Abstract
Objective
To present the worldwide antibiotic resistance rates of uropathogens reported in nosocomial urinary tract infections (NAUTI) during the period of 2003–2010.
Materials and methods
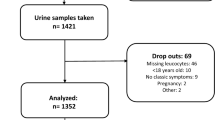
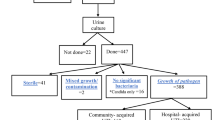
Data from the Global Prevalence Study of Infections in Urology from the period of 2003–2010 were analyzed to evaluate the resistance rates of pathogens causing NAUTI. The web-based application was used to record data of investigators from urology departments participating in the study every year during the days allocated in November. Each center was allowed to enter data on a single day of the study. The point prevalence data was used to find differences among geographic regions and years by utilizing multiple logistic regression analysis.
Results
A total of 19,756 patients were hospitalized during the study period, and in 1,866 of them, NAUTI was reported. Proof of infection was reported in 1,395 patients. Resistance rates of all antibiotics tested other than imipenem against the total bacterial spectrum were higher than 10 % in all regions. Resistance to almost all pathogens was lowest in North Europe, and there is no single year where an outbreak of resistance has been detected.
Conclusion
The resistance rates of most of the uropathogens against the antibiotics tested did not show significant trends of increase or decrease with Asia exhibiting the highest rates in general. The only antibiotic tested with an overall resistance rate below 10 % was imipenem. Knowledge of regional and local resistance data and prudent use of antibiotics are necessary to optimize antibiotic therapy in urological patients with NAUTI.


Similar content being viewed by others
References
Gastmeier P, Kampf G, Wischnewski N, Hauer T, Schulgen G, Schumacher M et al (1998) Prevalence of nosocomial infections in representative German hospitals. J Hosp Infect 38(1):37–49
Andrade SS, Sader HS, Jones RN, Pereira AS, Pignatari ACC, Gales AC (2006) Increased resistance to first-line agents among bacterial pathogens isolated from urinary tract infections in Latin America: time for local guidelines? Memórias do Instituto Oswaldo Cruz 101(7):741–748
Fluit AC, Jones ME, Schmitz FJ, Acar J, Gupta R, Verhoef J (1997) (2000) Antimicrobial resistance among urinary tract infection (UTI) isolates in Europe: results from the SENTRY Antimicrobial Surveillance Program. Antonie Van Leeuwenhoek 77(2):147–152
Wagenlehner FME, Niemetz A, Dalhoff A, Naber KG (2002) Spectrum and antibiotic resistance of uropathogens from hospitalized patients with urinary tract infections: 1994-2000. Int J Antimicrob Agents 19(6):557–564
Bjerklund Johansen TE, Cek M, Naber K, Stratchounski L, Svendsen MV, Tenke P (2007) Prevalence of hospital-acquired urinary tract infections in urology departments. Eur Urol 51(4):1100–1112
Johansen TE, Cek M, Naber KG, Stratchounski L, Svendsen MV, Tenke P (2006) Hospital acquired urinary tract infections in urology departments: pathogens, susceptibility and use of antibiotics. Data from the PEP and PEAP-studies. Int J Antimicrob Agents 28(Suppl 1):S91–S107
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36(5):309–332
Shaifali I, Gupta U, Mahmood SE, Ahmed J (2012) Antibiotic susceptibility patterns of urinary pathogens in female outpatients. N Am J Med Sci 4(4):163–169
Elhanan G, Sarhat M, Raz R (1997) Empiric antibiotic treatment and the misuse of culture results and antibiotic sensitivities in patients with community-acquired bacteraemia due to urinary tract infection. J infect 35(3):283–288
Cullen IM, Manecksha RP, McCullagh E, Ahmad S, O’Kelly F, Flynn RJ et al (2012) The changing pattern of antimicrobial resistance within 42,033 Escherichia coli isolates from nosocomial, community and urology patient-specific urinary tract infections, Dublin, 1999-2009. BJU int 109(8):1198–1206
Kahlmeter G, Poulsen HOn (2012) Antimicrobial susceptibility of Escherichia coli from community-acquired urinary tract infections in Europe: the ECO·SENS study revisited. Int J Antimicrob Agents 39(1):45–51
Bonkat G, M√ºller G, Braissant O, Frei R, Tschudin-Suter S, Rieken M, et al (2013) Increasing prevalence of ciprofloxacin resistance in extended-spectrum-ß-lactamase-producing Escherichia coli urinary isolates. World journal of urology
Nys S, Terporten PH, Hoogkamp-Korstanje JAA, Stobberingh EE, Group SSS (2008) Trends in antimicrobial susceptibility of Escherichia coli isolates from urology services in The Netherlands (1998–2005). J antimicrobial chemotherapy 62(1):126–132
Peña C, Pujol M, Ricart A, Ardanuy C, Ayats J, Liñares J et al (1997) Risk factors for faecal carriage of Klebsiella pneumoniae producing extended spectrum beta-lactamase (ESBL-KP) in the intensive care unit. J Hosp Infect 35(1):9–16
Lautenbach E, Patel JB, Bilker WB, Edelstein PH, Fishman NO (2001) Extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae: risk factors for infection and impact of resistance on outcomes. Clin Infect Dis 32(8):1162–1171
Akduman B, Akduman D, Tokgöz H, Erol B, Türker T, Ayoğlu F et al (2011) Long-term fluoroquinolone use before the prostate biopsy may increase the risk of sepsis caused by resistant microorganisms. Urology 78(2):250–255
Cek M, Tandoğdu Z, Naber K, Tenke P, Wagenlehner F, van Oostrum E, et al (2012) Antibiotic Prophylaxis in Urology Departments, 2005–2010. Eur Urol 63(2):386–394
Acknowledgments
This study was organized by the board of the ESIU and endorsed and sponsored by the EAU and performed in collaboration with the Asian Association of UTI and STD, the International Society of Chemotherapy for Infection and Cancer, and the Interregional Association of Clinical Microbiology and Antimicrobial Chemotherapy. We thank the EAU central office for administrative and secretarial assistance. The GPIU study group is most grateful to the altruistic contributions of the GPIU investigators (see supplementary material).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Zafer Tandogdu and Mete Cek authors have equally contributed.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tandogdu, Z., Cek, M., Wagenlehner, F. et al. Resistance patterns of nosocomial urinary tract infections in urology departments: 8-year results of the global prevalence of infections in urology study. World J Urol 32, 791–801 (2014). https://doi.org/10.1007/s00345-013-1154-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-013-1154-8