical variables were compared by Fisher’s exact test or chi-square test and continuous variables by Student’s t-test (two-sided) if normally distributed and Mann–Whitney U test if not normally distributed. We analysed the trends of outcomes of neonates with HIE over the 4 years (April 1st to December 31st of 2017–2020). The tests used were two-sided, and significance was defined as a p-value < 0.05. Data management and statistical analyses were performed using SAS, version 9.3 (SAS Institute Inc., Cary, NC).
Approvals
CNN Executive Committee approved the study, and the University of Calgary Conjoint Health Research Ethics Board provided ethics clearance (REB21-0497).
Results
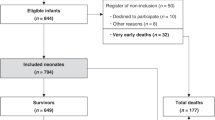
The total number of neonates diagnosed with HIE during the study period was 1591, of which we excluded 45 neonates (birth weight < 1800 g = 5 neonates, and major congenital anomaly = 40 neonates) (Fig. 1). As reported in Table 1, baseline characteristics did not reveal any significant differences between pre-pandemic and pandemic periods. Results of the primary and secondary outcomes are reported in Table 2. The composite outcome of death in the first week after birth and/or stage 3 HIE was 16% in the pandemic and 15% in the pre-pandemic periods (OR 1.08; 95% CI 0.78–1.48). Mortality in the first week after birth was 6% in both cohorts (OR 1.10, 95% CI 0.69–1.75). Overall mortality was also similar between the pandemic and pre-pandemic cohorts (7% vs. 7%, OR 1.02, 95% CI 0.67–1.55).
There was no difference in the number of neonates requiring delivery room chest compression and assisted ventilation in both cohorts. About one-quarter of the neonates had mild HIE (26%), and nearly half had moderate HIE in the two time periods. The incidence of stage 3 HIE was also similar in both cohorts (13% in pre-pandemic and 14% in the pandemic period). Other secondary outcomes such as seizures, organ dysfunction, DIC, and PPHN in neonates with HIE were similar between the study periods. There was no difference in the incidence of brain injury on MRI scan among neonates with available MRI data (27% vs. 30%, OR 1.24, 95% CI 0.97–1.58).
We analysed the trends for outcomes over the 4 years to see a general increase in the rates of events unrelated to the pandemic. There was an increasing trend over the 4-year study period for the total number of neonates with HIE. However, trends for primary and secondary outcomes were not statistically significant (Supplementary Table 1). Complete data on all births in the country during the study period was unavailable. Nevertheless, to explore the possible changes in the rates of HIE, we conducted an ad hoc analysis and calculated the rate of infants admitted with HIE to CNN sites among all live births in Canada during the corresponding periods [29]. When compared to the pre-pandemic cohort, there was a significant increase in the rates of neonates with HIE per 1000 live births in the pandemic cohort (p < 0.001; risk difference (RD) 0.04, 95% CI 0.02–0.05). The rate of use of TH per 1000 live births also was significantly higher in the pandemic cohort compared to the pre-pandemic period (p = < 0.001, RD 0.004; 95% CI 0.03–0.006).
Discussion
In this national population-representative cohort, we identified no significant difference in the composite of mortality and/or stage 3 HIE, mortality, or morbidities of neonates with HIE admitted to tertiary NICUs in Canada during the pandemic period when compared to a pre-pandemic period. There was also no difference in the trends of the outcomes studied.
During the COVID-19 pandemic lockdown, there was a difference in the profile of pregnant women presenting to the emergency room, health-seeking behaviours, difficulty in accessing healthcare, and a delay in providing care after admission to the hospital [9, 12, 13]. Concurrently, there were also increased rates of prolonged rupture of membranes, abruptio placenta, foetal distress, patients admitted in active labour, acute interventions in pregnant women, and operative deliveries during the pandemic lockdown [9,10,11,12,13, 30]. Some of these additional risk factors were found to be preventable and modifiable [31]. Pregnant women may also respond late to some of the warning signs of foetal distress such as absent/decreased foetal movements, signs of hypertension, bleeding, or worsening glucose control. A study from Nepal showed a decrease in the incidence of institutional deliveries and an increase in neonatal mortality [32]. All these could serve as risk factors for perinatal asphyxia and may increase the incidence of mortality and/or severe HIE. A population-based cohort study done in Sweden analyzing the risk factors for HIE concluded that careful assessment of acute obstetrical events and timely interventions could potentially decrease perinatal damage [5].
A recently published Canadian study, however, did not show a difference in the incidence of NICU admissions or neonatal deaths during the pandemic period [17, 33]. Kugelman et al. also reported that maternal and neonatal morbidity rates were not different during the pandemic, though there was an increase in the rates of emergency birth-related interventions [12]. Our hypothesis that neonates born during the pandemic period might have had higher mortality and/or severe injury based on the published poor perinatal outcomes was not supported by our results. Neonates born during the pandemic period did not have higher rates of HIE or associated morbidities.
In our ad hoc analysis, when compared to the total live births in Canada, there was an increase in the rate of infants with HIE per 1000 live births and the rate of infants receiving TH per 1000 live births in CNN sites which may be interpreted as an increase during the pandemic period. However, these results should be interpreted with caution for the following reasons: (1) Neonates with mild HIE may be born in the community and did not reach level 3 NICU; (2) There might be some immediate postnatal deaths that do not reach the tertiary NICU; and (3) There might be a difference in the referral practices over the 4-year study period unrelated to the pandemic lockdown.
There are several potential reasons for not finding a difference in the outcomes studied. Firstly, our sample size may be inadequate as we only included neonates born during 9 months (April to December 2020). Even though we had > 300 patients in each year, it may not be enough to detect minor differences. Secondly, contrary to our speculation, access to the healthcare system may not have been as restricted. Data from the National Physician Database in Canada in 2021 showed that more patients chose virtual healthcare during the pandemic [34, 35]. Based on the data, though there was a significant shift to virtual care, patients with a higher level of morbidity were still provided appropriate healthcare through virtual platforms [34]. It is possible that in the context of the universal Canadian healthcare system and the fast adoption of virtual healthcare, pregnant women were attended to with similar rigour during the pandemic and thus did not compromise neonatal care.
Strengths and limitations
Our data extracted are population-representative and come from a robust data collection system. However, we acknowledge some limitations to our study. Data of neonates not admitted to the level 3 NICU and those who died (stillbirths or immediate postnatal deaths) at the referring centres were not captured in both periods. However, in Ontario, one of the large provinces of Canada, the stillbirth rate was not different during the pandemic period [17]. The database does not capture all the births; hence, some neonates with mild HIE cared for at level-2 units might have been missed. Referral practices also might have varied over the last 4 years; however, we did not see an increase in the incidence of mild HIE, as would be expected with increased referrals. Finally, this study did not capture the phased lockdown relaxation period in 2021; however, it is unlikely we would have seen a change given there were no differences in outcome during strict lockdown.
Conclusion
The severity of HIE, mortality, and morbidity related to HIE during the COVID-19 pandemic period in Canada was not different from that of a pre-pandemic period. Creating awareness among pregnant women about timely access to the healthcare system may have helped prevent the unmeasured, unintended complications of the pandemic lockdown. Population-based studies that tend to capture complete data would help assess the actual difference. Further studies from larger cohorts and different healthcare system settings are needed to fully understand the impact of pandemic and lockdown.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Longo M, Hankins GDV (2009) Defining cerebral palsy: pathogenesis, pathophysiology and new intervention. Minerva Ginecol 61:421–429
Pappas A, Korzeniewski SJ (2016) Long-term cognitive outcomes of birth asphyxia and the contribution of identified perinatal asphyxia to cerebral palsy. Clin Perinatol 43:559–572. https://doi.org/10.1016/j.clp.2016.04.012
GBD (2013) Mortality and Causes of Death Collaborators (2015) Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet Lond Engl 385:117–171. https://doi.org/10.1016/S0140-6736(14)61682-2
Kurinczuk JJ, White-Koning M, Badawi N (2010) Epidemiology of neonatal encephalopathy and hypoxic-ischaemic encephalopathy. Early Hum Dev 86:329–338. https://doi.org/10.1016/j.earlhumdev.2010.05.010
Lundgren C, Brudin L, Wanby A-S, Blomberg M (2018) Ante- and intrapartum risk factors for neonatal hypoxic ischemic encephalopathy. J Matern Fetal Neonatal Med 31:1595–1601. https://doi.org/10.1080/14767058.2017.1321628
Shah P, Perlman M (2009) Time courses of intrapartum asphyxia: neonatal characteristics and outcomes. Am J Perinatol 26:039–044. https://doi.org/10.1055/s-0028-1095185
Peebles PJ, Duello TM, Eickhoff JC, McAdams RM (2020) Antenatal and intrapartum risk factors for neonatal hypoxic ischemic encephalopathy. J Perinatol 40:63–69. https://doi.org/10.1038/s41372-019-0531-6
Martinez-Biarge M, Diez-Sebastian J, Wusthoff CJ et al (2013) Antepartum and intrapartum factors preceding neonatal hypoxic-ischemic encephalopathy. Pediatrics 132:e952–e959. https://doi.org/10.1542/peds.2013-0511
Justman N, Shahak G, Gutzeit O et al (2020) Lockdown with a Price: the impact of the COVID-19 pandemic on prenatal care and perinatal outcomes in a tertiary care center. Isr Med Assoc J IMAJ 22:533–537
Mor M, Kugler N, Jauniaux E et al (2021) Impact of the COVID-19 pandemic on excess perinatal mortality and morbidity in Israel. Am J Perinatol 38:398–403. https://doi.org/10.1055/s-0040-1721515
Meyer R, Levin G, Hendin N, Katorza E (2020) Impact of the COVID-19 outbreak on routine obstetrical management. Isr Med Assoc J IMAJ 22:483–488
Kugelman N, Lavie O, Assaf W et al (2020) Changes in the obstetrical emergency department profile during the COVID-19 pandemic. J Matern-Fetal Neonatal Med Off J Eur Assoc Perinat Med Fed Asia Ocean Perinat Soc Int Soc Perinat Obstet. https://doi.org/10.1080/14767058.2020.1847072
Kumari V, Mehta K, Choudhary R (2020) COVID-19 outbreak and decreased hospitalisation of pregnant women in labour. Lancet Glob Health 8:e1116–e1117. https://doi.org/10.1016/S2214-109X(20)30319-3
Wei SQ, Bilodeau-Bertrand M, Liu S, Auger N (2021) The impact of COVID-19 on pregnancy outcomes: a systematic review and meta-analysis. Can Med Assoc J 193:E540–E548. https://doi.org/10.1503/cmaj.202604
Yang J, D’Souza R, Kharrat A et al (2022) Coronavirus disease 2019 pandemic and pregnancy and neonatal outcomes in general population: a living systematic review and meta-analysis (updated Aug 14, 2021). Acta Obstet Gynecol Scand 101:7–24. https://doi.org/10.1111/aogs.14277
Rizzolo A, Shah PS, Bertelle V et al (2021) Association of timing of birth with mortality among preterm infants born in Canada. J Perinatol Off J Calif Perinat Assoc 41:2597–2606. https://doi.org/10.1038/s41372-021-01092-9
Shah PS, Ye XY, Yang J, Campitelli MA (2021) Preterm birth and stillbirth rates during the COVID-19 pandemic: a population-based cohort study. Can Med Assoc J 193:E1164–E1172. https://doi.org/10.1503/cmaj.210081
Ritchie H, Mathieu E, Rodés-Guirao L et al (2020) Coronavirus Pandemic (COVID-19). In: Our World Data Available via GOOGLE. https://ourworldindata.org/coronavirus/country/canada#government-stringency-index. Accessed 8 Jun 2022
Wood A, Smith J, Sawatsky J et al (2021) Variation in the Canadian provincial and territorial responses to COVID-19. Available via GOOGLE. https://www.bsg.ox.ac.uk/research/publications/variation-canadian-provincial-and-territorial-responses-covid-19. Accessed 9 Dec 2021
Werschler T, Halli S (1992) The seasonality of births in Canada: a comparison with the northern United States. Popul Environ 14:85–94
Chaudhury RH (1972) Socioeconomic and seasonal variations in births: a replication. Soc Biol 19:65–68. https://doi.org/10.1080/19485565.1972.9987967
Mathers CD, Harris RS (1983) Seasonal distribution of births in Australia. Int J Epidemiol 12:326–331. https://doi.org/10.1093/ije/12.3.326
Xu EH, Claveau M, Yoon EW et al (2020) Neonates with hypoxic-ischemic encephalopathy treated with hypothermia: observations in a large Canadian population and determinants of death and/or brain injury. J Neonatal-Perinat Med 13:449–458. https://doi.org/10.3233/NPM-190368
Sarnat HB (1976) Neonatal encephalopathy following fetal distress: a clinical and electroencephalographic study. Arch Neurol 33:696. https://doi.org/10.1001/archneur.1976.00500100030012
Shah PS, Seidlitz W, Chan P et al (2017) Internal audit of the Canadian Neonatal Network data collection system. Am J Perinatol 34:1241–1249. https://doi.org/10.1055/s-0037-1603325
Goswami IR, Whyte H, Wintermark P et al (2020) Characteristics and short-term outcomes of neonates with mild hypoxic-ischemic encephalopathy treated with hypothermia. J Perinatol Off J Calif Perinat Assoc 40:275–283. https://doi.org/10.1038/s41372-019-0551-2
Kellum JA, Lameire N, KDIGO AKI Guideline Work Group (2013) Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (Part 1). Crit Care Lond Engl 17:204. https://doi.org/10.1186/cc11454
CNN abstractor’s manual version 3.5.2 (2022) Available via GOOGLE. https://www.google.com/search?q=CNN+abstractor%27s+manual+version+3.5.2&rlz=1C1WERZ_enCA989CA989&oq=CNN+abstractor%27s+manual+version+3.5.2&aqs=chrome..69i57.13371j0j7&sourceid=chrome&ie=UTF-8. Accessed 8 Jun 2022
Statistics Canada: Canada’s national statistical agency. Available via GOOGLE. https://www.statcan.gc.ca/en/start. Accessed 21 Jan 2022
Du M, Yang J, Han N et al (2021) Association between the COVID-19 pandemic and the risk for adverse pregnancy outcomes: a cohort study. BMJ Open 11:e047900
Kumar M, Puri M, Yadav R et al (2021) Stillbirths and the COVID-19 pandemic: Looking beyond SARS-CoV-2 infection. Int J Gynecol Obstet 153:76–82. https://doi.org/10.1002/ijgo.13564
Kc A, Gurung R, Kinney MV et al (2020) Effect of the COVID-19 pandemic response on intrapartum care, stillbirth, and neonatal mortality outcomes in Nepal: a prospective observational study. Lancet Glob Health 8:e1273–e1281. https://doi.org/10.1016/S2214-109X(20)30345-4
Simpson AN, Snelgrove JW, Sutradhar R et al (2021) Perinatal outcomes during the COVID-19 pandemic in Ontario. Canada JAMA Netw Open 4:e2110104. https://doi.org/10.1001/jamanetworkopen.2021.10104
Glazier RH, Green ME, Wu FC et al (2021) Shifts in office and virtual primary care during the early COVID-19 pandemic in Ontario, Canada. Can Med Assoc J 193:E200–E210. https://doi.org/10.1503/cmaj.202303
Bhatia RS, Chu C, Pang A et al (2021) Virtual care use before and during the COVID-19 pandemic: a repeated cross-sectional study. CMAJ Open 9:E107–E114. https://doi.org/10.9778/cmajo.20200311
Acknowledgements
List of network investigators, CNN Site Investigators: Prakesh S Shah, MD, MSc (Director, Canadian Neonatal Network and Site Investigator), Mount Sinai Hospital, Toronto, Ontario; Marc Beltempo, MD, (Associate Director, Canadian Neonatal Network and Site Investigator), Montreal Children’s Hospital at McGill University Health Centre, Montréal, Québec; Jaideep Kanungo, MD, Victoria General Hospital, Victoria, British Columbia; Jonathan Wong, MD, British Columbia Women’s Hospital, Vancouver, British Columbia; Dr. Miroslav Stavel, MD, Royal Columbian Hospital, New Westminster, British Columbia; Rebecca Sherlock, MD, Surrey Memorial Hospital, Surrey, British Columbia; Ayman Abou Mehrem, MD, Foothills Medical Centre, Calgary, Alberta; Jennifer Toye, MD, and Joseph Ting, MD, Royal Alexandra Hospital, Edmonton, Alberta; Carlos Fajardo, MD, Alberta Children’s Hospital, Calgary, Alberta; Jaya Bodani, MD, Regina General Hospital, Regina, Saskatchewan; Lannae Strueby, MD, Jim Pattison Children’s Hospital , Saskatoon, Saskatchewan; Mary Seshia, MBChB, and Deepak Louis, MD, Winnipeg Health Sciences Centre, Winnipeg, Manitoba; Ruben Alvaro, MD, St. Boniface General Hospital, Winnipeg, Manitoba; Amit Mukerji, MD, Hamilton Health Sciences Centre, Hamilton, Ontario; Orlando Da Silva, MD, MSc, London Health Sciences Centre, London, Ontario; Sajit Augustine, MD, Windsor Regional Hospital, Windsor, Ontario; Kyong-Soon Lee, MD, MSc, Hospital for Sick Children, Toronto, Ontario; Eugene Ng, MD, Sunnybrook Health Sciences Centre, Toronto, Ontario; Brigitte Lemyre, MD, The Ottawa Hospital, Ottawa, Ontario; Thierry Daboval, MD, Children’s Hospital of Eastern Ontario, Ottawa, Ontario; Faiza Khurshid, MD, Kingston General Hospital, Kingston, Ontario; Victoria Bizgu, MD, Jewish General Hospital, Montréal, Québec; Keith Barrington, MBChB, Anie Lapointe, MD, and Guillaume Ethier, NNP, Hôpital Sainte-Justine, Montréal, Québec; Christine Drolet, MD, and Bruno Piedboeuf, MD, Centre Hospitalier Universitaire de Québec, Sainte Foy, Québec; Martine Claveau, MSc, LLM, NNP, Montreal Children’s Hospital at McGill University Health Centre, Montréal, Québec; Marie St-Hilaire, MD, Hôpital Maisonneuve-Rosemont, Montréal, Québec; Valerie Bertelle, MD, and Edith Masse, MD, Centre Hospitalier Universitaire de Sherbrooke, Sherbrooke, Québec; Dr. Hamid Mehdizadeh-Hakak, MD, Moncton Hospital, Moncton, New Brunswick; Hala Makary, MD, Dr. Everett Chalmers Hospital, Fredericton, New Brunswick; Cecil Ojah, MBBS, Saint John Regional Hospital, Saint John, New Brunswick; Dr. Jo-Anna Hudson, MD, Janeway Children’s Health and Rehabilitation Centre, St. John’s, Newfoundland; Jehier Afifi, MB BCh, MSc, IWK Health Centre, Halifax, Nova Scotia; Ameer Aslam, MD, Cape Breton Regional Hospital, Sydney, Nova Scotia; Shoo K Lee, MBBS, PhD (Chairman, Canadian Neonatal Network), Mount Sinai Hospital, Toronto, Ontario, CPTBN Site Investigators: Wendy Whittle, MD, Mount Sinai Hospital, Toronto, Ontario; Michelle Morais, MD, Hamilton Health Sciences Centre, Hamilton, Ontario; Kenneth Lim, MD, Children’s & Women’s Health Centre of BC, Vancouver, British Columbia; Darine El-Chaar, MD, Children’s Hospital of Eastern Ontario, Ottawa, Ontario; Katherine Theriault, MD, Centre Hospitalier Universitaire de Quebec, Sainte Foy, Québec; Marie-Ève Roy-Lacroix, MD, Centre Hospitalier Universitaire de Sherbrooke, Sherbrooke, Québec; Kimberly Butt, MD, Dr. Everett Chalmers Hospital, Fredericton, New Brunswick; Candace O’Quinn, MD, Foothills Medical Centre, Calgary, Alberta; Christy Pylypjuk, MD, Health Sciences Centre, Winnipeg, Manitoba; Isabelle Boucoiran, MSc, MD, Hôpital Sainte-Justine, Montréal, Québec; Catherine Taillefer, MD, Hôpital Sainte-Justine, Montréal, Québec; Joan Crane, MD, Janeway Children’s Health and Rehabilitation Centre, St. John’s, Newfoundland; Haim Abenhaim, MD, Jewish General Hospital, Montréal, Québec; Graeme Smith, MD, Kingston General Hospital, Kingston, Ontario; Karen Wou, MDCM, McGill University Health Centre, Montréal, Québec; Sue Chandra, MD, Royal Alexandra Hospital/Stollery Children’s Hospital, Edmonton, Alberta; Jagdeep Ubhi, MD, Royal Columbian Hospital, New Westminster, British Columbia; George Carson, MD, Regina General Hospital, Regina, Saskatchewan; Michael Helewa, MD, St. Boniface General Hospital, Winnipeg, Manitoba; Ariadna Grigoriu, MD, The Moncton Hospital, Moncton, New Brunswick; Rob Gratton, MD, London Health Sciences Centre, London, Ontario; Cynthia Chan, MD, London Health Sciences Centre, London, Ontario; James Andrews, MD, Saint John Regional Hospital, St. John, New Brunswick; Naila Ramji, MD, Saint John Regional Hospital, St. John, New Brunswick; Nir Melamed, MD, Sunnybrook Health Sciences Centre, Toronto, Ontario; Jason Burrows, MD, Surrey Memorial Hospital, Surrey, British Columbia; Sajit Augustine, MD, Windsor Regional Hospital, Windsor, Ontario; Lara Wesson, MD, Royal University Hospital, Saskatoon, Saskatchewan; Erin MacLellan, MD, Cape Breton Regional Hospital, Sydney, Nova Scotia; Hayley Bos, MD, Victoria General Hospital, Victoria, British Columbia; Victoria Allen, MD, IWK Health Centre, Halifax, Nova Scotia.
Funding
Although no specific funding was received for this study, organizational support for the Canadian Neonatal Network, Canadian Preterm Birth Network, and the Canadian Neonatal Follow-Up Network was provided by the Maternal-infant Care Research Centre (MiCare) at Mount Sinai Hospital in Toronto, Ontario, Canada. MiCare is supported by a Canadian Institutes of Health Research (CIHR) Team Grant (CTP 87518) and the participating hospitals.
Author information
Authors and Affiliations
Consortia
Contributions
Khorshid Mohammad, Sujith Kumar Reddy Gurram Venkata, Marc Beltempo, and Prakesh S Shah contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Marc Beltempo. The first draft of the manuscript was written by Sujith Kumar Reddy Gurram Venkata and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and patient consent
The University of Calgary Conjoint Health Research Ethics Board approved the project and waved the need for parental consent (REB21-0497).
Disclaimer
The funding bodies played no role in the design and conduct of the study; the collection, management, analysis, or interpretation of the data; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gurram Venkata, S.K.R., Shah, P.S., Beltempo, M. et al. Outcomes of infants with hypoxic-ischemic encephalopathy during COVID-19 pandemic lockdown in Canada: a cohort study. Childs Nerv Syst 38, 1727–1734 (2022). https://doi.org/10.1007/s00381-022-05575-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-022-05575-8