Abstract
Purpose
The aim was to compare the effects of propofol and desflurane anesthesia on transcranial motor evoked potentials (MEPs) from pediatric patients undergoing surgery for spinal deformities.
Methods
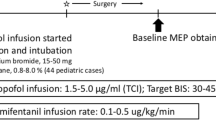
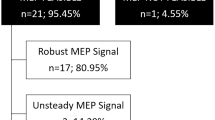
Desflurane and propofol cohorts (25 patients each) were obtained retrospectively and matched for patient characteristics and surgical approach. MEPs from the thenar eminence and abductor hallucis were compared during maintenance anesthesia on desflurane (0.6–0.8 MAC) or propofol infusion (150–300 μg/kg/min). MEP amplitudes and durations were obtained for successive 30-min intervals for 150 min, beginning 60 min after maintenance anesthesia.
Results
Mean peak to peak amplitudes of MEPs under desflurane anesthesia from the thenar eminence (419 μV) and abductor hallucis (386 μv) were not significantly different from those under propofol (608 μV, 343 μV, thenar, and abductor hallucis, respectively). Stimulation was greater by 42 V and 136 mA, and trains were slightly longer in the desflurane compared to the propofol group (p < 0.05). Most MEP amplitudes for the desflurane and propofol cohorts remained the same or increased (71 % of cases) when those after 150 min were compared to those in the first 30-min interval.
Conclusions
MEPs with good amplitudes were obtained under desflurane only anesthesia that were comparable to propofol only anesthesia in pediatric patients during surgery for spinal deformities. There was no evidence for anesthetic fade over the time period examined. When used by itself, desflurane can be considered a viable alternative to propofol anesthesia.



Similar content being viewed by others
References
Chen Z (2004) The effects of isoflurane and propofol on intraoperative neurophysiological monitoring during spinal surgery. J Clin Monit Comput 18:303–308
Clapcich AJ, Emerson RG, Roye DP et al (2004) The effects of propofol, small-dose isoflurane, and nitrous oxide on cortical somatosensory evoked potential and bispectral index monitoring in adolescents undergoing spinal fusion. Anesth Analg 99:1334–1340
Deiner SG, Kwatra SG, Lin H, Weisz DJ (2010) Patient characteristics and anesthetic technique are additive but not synergistic predictors of successful motor evoked potential monitoring. Anesth Analg 111:421–426
Jellinek D, Platt M, Jewkes D, Symon L (1991) Effects of nitrous oxide on motor evoked potentials recorded from skeletal muscle in patients under total anesthesia with intravenously administered propofol. Neurosurgery 29:558–562
Kunisawa T, Nagata O, Nomura M, Iwasaki H, Ozaki M (2004) A comparison of the absolute amplitude of motor evoked potentials among groups of patients with various concentrations of nitrous oxide. J Anesth 18:181–184
Lieberman JA, Lyon R, Feiner J, Diab M, Gregory GA (2006) The effect of age on motor evoked potentials in children under propofol/isoflurane anesthesia. Anesth Analg 103:316–321
Liu HY, Zeng HY, Cheng H, Wang MR, Qiao H, Han RQ (2012) Comparison of the effects of etomidate and propofol combined with remifentanil and guided by comparable BIS on transcranial electrical motor-evoked potentials during spinal surgery. J Neurosurg Anesthesiol 24:133–138
Lo YL, Dan YF, Tan YE, Nurjannah S, Tan SB, Tan CT, Raman S (2004) Intra-operative monitoring in scoliosis surgery with multi-pulse cortical stimuli and desflurane anesthesia. Spinal Cord 42:342–345
Lo YL, Dan YF, Tan YE, Nurjannah S, Tan SB, Tan CT, Raman S (2006) Intraoperative motor-evoked potential monitoring in scoliosis surgery: comparison of desflurane/nitrous oxide with propofol total intravenous anesthetic regimens. J Neurosurg Anesthesiol 18:211–214
Lyon R, Feiner J, Lieberman JA (2005) Progressive suppression of motor evoked potentials during general anesthesia: the phenomenon of "anesthetic fade". J Neurosurg Anesthesiol 17:13–19
Macdonald DB, Skinner S, Shils J, Yingling C (2013) Intraoperative motor evoked potential monitoring—a position statement by the American Society of Neurophysiological Monitoring. Clin Neurophysiol 124:2291–2316
Nathan N, Tabaraud F, Lacroix F, Mouliès D, Viviand X, Lansade A, Terrier G, Feiss P (2003) Influence of propofol concentrations on multipulse transcranial motor evoked potentials. Br J Anaesth 91:493–497
Pechstein U, Cedzich C, Nadstawek J, Schramm J (1996) Transcranial high-frequency repetitive electrical stimulation for recording myogenic motor evoked potentials with the patient under general anesthesia. Neurosurgery 39:335–344
Pelosi L, Stevenson M, Hobbs GJ, Jardine A, Webb JK (2001) Intraoperative motor evoked potentials to transcranial electrical stimulation during two anaesthetic regimens. Clin Neurophysiol 112:1076–1087
Schindler E, Müller M, Zickmann B, Osmer C, Wozniak G, Hempelmann G (1998) Modulation of somatosensory evoked potentials under various concentrations of desflurane with and without nitrous oxide. J Neurosurg Anesthesiol 10:218–223
Shida Y, Shida C, Hiratsuka N, Kaji K, Ogata J (2012) High-frequency stimulation restored motor-evoked potentials to the baseline level in the upper extremities but not in the lower extremities under sevoflurane anesthesia in spine surgery. J Neurosurg Anesthesiol 24:113–120
Sloan TB, Janik D, Jameson L (2008) Multimodality monitoring of the central nervous system using motor-evoked potentials. Curr Opin Anaesthesiol 21:560–564
Sloan TB, Heyer EJ (2002) Anesthesia for intraoperative neurophysiologic monitoring of the spinal cord. J Clin Neurophysiol 19:430–443
Sloan T (2010) Anesthesia and intraoperative neurophysiological monitoring in children. Childs Nerv Syst 26:227–235
Tamkus AA, Rice K, Kim HL (2014) Differential rates of false-positive findings in transcranial electric motor evoked potential monitoring when using inhalational anesthesia versus total intravenous anesthesia during spine surgeries. Spine J. doi:10.1016/j.spinee.2013.08.037
Vaughan DJA (2001) Effects of different concentrations of sevoflurane and desflurane on subcortical somatosensory evoked responses in anaesthetized, non-stimulated patients. Br J Anaesth 86:59–62
Zhang JLW (2005) Effects of volatile anesthetics on cortical somatosensory evoked potential and bispectral index. Chung-Hua I Hsueh Tsa Chih 85:2700–2703
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Holdefer, R.N., Anderson, C., Furman, M. et al. A comparison of the effects of desflurane versus propofol on transcranial motor-evoked potentials in pediatric patients. Childs Nerv Syst 30, 2103–2108 (2014). https://doi.org/10.1007/s00381-014-2510-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-014-2510-8