Abstract
Objectives
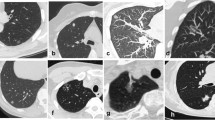
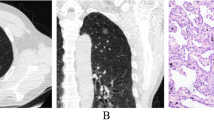
This study aims to predict the high-grade pattern (HGP) of stage IA lung invasive adenocarcinoma (IAC) based on the high-resolution CT (HRCT) features.
Methods
The clinical, pathological, and HRCT imaging data of 457 patients (from bicentric) with pathologically confirmed stage IA IAC (459 lesions in total) were retrospectively analyzed. The 459 lesions were classified into high-grade pattern (HGP) (n = 101) and non-high-grade pattern (n-HGP) (n = 358) groups depending on the presence of HGP (micropapillary and solid) in pathological results. The clinical and pathological data contained age, gender, smoking history, tumor stage, pathological type, and presence or absence of tumor spread through air spaces (STAS). CT features consisted of lesion location, size, density, shape, spiculation, lobulation, vacuole, air bronchogram, and pleural indentation. The independent predictors for HGP were screened by univariable and multivariable logistic regression analyses. The clinical, CT, and clinical-CT models were constructed according to the multivariable analysis results.
Results
The multivariate analysis suggested the independent predictors of HGP, encompassing tumor size (p = 0.001; OR = 1.090, 95% CI 1.035–1.148), density (p < 0.001; OR = 9.454, 95% CI 4.911–18.199), and lobulation (p = 0.002; OR = 2.722, 95% CI 1.438–5.154). The AUC values of clinical, CT, and clinical-CT models for predicting HGP were 0.641 (95% CI 0.583–0.699) (sensitivity = 69.3%, specificity = 79.2%), 0.851 (95% CI 0.806–0.896) (sensitivity = 79.2%, specificity = 79.6%), and 0.852 (95% CI 0.808–0.896) (sensitivity = 74.3%, specificity = 85.8%).
Conclusion
The logistic regression model based on HRCT features has a good diagnostic performance for the high-grade pattern of stage IA IAC.
Key Points
• The AUC values of clinical, CT, and clinical-CT models for predicting high-grade patterns were 0.641 (95% CI 0.583–0.699), 0.851 (95% CI 0.806–0.896), and 0.852 (95% CI 0.808–0.896).
• Tumor size, density, and lobulation were independent predictive markers for high-grade patterns.
• The logistic regression model based on HRCT features has a good diagnostic performance for the high-grade patterns of invasive adenocarcinoma.






Similar content being viewed by others
Abbreviations
- AC:
-
Adenocarcinoma
- AI:
-
Artificial intelligence
- ATS:
-
American Thoracic Society
- ERS:
-
European Respiratory Society
- HGP:
-
High-grade pattern
- HRCT:
-
High-resolution CT
- IAC:
-
Invasive adenocarcinoma
- IASLC:
-
International Association for the Study of Lung Cancer
- ICC:
-
Intraclass correlation coefficient
- LNM:
-
Lymph node metastasis
- ML:
-
Machine learning
- n-HGP:
-
Non-high-grade pattern
- SN:
-
Solid nodule
- SSN:
-
Subsolid nodule
- STAS:
-
Tumor spread through air spaces
- TNM:
-
Tumor node metastasis
References
Travis WD, Brambilla E, Noguchi M et al (2011) International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society: international multidisciplinary classification of lung adenocarcinoma: executive summary. Proc Am Thorac Soc 8:381–385
Takahashi Y, Eguchi T, Kameda K et al (2018) Histologic subtyping in pathologic stage I-IIA lung adenocarcinoma provides risk-based stratification for surveillance. Oncotarget 9:35742–35751
Yanagawa N, Shiono S, Abiko M, Katahira M, Osakabe M, Ogata SY (2016) The clinical impact of solid and micropapillary patterns in resected lung adenocarcinoma. J Thorac Oncol 11:1976–1983
Choi SH, Jeong JY, Lee SY et al (2021) Clinical implication of minimal presence of solid or micropapillary subtype in early-stage lung adenocarcinoma. Thorac Cancer 12:235–244
Rekhtman N, Brandt SM, Sigel CS et al (2011) Suitability of thoracic cytology for new therapeutic paradigms in non-small cell lung carcinoma: high accuracy of tumor subtyping and feasibility of EGFR and KRAS molecular testing. J Thorac Oncol 6(3):451–458
Nitadori J, Kadota K et al (2015) Using frozen section to identify histological patterns in stage I lung adenocarcinoma of ≤ 3 cm: accuracy and interobserver agreement. Histopathology. 66(7):922–938
Cahan WG (1960) Radical lobectomy. J Thorac Cardiovasc Surg 39:555–572
Ginsberg RJ, Rubinstein LV (1995) Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg 60(3):615–622 discussion 22-3
Keenan RJ, Landreneau RJ, Maley RH Jr, et al (2004) Segmental resection spares pulmonary function in patients with stage I lung cancer. Ann Thorac Surg 78(1):228–233 discussion -33
Kent MS, Mandrekar SJ, Landreneau R, et al (2016) Impact of sublobar resection on pulmonary function: long-term results from American College of Surgeons Oncology Group Z4032 (Alliance). Ann Thorac Surg 102(1):230–238
Gu C, Wang R, Pan X, et al (2017) Sublobar resection versus lobectomy in patients aged ≤35 years with stage IA non-small cell lung cancer: a SEER database analysis. J Cancer Res Clin Oncol 143(11):2375–2382
Veluswamy RR, Ezer N, Mhango G, et al (2015) Limited resection versus lobectomy for older patients with early-stage lung cancer: impact of histology. J Clin Oncol 33(30):3447–3453
Saji H, Okada M, Tsuboi M, et al (2022) Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): a multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet 399(10335):1607–1617
Nitadori J, Bograd AJ, Kadota K, et al (2013) Impact of micropapillary histologic subtype in selecting limited resection vs lobectomy for lung adenocarcinoma of 2cm or smaller. J Natl Cancer Inst 105(16):1212–1220
Hung JJ, Jeng WJ, Chou TY et al (2013) Prognostic value of the new International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society lung adenocarcinoma classification on death and recurrence in completely resected stage I lung adenocarcinoma. Ann Surg 258:1079–1086
Hung JJ, Yeh YC, Jeng WJ et al (2014) Predictive value of the International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society classification of lung adenocarcinoma in tumor recurrence and patient survival. J Clin Oncol 32:2357–236417
Choi Y, Aum J, Lee SH et al (2021) Deep learning analysis of CT images reveals high-grade pathological features to predict survival in lung adenocarcinoma. Cancers (Basel) 13
Wang X, Zhang L, Yang X et al (2020) Deep learning combined with radiomics may optimize the prediction in differentiating high-grade lung adenocarcinomas in ground glass opacity lesions on CT scans. Eur J Radiol 129:109150
Chen LW, Yang SM, Wang HJ et al (2021) Prediction of micropapillary and solid pattern in lung adenocarcinoma using radiomic values extracted from near-pure histopathological subtypes. Eur Radiol 31:5127–5138
Crosby D, Bhatia S, Brindle KM et al (2022) Early detection of cancer. Science 375:eaay9040
Goldstraw P, Chansky K, Crowley J et al (2016) The IASLC Lung Cancer Staging Project: proposals for revision of the TNM stage groupings in the forthcoming (Eighth) edition of the TNM classification for lung cancer. J Thorac Oncol 11:39–51
Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG (2015) Introduction to The 2015 World Health Organization classification of tumors of the lung, pleura, thymus, and heart. J Thorac Oncol 10:1240–1242
Meng Y, Liu CL, Cai Q, Shen YY, Chen SQ (2019) Contrast analysis of the relationship between the HRCT sign and new pathologic classification in small ground glass nodule-like lung adenocarcinoma. Radiol Med 124:8–13
Zhang Y, Qiang JW, Shen Y, Ye JD, Zhang J, Zhu L (2016) Using air bronchograms on multi-detector CT to predict the invasiveness of small lung adenocarcinoma. Eur J Radiol 85:571–577
Gao F, Li M, Ge X et al (2013) Multi-detector spiral CT study of the relationships between pulmonary ground-glass nodules and blood vessels. Eur Radiol 23:3271–3277
Jeon HW, Kim YD, Sim SB, Moon MH (2021) Significant difference in recurrence according to the proportion of high grade patterns in stage IA lung adenocarcinoma. Thorac Cancer 12:1952–1958
Lee G, Choi ER, Lee HY et al (2016) Pathologic heterogeneity of lung adenocarcinomas: a novel pathologic index predicts survival. Oncotarget 7:70353–70363
Choi Y, Kim J, Park H et al (2021) Rethinking a non-predominant pattern in invasive lung adenocarcinoma: prognostic dissection focusing on a high-grade pattern. Cancers (Basel) 13
Zhao ZR, Xi SY, Li W et al (2015) Prognostic impact of pattern-based grading system by the new IASLC/ATS/ERS classification in Asian patients with stage I lung adenocarcinoma. Lung Cancer 90:604–609
Vaghjiani RG, Takahashi Y, Eguchi T et al (2020) Tumor spread through air spaces is a predictor of occult lymph node metastasis in clinical stage IA lung adenocarcinoma. J Thorac Oncol 15:792–802
Sun F, Huang Y, Yang X et al (2020) Solid component ratio influences prognosis of GGO-featured IA stage invasive lung adenocarcinoma. Cancer Imaging 20:87
Miyoshi T, Aokage K, Katsumata S, Tane K, Ishii G, Tsuboi M (2019) Ground-glass opacity is a strong prognosticator for pathologic stage IA lung adenocarcinoma. Ann Thorac Surg 108:249–255
Ma X, Zhou S, Huang L et al (2021) Assessment of relationships among clinicopathological characteristics, morphological computer tomography features, and tumor cell proliferation in stage I lung adenocarcinoma. J Thorac Dis 13:2844–2857
Tsao MS, Marguet S, Le Teuff G et al (2015) Subtype classification of lung adenocarcinoma predicts benefit from adjuvant chemotherapy in patients undergoing complete resection. J Clin Oncol 33:3439–3446
Qian F, Yang W, Wang R et al (2018) Prognostic significance and adjuvant chemotherapy survival benefits of a solid or micropapillary pattern in patients with resected stage IB lung adenocarcinoma. J Thorac Cardiovasc Surg 155:1227–1235.e1222
Zhang P, Li T, Tao X, Jin X, Zhao S (2021) HRCT features between lepidic-predominant type and other pathological subtypes in early-stage invasive pulmonary adenocarcinoma appearing as a ground-glass nodule. BMC Cancer 21:1124
Funding
This work was supported by Major Research Plan of the National Natural Science Foundation of China (Grant No. 92059206), National Science Foundation of China (82071990), National Science Foundation of China (81571629), National Science Foundation of China (81301218), Project of Shanghai Science and Technology Commission (19411965200), Policy Guidance Project of Major Science and Technology Plan for Social Development of Xiaoshan District (No. 2021309), Hangzhou Agricultural and Social Development Scientific Research Guidance Project (20220919Y078), and Zhejiang Provincial Health Commission Youth Innovation Project (2023RC252).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Xiao-dan Ye.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
Two of the authors (Hao Dong and Xiao-Dan Ye) have significant statistical expertise.
Informed consent
Our hospital ethics committee approved this retrospective study and waived patient informed consent.
Ethical approval
Institutional review board approval was obtained.
Methodology
• retrospective
• diagnostic study
• performed at two institutions
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 24 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dong, H., Yin, LK., Qiu, YG. et al. Prediction of high-grade patterns of stage IA lung invasive adenocarcinoma based on high-resolution CT features: a bicentric study. Eur Radiol 33, 3931–3940 (2023). https://doi.org/10.1007/s00330-022-09379-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-09379-x