Abstract
Objectives
Radiological markers for cerebral small vessel disease (SVD) may have different biological underpinnings in their development. We attempted to categorize SVD burden by integrating white matter signal abnormalities (WMSA) features and secondary presence of lacunes, microbleeds, and enlarged perivascular spaces.
Methods
Data were acquired from 610 older adults (aged > 40 years) who underwent brain magnetic resonance imaging exam as part of a health checkup. The WMSA were classified individually by the number and size of non-contiguous lesions, distribution, and contrast. Age-detrended lacunes, microbleeds, and enlarged perivascular space were quantified to further categorize individuals. Clinical and laboratory values were compared across the individual classes.
Results
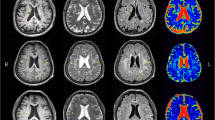
Class I was characterized by multiple, small, deep WMSA but a low burden of lacunes and microbleeds; class II had large periventricular WMSA and a high burden of lacunes and microbleeds; and class III had limited juxtaventricular WMSA and lacked lacunes and microbleeds. Class II was associated with older age, diabetes, and a relatively higher neutrophil-to-lymphocyte ratio. Smoking and higher uric acid levels were associated with an increased risk of class I.
Conclusion
The heterogeneity of SVD was categorized into three classes with distinct clinical correlates. This categorization will improve our understanding of SVD pathophysiology, risk stratification, and outcome prediction.
Key Points
• Classification of white matter signal abnormality (WMSA) features was associated with different characteristic of lacunes, microbleeds, and enlarged perivascular space and clinical variability.
• Class I was characterized by multiple, small, deep WMSA but a low burden of lacunes and microbleeds. Class II had large periventricular WMSA and a high burden of lacunes and microbleeds. Class III had limited juxtaventricular WMSA and lacked lacunes and microbleeds.
• Class II was associated with older age, diabetes, and higher neutrophil-to-lymphocyte ratio. Smoking and higher uric acid levels were associated with an increased risk of class I.


Similar content being viewed by others
Abbreviations
- CMB:
-
Cerebral microbleeds
- EPVS:
-
Enlarged perivascular spaces
- NLR:
-
Neutrophil-to-lymphocyte ratio
- SVD:
-
Small vessel disease
- WMSA:
-
White matter signal abnormalities
References
Inzitari D, Pracucci G, Poggesi A et al (2009) Changes in white matter as determinant of global functional decline in older independent outpatients: three year follow-up of LADIS (leukoaraiosis and disability) study cohort. BMJ 339:b2477
Wardlaw JM, Smith EE, Biessels GJ et al (2013) Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol 12:822–838
Gouw AA, Seewann A, van der Flier WM et al (2011) Heterogeneity of small vessel disease: a systematic review of MRI and histopathology correlations. J Neurol Neurosurg Psychiatry 82:126–135
Wardlaw JM, Smith C, Dichgans M (2019) Small vessel disease: mechanisms and clinical implications. Lancet Neurol 18:684–696
Jung KH, Stephens KA, Yochim KM et al (2021) Heterogeneity of cerebral white matter lesions and clinical correlates in older adults. Stroke 52:620–630
Ghaznawi R, Geerlings MI, Jaarsma-Coes M, Hendrikse J, de Bresser J (2021) Association of white matter hyperintensity markers on MRI and long-term risk of mortality and ischemic stroke: the SMART-MR Study. Neurology 96:e2172–e2183
Adachi T, Kobayashi S, Yamaguchi S, Okada K (2000) MRI findings of small subcortical “lacunar-like” infarction resulting from large vessel disease. J Neurol 247:280–285
Shoamanesh A, Kwok CS, Benavente O (2011) Cerebral microbleeds: histopathological correlation of neuroimaging. Cerebrovasc Dis 32:528–534
Wardlaw JM, Benveniste H, Nedergaard M et al (2020) Perivascular spaces in the brain: anatomy, physiology and pathology. Nat Rev Neurol 16:137–153
Gracien RM, Maiworm M, Brüche N et al (2020) How stable is quantitative MRI? - Assessment of intra- and inter-scanner-model reproducibility using identical acquisition sequences and data analysis programs. Neuroimage 207:116364
Dale AM, Fischl B, Sereno MI (1999) Cortical surface-based analysis. I. Segmentation and surface reconstruction. Neuroimage 9:179–194
Fischl B, Salat DH, Busa E et al (2002) Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron 33:341–355
Cordonnier C, Potter GM, Jackson CA et al (2009) Improving interrater agreement about brain microbleeds: development of the Brain Observer MicroBleed Scale (BOMBS). Stroke 40:94–99
Gregoire SM, Chaudhary UJ, Brown MM et al (2009) The microbleed anatomical rating scale (MARS): reliability of a tool to map brain microbleeds. Neurology 73:1759–1766
Doubal FN, MacLullich AM, Ferguson KJ, Dennis MS, Wardlaw JM (2010) Enlarged perivascular spaces on MRI are a feature of cerebral small vessel disease. Stroke 41:450–454
Vermeer SE, Longstreth WT Jr, Koudstaal PJ (2007) Silent brain infarcts: a systematic review. Lancet Neurol 6:611–619
Staals J, Makin SD, Doubal FN, Dennis MS, Wardlaw JM (2014) Stroke subtype, vascular risk factors, and total MRI brain small-vessel disease burden. Neurology 83:1228–1234
van Leijsen EMC, van Uden IWM, Ghafoorian M et al (2017) Nonlinear temporal dynamics of cerebral small vessel disease: The RUN DMC study. Neurology 89:1569–1577
Nonaka H, Akima M, Hatori T, Nagayama T, Zhang Z, Ihara F (2003) Microvasculature of the human cerebral white matter: arteries of the deep white matter. Neuropathology 23:111–118
Lee MJ, Park BY, Cho S, Park H, Chung CS (2019) Cerebrovascular reactivity as a determinant of deep white matter hyperintensities in migraine. Neurology 92:e342–e350
Fukuda H, Kitani M (1996) Cigarette smoking is correlated with the periventricular hyperintensity grade of brain magnetic resonance imaging. Stroke 27:645–649
Choi YJ, Yoon Y, Lee KY et al (2014) Uric acid induces endothelial dysfunction by vascular insulin resistance associated with the impairment of nitric oxide synthesis. FASEB J 28:3197–3204
Yang S, Zhang X, Yuan J, Yin J, Hu W (2017) Serum uric acid is independently associated with enlarged perivascular spaces. Sci Rep 7:16435
Wardlaw JM, Smith C, Dichgans M (2013) Mechanisms of sporadic cerebral small vessel disease: insights from neuroimaging. Lancet Neurol 12:483–497
Pantoni L (2010) Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol 9:689–701
Duering M, Csanadi E, Gesierich B et al (2013) Incident lacunes preferentially localize to the edge of white matter hyperintensities: insights into the pathophysiology of cerebral small vessel disease. Brain 136:2717–2726
Nyquist PA, Bilgel M, Gottesman R et al (2015) Age differences in periventricular and deep white matter lesions. Neurobiol Aging 36:1653–1658
Romero JR, Preis SR, Beiser A et al (2014) Risk factors, stroke prevention treatments, and prevalence of cerebral microbleeds in the Framingham Heart Study. Stroke 45:1492–1494
Nam KW, Kwon HM, Jeong HY et al (2017) High neutrophil to lymphocyte ratio is associated with white matter hyperintensity in a healthy population. J Neurol Sci 380:128–131
Black S, Gao F, Bilbao J (2009) Understanding white matter disease: imaging-pathological correlations in vascular cognitive impairment. Stroke 40:S48–S52
Houck AL, Gutierrez J, Gao F et al (2019) Increased diameters of the internal cerebral veins and the basal veins of rosenthal are associated with white matter hyperintensity volume. AJNR Am J Neuroradiol 40:1712–1718
Dadar M, Maranzano J, Ducharme S, Carmichael OT, Decarli C, Collins DL (2018) Validation of T1w-based segmentations of white matter hyperintensity volumes in large-scale datasets of aging. Hum Brain Mapp 39:1093–1107
Funding
This work was supported by grants from the SNUH Research Fund (0520200010) and the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (2020R1A2C1100337).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Keun-Hwa Jung, MD, PhD.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
This study was approved by the institutional review board of Seoul National University Hospital.
Methodology
• Retrospective
• Cross-sectional study
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(PDF 593 kb)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Park, KI., Jung, KH., Lee, EJ. et al. Classification of white matter lesions and characteristics of small vessel disease markers. Eur Radiol 33, 1143–1151 (2023). https://doi.org/10.1007/s00330-022-09070-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-09070-1