Abstract
Purpose
The purpose of this study was to define, in children following head trauma and GSC ≤ 8, at which level of intracranial pressure (ICP), the thermodilutional, and gas analytic parameters implicated in secondary cerebral insults shows initial changes.
Methods
We enrolled in the study 56 patients: 30 males and 26 females, mean age 71 ± 52 months. In all children, volumetric hemodynamic and blood gas parameters were monitored following initial resuscitation and every 4 h thereafter or whenever a hemodynamic deterioration was suspected. During the cumulative hospital stay, a total of 1050 sets of measurements were done. All parameters were stratified in seven groups according to ICP (group A1 = 0–5 mmHg, group A2 = 6–10 mmHg, group A3 = 11–15 mmHg, group A4 16–20 mmHg, group A5 21–25 mmHg, group A6 26–30 mmHg, group A7 >31 mmHg).
Results
Mean values of jugular oxygen saturation (SJO2), jugular oxygen partial pressure (PJO2), extravascular lung water (EVLWi), pulmonary vascular permeability (PVPi), fluid overload (FO), and cerebral extraction of oxygen (CEO2) vary significantly from A3 (11–15 mmHg) to A4 (16–20 mmHg). They relate to ICP in a four-parameter sigmoidal function (4PS function with: r 2 = 0.90), inflection point of 15 mmHg of ICP, and a maximum curvature point on the left horizontal asymptote at 13 mmHg of ICP.
Conclusions
Mean values of SJO2, PJO2, EVLWi, PVPi, FO, and CEO2 become pathologic at 15 mmHg of ICP; however, the curve turns steeper at 13 mmHg, possibly a warning level in children for the development of post head trauma secondary insult.
Similar content being viewed by others
Introduction
Head trauma is the main cause of death or permanent disability in children between 1 and 19 years of age [1–3]. Secondary cerebral insults derive from increased intracranial pressure (ICP) [4, 5] and reduced cerebral blood flow (CBF) [6] and ischemia. Prevention of secondary insults is a most relevant target in the treatment of head trauma patients in the intensive care units [7–9]. ICP monitoring and calculation of cerebral perfusion pressure (CPP) are instrumental to guide the treatment [10, 11] and possibly are prognostic predictors [7, 12]. Although ICP and CPP [13] are commonly considered of equal reliability, ICP as a guide to treatment has been credited of better patient outcomes [14]. The therapeutic measures for ICP control can have relevant side effect, and continuous monitoring is therefore necessary [15]. The interpretation of the levels of ICP in children is made difficult by the fact that in children, the pressure-volume index [16] and the auto regulatory curve functions [17] have age-related differences. Furthermore, some authors have found that the relation between ICP and partial pressure of brain tissue oxygen (PbtO2) is weak, as it is influenced by a large number of variables [18]. No ICP threshold predictive of brain hypoxia has been identified so far in children. Based on the observation that ICP >20 mmHg is associated with a poor prognosis, most authors consider this level the threshold to start treatment of pediatric head trauma [7, 19–21]. A few do consider pathologic pressures between 15 and 20 mmHg but stratify them by age [22].
Hemodynamic surveillance in children with severe head trauma was done monitoring ICP, blood gas, and thermodilutional parameters. The thermodilution method for hemodynamic monitoring is particularly appealing for use in pediatrics, sparing pulmonary artery catheterization that carries significant risks [23]. With thermodilution, one can measure global end diastolic volume (used as preload index), stroke volume, systemic vascular resistances, extravascular lung water, and pulmonary permeability, opening new diagnostic and therapeutic perspectives [24].
In this study, we investigate if there is an ICP threshold for significant blood gas parameters and thermodilutional parameter changes after a severe traumatic head injury and GCS ≤8.
Materials and methods
We considered for enrollment in the study 68 children with a diagnosis of traumatic head injury and GCS ≤8 admitted to the Pediatric Intensive Care Unit of Ospedale Bambino Gesù between June 2009 and October 2013. Fifty-six were actually entered and 12 were excluded because of congenital or acquired heart diseases or intracardiac shunts; abnormal coagulation profile contraindicating femoral artery catheterization; chronic and acute respiratory diseases (pneumonia, bronchopneumonia, pleural effusion); neurologic diseases; renal insufficiency; multiple trauma; and diabetes insipidus either primary or secondary to head trauma and multiple trauma.
Informed consent was obtained from both parents of each child on admission to ICU and again at the end of the study. The protocol conforms to the guidelines of the Declaration of Helsinki and was approved by the ethical committee of the involved institution [25].
Model of the study
Following initial resuscitation and stabilization, hemodynamics by thermodilution was started within 60 min from admission. Measurements of thermodilutional parameters were done at 4-h intervals and additional readings were obtained whenever hemodynamics appeared to worsen. Each thermodilutional measurement is expressed as the mean value of three consecutive readings. The monitoring of hemodynamic parameters ended when the child was weaned from the ventilator or died. The same time schedule was applied to blood gas analysis and ICP. Invasive monitoring of ICP lasted nearly 96 h; then the intracranial catheter was removed. Also, the catheters in the internal jugular vein were removed within 96 h from their placement.
Patients’ care
Hemodynamics was monitored in all patients on a continuous basis, and all were intubated and mechanically ventilated. The target PaO2 was 80 mmHg, and the initial PEEP level never exceeded 5 cm H2O. Arterial PaCO2 levels were maintained with a target ≈35 mmHg, independently of airway pressures. Ventilator setting was optimized according to blood gas analysis results. All patients were sedated with continuous infusion of midazolam 0.1 mg/kg/h and fentanyl 3 μg/kg/h, according to COMFORT score obtained every 2 h by nurses. A neuromuscular blockade with vecuronium (0.1 mg/kg) was performed with the dose titrated by twitch response to stimulation
During the study, respiratory and hemodynamic functions were maintained stable in all patients with inotropic support (dopamine >5 μg/kg/min or norepinephrine >0.03 μg/kg/min and/or dobutamine >5 μg/kg/min), the goal being to maintain an average cardiac index >3.0 l/min/m2, with a ICP ≤15 mmHg and a cerebral perfusion pressure (CPP) ≥60 mmHg.
Stepwise escalations of care were implemented via a protocol, based on the “Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents—second edition” [26], and included sedation (with fentanyl), neuromuscular blockade (with vecuronium), mild hyperventilation (PaCO2 ≈ 35 mmHg), hyperosmolar therapies (mannitol or 3 % NaCl), barbiturate administration, and decompressive craniotomy for intracranial hypertension refractory to medical management.
Monitoring
Thermodilution method for hemodynamic monitoring
Hemodynamic monitoring was obtained placing a thermodiluition catheter in the femoral artery (Pulsiocath Arterial Thermodilution Catheter, Pulsion Medical Systems, Munich, Germany using a 3F catheter when weight was <10 kg and a 4F catheter for weights ≥10 kg) and a central venous line into an internal jugular or subclavian vein (Arrow Bilumen 5–7 French). A bolus of 0.15 ml/kg + 1.5 ml ice-cold saline solution is injected into a central vein, random to respiratory cycle, and a thermistor on the tip of the femoral arterial catheter measures the downstream temperature changes. Using a commercially available device (PiCCO; Pulsion Medical System, Munich, Germany), thermodilutional parameters were estimated or calculated according with the methods previously reported [27]. Estimation or calculation included cardiac output (CO = l/min), extravascular lung water (EVLW = ml), global end diastolic volume (GEDV = ml), pulmonary blood volume (PBV = ml), pulmonary vascular permeability (PVP) as EVLW/PBV ratio, cardiac function index (CFi) as CO/GEDV ratio (per minute), and systemic vascular resistance (SVR, dyn·s·cm−5). All parameters were indexed (i) for body surface area (BSA) (Ci = CO/BSA, GEDVi = GEDV/BSA, PBVi = PBV/BSA, SVRi = SVR/BSA) or body weight (EVLWi = EVLW/body weight).
Cerebral oxygenation
All patients were subjected to intermittent jugular bulb venous blood sampling for oxygen saturation (SJO2) and oxygen partial pressure (PJO2) monitoring. For this purpose, ultrasound-guided retrograde catheterization of the internal jugular vein was performed. All catheters were removed within 96 h from their placement. At the time of each SJO2 and PJO2 assessment, we did also a blood gas analysis for PaO2 and SaO2, and calculated the cerebral extraction of oxygen (CEO2) as the difference between SaO2 and SJO2.
Intracranial pressure (ICP mmHg) monitoring
For ICP monitoring, a Codman microsensor ICP transducer is inserted as to provide measurements of intracranial pressure at the parenchymal level. Information is relayed electronically rather than through a hydrostatic column or fiber optics. The catheter is removed after 96 h.
Fluid overload monitoring
Percent fluid overload (FO) is calculated using the formula %FO = (total fluid intake − total fluid output) [l]/body weight [kg] × 100. We entered the lowest weight registered during the month prior to admission.
Objectives of the study
-
Primary goals were the following:
-
Assess which parameters, SJO2, PJO2, EVLWi, PVPi, Ci, SVRi, CFi, CEO2, PaO2, FO, SaO2, mean arterial pressure (MAP), and PaCO2, could be related to ICP and/or time of recording
-
Determine whether critical ICP thresholds for changes in parameters could be defined; to this aim, the parameters under scrutiny were also pooled in 7 groups according to ICP increments of 5 mmHg (group A1 = 0–5 mmHg—5 patients, group A2 = 6–10 mmHg—11 patients, group A3 = 11–15 mmHg—19 patients, group A4 16–20 mmHg—5 patients, group A5 21–25 mmHg—6 patients, group A6 26–30 mmHg—5 patients, group A7 >31 mmHg—5 patients)
-
-
Secondary goals were the following:
-
Determine if all the parameters under scrutiny that correlate
swith ICP can be linked in one single equation -
Ascertain if it can be identified a definite ICP threshold for significant blood gas parameters and thermodilutional parameters changes after a severe traumatic head injury with GCS ≤8 in children
-
Measure also at the end of observation the mean value of intracranial pressure in deceased and recovered patients
-
Statistics
For statistical analysis, we relied on JMP® 10.0.1 program for Mac by SAS Institute, Inc.
For all the parameters considered in the study, the approximation to normal of the distribution of the population was tested by Kolmogorov-Smirnov one-sample test and statistics for kurtosis and symmetry. As results were asymmetrically distributed, nonparametric tests were used. Data are expressed as mean ± standard deviation. We used the Kruskal-Wallis nonparametric one-way analysis of variance to examine the changes of each parameter between the subgroups; the null hypothesis was that the groups for the same parameter all came from the same distribution. After, the mean values of all the groups of the parameters considered in the study were compared using the non-parametric test of Wilcoxon.
A p < 0.05 was considered significant.
In evaluating the importance of the variable time in the analysis of the monitored parameters, we studied the dependency between ICP and the other parameters at the different times of recording. To this purpose, we used a generalized linear model (GLM) considering the times of recording as categorical predictor, ICP as continuous predictor, and the other parameters under scrutiny as response variable.
We did a principal component analysis to assess which among the monitored parameters are interrelated and thus select the ones significantly related with ICP changes. With the principal component analysis, we then studied if and how all the parameters with a significant relation to ICP allowed us to express an index variable (F1) summarizing the contemporary variations of all the parameters with changing values of ICP. The analysis of the system will also define by what percentage the F1 index variable expresses the overall variations of the monitored parameters.
The F1 index variable thus identified is used in a four-parameter sigmoidal (4PS) function generalized nonlinear regression model of response to ICP changes. In this model, we obtain a visual representation of the relation between ICP and F1, that is the relation between ICP and the changes of all the parameters considered, the ones that at the previous analyses had been found related to ICP. This is in itself a generalized model with logistic link, represented in the form of a sigmoid curve.
We computed the point of maximal curvature on the left horizontal asymptote and the inflection point. The point of maximal curvature is the point on the left asymptote where the parameter under scrutiny starts to detach from horizontal asymptote. The inflection point is defined as the point on the curve where the curve changes from concave upwards to concave downwards.
Results
Out of the total 68 children, 12 were excluded: 7 because of multiple trauma, 3 because of intercurrent nosocomial pneumonia, and 2 because of the onset of acute renal failure. The population of the study (Table 1) was formed with 56 patients: 30 males and 26 females, mean age 73 ± 27 months (lower 95 % mean = 65.82; upper 95 % mean = 80.17). Their diagnoses were epidural hematoma (16 cases), subdural hematoma and subarachnoid hemorrhage (4 cases), concussion and axonal damage (8 cases), axonal damage (4 cases), subarachnoid hemorrhage and axonal damage (4 cases), subarachnoid hemorrhage and intraventricular brain hemorrhage (4 cases), intracranial hypertension and loss of cerebral tissue (4 cases), intracranial hypertension and cerebral edema (8 cases), and concussion and subdural hemorrhage (4 cases). Fifteen patients died while in the hospital (13 of malignant intracranial hypertension and cerebral edema, 2 of sepsis). A total of 1050 sets of measurements were done equal to 18.44 ± 4.85 sets of measurements/child (upper 95 % mean = 19.75; lower 95 % mean 17.15).
With the GLM, we found that some of the monitored parameters changed as a function of ICP (SJO2, PJO2, EVLWi, PVPi, CEO2, and FO; p < 0.05), but not as a function of timing of recording (p = NS), while the others does not change both in function of the time of recording and the ICP.
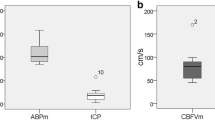
As shown in Fig. 1, pooling the values of SJO2, PJO2, EVLWi, PVPi, Ci, SVRi, CFi, CEO2, PaO2, FO, SaO2, MAP, and PaCO2 according to ICP, statistically significant changes are detectable for the mean value of SJO2, PJO2, EVLWi, PVPi, FO, and CEO2 between groups A3 (ICP = 11–15 mmHg) and A4 (ICP = 16–20 mmHg): SJO2 (69.94 ± 10.09 vs. 80.40 ± 3.94; p < 0.033), PJO2 (33.11 ± 4.77 vs. 41.77 ± 4.99; p < 0.007), EVLWi (7.00 ± 0.86 vs. 10.88 ± 1.46; p < 0.0001), PVPi (4.88 ± 0.61 vs. 7.01 ± 0.97; p < 0.0006), FO (0.95 ± 0.11 vs. 1.45 ± 0.19; p < 0.0001), and CEO2 (28.87 ± 10.22 vs. 15.48 ± 8.85; p < 0.0217).
The analysis of the correlations with the statistical method for principal components (Fig. 2a) for PaO2, SaO2, PJO2, SJO2, MAP, ICP, Ci, EVLWi, FO, SVRi, CFi, PVPi, CEO2, and PaCO2 shows a significant correlation between ICP and EVLWi (r = 0.56), FO (r = 0.55), PJO2 (r = 0.62), SJO2 (r = 0.49), PVPi (r = 0.64), and CEO2 (r = −0.43).
Principal components analysis. a Correlations of the parameters of the study with ICP and principal components analysis of the parameters significantly related to ICP b with indicator of the entire system (F1) determination. Figure 2 describes the structure of the linear correlations between the parameters under study. The position of the dots in the four quadrants of the circle is indicative of the intensity of the correlations. Reading directions: (1) Two dots in the same quadrant, near to each other, in close proximity with the y-axis and distant from the origin have a strong positive correlation. (2) Two dots falling in opposite quadrants but near to the y-axis and far from the origin have a strong negative correlation. (3) Dots of the variables falling next to the origin point indicate low correlation between those variables and with all of the others. (4) Dots of the variables scattered and far from the origin of the axes have middle range correlation. Therefore, F1 is a synthetic indicator of a system of linear relations able to explain 70 % of the overall variability of the system of physiological variables PJO2, SJO2, EVLWI, PVPI, CEO2, and FO
Subsequent analysis for principal components between parameters significantly related with ICP explains nearly 70.3 % of the global variability of the system (Fig. 2b).
As shown in Fig. 3, four-parameter sigmoidal (4PS) function of response to ICP changes of all these parameters is characterized by a nonlinear regression with r 2 correlation = 0.90, a maximal curvature point on the left horizontal asymptote at 13 mmHg of ICP, and an inflection point at 15 mmHg of ICP.
Four-parameter sigmoidal (4PS) function generalized nonlinear regression model for the calculation of the existing relation between ICP and SJO2, PJO2, EVLWi, PVPi, FO, and CEO2 and with indication of inflection point and maximum curvature point on the left asymptote. The red line in the figure represents the course of F1 with changing values of ICP. Keeping in mind what F1 represents, the line epitomizes the overall course of PJO2, SjO2, EVLWI, PVPI, CEO2, and FO at ICP changes. This model shows a coefficient of correlation r = 0.90 (correlation between F1 values observed and F1 values expected from the equation). In the graph, the F1 indicator shows that the system is stable until ICP approximates 13 mmHg (maximum curvature point). Above this level, the system becomes unstable and the inflection point is reached at about 15 mmHg
Also, the model of comparison 4PS function for each of the six related parameters shows a maximal curvature point (MCP) on the left horizontal asymptote of ICP and an inflection point (IP) very near to each other and similar to the curve in Fig. 3: SJO2 (MCP = 12.88 and IP = 15.40 mmHg), PJO2 (MCP = 12.70 and IP = 15.16 mmHg), EVLWi (MCP = 12.81 and IP = 15.36 mmHg), PVPi (MCP = 12.82 and IP = 15.52 mmHg), FO (MCP = 13.11 and IP = 15.26 mmHg), and CEO2 (MCP = 12.90 and IP = 15.25 mmHg).
Mean values of ICP at the end of observation are significantly higher in the group of the deceased (12.50 ± 1.40 vs. 24.47 ± 2.45 mmHg; p < 0.0001).
Discussion
In our study, the GLM shows that we found that some of the monitored parameters changed as a function of ICP (SJO2, PJO2, EVLWi, PVPi, CEO2, and FO), but not as a function of timing of recording. As the temporal relation has no statistical significance, we did not consider it any further, while we did analyze the relation between ICP and the related monitored parameters.
According to our data, stratifying the behavior of thermodilutional and blood gas parameters on ICP changes (Fig. 1) the most abrupt changes of SJO2, PJO2, EVLWi, PVPi, FO, and CEO2 are observed when ICP increases from 11–15 mmHg to 16–20 mmHg (group A3 vs. group A4).
The same parameters show a significant correlation with ICP both taken as a group (Fig. 3) or examined singularly, pointing to a correlation between ICP and brain tissue oxygenation (Fig. 2), while no correlation is found between brain tissue oxygenation, PaO2, and SaO2. This is in accordance with the report by Figaji et al. in children [28]. However, other authors found no correlation between brain tissue oxygenation, hemodynamics and cerebral pressures [29, 30].
We do not found a correlation between the PaCO2 and ICP levels. The most likely explanation is that the mechanical ventilator setting was constantly adjusted to maintain PaCO2 at about 35 mmHg, altering the possible related change.
The straight line relating ICP with the parameters under scrutiny (SJO2, PJO2, EVLWi, PVPi, FO, and CEO2) analyzed with type 4PS function both singularly and as a group (Fig. 3), consistently shows an inflection point at about 15 mmHg. This 15 mmHg level seems critical as it is accompanied by a decrease in oxygen consumption by the brain cells, an increase SJO2, and PJO2 and a decrease in CEO2. Fifteen mmHg could be the threshold of the secondary brain damage in head injury. Evidence which is in agreement with the report by Cruz et al. [5] that describes hyperoxic uncoupling between global cerebral consumption of oxygen and cerebral blood flow at the same 15 mmHg ICP levels.
At a more accurate analysis of the correlation curve of ICP with the group of parameters considered (Fig. 3), one observes that the curve changes from its horizontal when ICP reaches the level of 13 mmHg (maximal curvature point on the left horizontal asymptote, of Fig. 3) and after a steep climb, it inverts its concavity at an inflection point corresponding to ICP around 15 mmHg. The equation of the curve (Fig. 3) that explains nearly 70.3 % of the global variability of the system is characterized by a high statistical significance (r 2 = 0.90), and it is an interesting mathematical model predictive of the existing relation between ICP and the bulk of SJO2, PJO2, EVLWi, PVPi, FO, and CEO2 as well as each parameter singularly taken. Therefore, it appears that in children with severe head trauma (GCS <8) already when ICP reaches 13 mmHg, one should institute a therapy adequate to prevent further. Hyperventilation, hyperosmolar therapy, diuretics, fluid restriction, cerebrospinal fluid drainage, barbiturate, corticosteroids, decompressive craniotomy, analgesics, sedatives, and neuromuscular blockade are part of the armamentarium presently available, although with wide differences of clinical evidence [26].
The correlation between ICP and EVLWi accounts for the described development of neurogenic pulmonary edema in children after head trauma at a threshold value of 15 mmHg [31].
At the end of observation, ICP levels were significantly higher in the group of the deceased (12.50 ± 1.40 vs. 24.47 ± 2.45 mmHg, p < 0.0001). This is in agreement with the findings by other authors that an increasing ICP heralds a worse prognosis [32, 33].
Conclusions
In conclusion, our results show that in children aged 71 ± 52 months, oxygen consumption by brain cells is already reduced when ICP reaches the threshold of 15 mmHg. However, a more careful surveillance should better be instituted earlier, i.e., when ICP ≥13 mmHg, because ICP of 15 mmHg or greater is associated with risk of secondary brain injury. In fact, from ICP ≥13 mmHg, the line representing SJO2, PJO2, EVLWi, PVPi, FO, and CEO2 on a graph abandons the horizontal course starting to climb, although still without clinical manifestations.
References
Heron M, Sutton PD, Xu J, Ventura SJ, Strobino DM, Guyer B (2010) Annual summary of vital statistics: 2007. Pediatrics 125:4–15
Keenan HT, Bratton SL (2006) Epidemiology and outcomes of pediatric traumatic brain injury. Dev Neurosci 28:256–263
Langlois JA, Rutland-Brown W, Wald MM (2006) The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil 21:375–378
Barzilay Z, Augarten A, Sagy M, Shahar E, Yahav Y, Boichis H (1988) Variables affecting outcome from severe brain injury in children. Intensive Care Med 14:417–421
Cruz J, Nakayama P, Imamura JH, Rosenfeld KG, de Souza HS, Giorgetti GV (2002) Cerebral extraction of oxygen and intracranial hypertension in severe, acute, pediatric brain trauma: preliminary novel management strategies. Neurosurgery 50:774–777
Andrews PJ, Citerio G (2004) Intracranial pressure. Part one: historical overview and basic concepts. Intensive Care Med 30:1730–1733
Kochanek PM, Carney N, Adelson PD Ashwal S, Bell MJ, Bratton S, Carson S, Chesnut RM, Ghajar J, Goldstein B, Grant GA, Kissoon N, Peterson K, Selden NR, Tasker RC, Tong KA, Vavilala MS, Wainwright MS, Warden CR, American Academy of Pediatrics-Section on Neurological Surgery, American Association of Neurological Surgeons/Congress of Neurological Surgeons; Child Neurology Society, European Society of Pediatric and Neonatal Intensive Care, Neurocritical Care Society, Pediatric Neurocritical Care Research Group, Society of Critical Care Medicine, Paediatric Intensive Care Society UK, Society for Neuroscience in Anesthesiology and Critical Care, World Federation of Pediatric Intensive and Critical Care Societies (2012) Guidelines for the acute medical management of severe traumatic brain injury in infant, children and adolescents—second edition. Pediatr Crit Care Med 13:S1–S82
Tang ME, Lobel DA (2009) Severe traumatic brain injury: maximizing outcomes. Mt Sinai J Med 76:119–128
Elf K, Nilsson P, Enblad P (2002) Outcome after traumatic brain injury improved by an organized secondary insult program and standardized neurointensive care. Crit Care Med 30:2129–2134
Alali AS, Fowler RA, Mainprize TG, Scales DC, Kiss A, de Mestral C, Ray JG, Nathens AB (2013) Intracranial pressure monitoring in severe traumatic brain injury: results from the American College of Surgeons Trauma Quality Improvement Program. J Neurotrauma 30:1–10
Talving P, Karamanos E, Teixeira PG, Skiada D, Lam L, Belzberg H, Inaba K, Demetriades D (2013) Intracranial pressure monitoring in severe head injury: compliance with brain trauma foundation guidelines and effect on outcomes: a prospective study. J Neurosurg 119:1248–1254
White JR, Farukhi Z, Bull C, Christensen J, Gordon T, Paidas C, Nichols DG (2001) Predictors of outcome in severely head-injured children. Crit Care Med 29:534–540
Prabhakaran P, Reddy AT, Oakes WJ, King WD, Winkler MK, Givens TG (2004) A pilot trial comparing cerebral perfusion pressure-targeted therapy to intracranial pressure-targeted therapy in children with severe traumatic brain injury. J Neurosurg 100:454–459
Bennett TD, Riva-Cambrin J, Keenan HT, Korgenski EK, Bratton SL (2012) Variation in intracranial pressure monitoring and outcomes in pediatric traumatic brain injury. Arch Pediatr Adolesc Med 166:641–647
Steiner LA, Andrews PJD (2006) Monitoring the injured brain: ICP and CBF. Br J Anesth 97:26–38
Shapiro K, Marmarou A (1982) Clinical applications of the pressure—volume index in treatment of pediatric head injuries. J Neurosurg 56:819–825
Udomphorn Y, Armstead WM, Vavilala MS (2008) Cerebral blood flow and autoregulation after pediatric traumatic brain injury. Pediatr Neurol 38:225–234
Rohlwink UK, Zwane E, Fieggen AG, Argent AC, le Roux PD, Figaji AA (2012) The relationship between intracranial pressure and brain oxygenation in children with severe traumatic brain injury. Neurosurgery 70:1220–1231
Morris KP, Forsyth RJ, Parslow RC, Tasker RC, Hawley CA, UK Paediatric Traumatic Brain Injury Study Group, Paediatric Intensive Care Society Study Group (2006) Intracranial pressure complicating severe traumatic brain injury in children: monitoring and management. Intensive Care Med 32:1606–1612
Adelson PD, Bratton SL, Carney NA, Chesnut RM, du Coudray HE, Goldstein B, Kochanek PM, Miller HC, Partington MD, Selden NR, Warden CR, Wright DW, American Association for Surgery of Trauma, Child Neurology Society; International Society for Pediatric Neurosurgery, International Trauma Anesthesia and Critical Care Society, Society of Critical Care Medicine, World Federation of Pediatric Intensive and Critical Care Societies (2003) Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents. Chapter 5. Indications for intracranial pressure monitoring in pediatric patients with severe traumatic brain injury. Pediatr Crit Care Med 4(Suppl 3):S19–S24
Adelson PD, Bratton SL, Carney NA, Chesnut RM, du Coudray HE, Goldstein B, Kochanek PM, Miller HC, Partington MD, Selden NR, Warden CR, Wright DW, American Association for Surgery of Trauma, Child Neurology Society, International Society for Pediatric Neurosurgery, International Trauma Anesthesia and Critical Care Society, Society of Critical Care Medicine, World Federation of Pediatric Intensive and Critical Care Societies (2003) Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents. Chapter 6. Threshold for treatment of intracranial hypertension. Pediatr Crit Care Med 4(Suppl 3):S25–S27
Mazzola CA, Adelson PD (2002) Critical care management of head trauma in children. Crit Care Med 30:S393–S401
Pauli C, Falker U, Genz T, Hennig M, Lorenz HP, Hess J (2002) Cardiac output determination in children: equivalence of the transpulmonary thermodilution method to the direct Fick principle. Intensive Care Med 28:947–952
Cecchetti C, Lubrano R, Cristaldi S, Stoppa F, Barbieri MA, Elli M, Masciangelo R, Perrotta D, Travasso E, Raggi C, Marano M, Pirozzi N (2008) Relationship between global end-diastolic volume and cardiac output in critically ill infants and children. Crit Care Med 36:928–932
World Medical Association (2000) Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 284:3043–3045
Carney NA, Chesnut R, Kochanek PM, American Association for Surgery of Trauma, Child Neurology Society, International Society for Pediatric Neurosurgery, International Trauma Anesthesia and Critical Care Society, Society of Critical Care Medicine, World Federation of Pediatric Intensive and Critical Care Societies (2012) Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents—second edition. Pediatr Crit Care Med 13:S1–S82
Lubrano R, Cecchetti C, Elli M, Tomasello C, Guido G, Di Nardo M, Masciangelo R, Pasotti E, Barbieri MA, Bellelli E, Pirozzi N (2011) Prognostic value of extravascular lung water index in critically ill children with acute respiratory failure. Intensive Care Med 37:124–131
Figaji AA, Zwane E, Fieggen AG, Argent AC, Le Roux PD, Siesjo P, Peter JC (2009) Pressure autoregulation, intracranial pressure, and brain tissue oxygenation in children with severe traumatic brain injury. J Neurosurg Pediatr 4:40020–400280
Eriksson EA, Barletta JF, Figueroa BE, Bonnell BW, Vanderkolk WE, McAllen KJ, Ott MM (2012) Cerebral perfusion pressure and intracranial pressure are not surrogates for brain tissue oxygenation in traumatic brain injury. Clin Neurophysiol 123:1255–1260
Figaji AA, Zwane E, Thompson C, Fieggen AG, Argent AC, Le Roux PD, Peter JC (2009) Brain tissue oxygen tension monitoring in pediatric severe traumatic brain injury. Part 1: relationship with outcome. Childs Nerv Syst 25:1325–1333
Cecchetti C, Elli M, Stoppa F, Di Nardo M, Pasotti E, Gentile I, Paoli S, Pirozzi N, Lubrano R (2013) Neurogenic pulmonary edema and variations of hemodynamic volumetric parameters in children following head trauma. Minerva Anestesiol 79:1140–1146
Jagannathan J, Okonkwo DO, Yeoh HK, Dumont AS, Saulle D, Haizlip J, Barth JT, Jane JA Sr, Jane JA Jr (2008) Long-term outcomes and prognostic factors in pediatric patients with severe traumatic brain injury and elevated intracranial pressure. J Neurosurg Pediatr 2:240–249
Allen BB, Chiu YL, Gerber LM, Ghajar J, Greenfield JP (2014) Age-specific cerebral perfusion pressure thresholds and survival in children and adolescents with severe traumatic brain injury. Pediatr Crit Care Med 15:62–70
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lubrano, R., Elli, M., Stoppa, F. et al. Variations of the blood gas levels and thermodilutional parameters during ICP monitoring after severe head trauma in children. Childs Nerv Syst 31, 1273–1281 (2015). https://doi.org/10.1007/s00381-015-2700-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-015-2700-z