Abstract
Objective
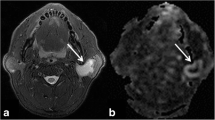
To evaluate the influence of post-label delay times (PLDs) on the performance of 3D pseudo-continuous arterial spin labeling (pCASL) magnetic resonance imaging for characterizing parotid gland tumors and to explore the optimal PLDs for the differential diagnosis.
Materials and method
Fifty-eight consecutive patients with parotid gland tumors were enrolled, including 33 patients with pleomorphic adenomas (PAs), 16 patients with Warthin’s tumors (WTs), and 9 patients with malignant tumors (MTs). 3D pCASL was scanned for each patient five times, with PLDs of 1025 ms, 1525 ms, 2025 ms, 2525 ms, and 3025 ms. Tumor blood flow (TBF) was calculated, and compared among different PLDs and tumor groups. Performance of TBF at different PLDs was evaluated using receiver operating characteristic analysis.
Results
With an increasing PLD, TBF tended to gradually increase in PAs (p < 0.001), while TBF tended to slightly increase and then gradually decrease in WTs (p = 0.001), and PAs showed significantly lower TBF than WTs at all 5 PLDs (p < 0.05). PAs showed significantly lower TBF than MTs at 4 PLDs (p < 0.05), except at 3025 ms (p = 0.062). WTs showed higher TBF than MTs at all 5 PLDs; however, differences did not reach significance (p > 0.05). Setting a TBF of 64.350 mL/100g/min at a PLD of 1525 ms, or a TBF of 23.700 mL/100g/min at a PLD of 1025 ms as the cutoff values, optimal performance could be obtained for differentiating PAs from WTs (AUC = 0.905) or from MTs (AUC = 0.872).
Conclusions
Short PLDs (1025 ms or 1525 ms) are suggested to be used in 3D pCASL for characterizing parotid gland tumors in clinical practice.
Key Points
• With 5 different PLDs, 3D pCASL can reflect the variation of blood flow in parotid gland tumors.
• 3D pCASL is useful for characterizing PAs from WTs or MTs.
• Short PLDs (1025 ms or 1525 ms) are suggested to be used in 3D pCASL for characterizing parotid gland tumors in clinical practice.



Similar content being viewed by others
Abbreviations
- 3D pCASL:
-
Three-dimensional pseudo-continuous arterial spin labeling
- ADW:
-
Vendor-provided workstation
- FOV:
-
Field of view
- FSE:
-
Fast spin echo
- ICC:
-
Intraclass correlation coefficient
- MTs:
-
Malignant tumors
- PAs:
-
Pleomorphic adenomas
- PLD:
-
Post-label delay time
- SIR:
-
Signal intensity ratio
- TBF:
-
Tumor blood flow
- TE:
-
Echo time
- TR:
-
Repetition time
- WTs:
-
Warthin’s tumors
References
Freling N, Crippa F, Maroldi R (2016) Staging and follow-up of high-grade malignant salivary gland tumors: the role of traditional versus functional imaging approaches – a review. Oral Oncol 60:157–166
Speight PM, Barrett AW (2002) Salivary gland tumors. Oral Dis 8:229–240
Gökçe E (2020) Multiparametric magnetic resonance imaging for the diagnosis and differential diagnosis of parotid gland tumors. J Magn Reson Imaging 52:11–32
Razek AAKA (2018a) Characterization of salivary gland tumours with diffusion tensor imaging. Dentomaxillofac Radiol 47:20170343
Ma G, Xu XX, Zhu LN et al (2021) Intravoxel incoherent motion magnetic resonance imaging for assessing parotid gland tumors: correlation and comparison with arterial spin labeling imaging. Korean J Radiol 22:243–252
Reddy VM, Thangarajah T, Castellanos-Arango F, Panarese A (2008) Conservative management of Warthin tumour. J Otolaryngol Head Neck Surg 37:744–749
Gudmundsson JK, Ajan A, Abtahi J (2016) The accuracy of fine-needle aspiration cytology for diagnosis of parotid gland masses: a clinicopathological study of 114 patients. J Appl Oral Sci 24:561–567
Razek AAKA, Mukherji SK (2018) State-of-the-art imaging of salivary gland tumors. Neuroimaging Clin N Am 28:303–317
Razek AAKA (2018b) Routine and advanced diffusion imaging modules of the salivary glands. Neuroimaging Clin N Am 28:245–254
Tao X, Yang G, Wang P et al (2017) The value of combining conventional, diffusion-weighted and dynamic contrast-enhanced MR imaging for the diagnosis of parotid gland tumours. Dentomaxillofac Radiol 46:20160434
Munhoz L, Ramos EADA, Im DC et al (2019) Application of diffusion-weighted magnetic resonance imaging in the diagnosis of salivary gland diseases: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol 128:280–310
Matsushima N, Maeda M, Takamura M, Takeda K (2007) Apparent diffusion coefficients of benign and malignant salivary gland tumors. Comparison to histopathological findings. J Neuroradiol 34:183–189
Habermann CR, Arndt C, Graessner J et al (2009) Diffusion-weighted echo-planar MR imaging of primary parotid gland tumors: is a prediction of different histologic subtypes possible? AJNR Am J Neuroradiol 30:591–596
Zhang Z, Song C, Zhang Y, Wen B, Zhu J, Cheng J (2019) Apparent diffusion coefficient (ADC) histogram analysis: differentiation of benign from malignant parotid gland tumors using readout-segmented diffusion-weighted imaging. Dentomaxillofac Radiol 48:20190100
Ogawa T, Suzuki T, Sakamoto M et al (2012) Correct diagnosis of Warthin tumor in the parotid gland with dynamic MRI. Tohoku J Exp Med 227:53–57
Choi JW, Moon WJ (2019) Gadolinium deposition in the brain: current updates. Korean J Radiol 20:134–147
Fujima N, Kudo K, Yoshida D et al (2014) Arterial spin labeling to determine tumor viability in head and neck cancer before and after treatment. J Magn Reson Imaging 40:920–928
Amukotuwa SA, Yu C, Zaharchuk G (2016) 3D Pseudocontinuous arterial spin labeling in routine clinical practice: a review of clinically significant artifacts. J Magn Reson Imaging 43:11–27
Alsop DC, Detre JA, Golay X et al (2015) Recommended implementation of arterial spin labeled perfusion MRI for clinical applications: a consensus of the ISMRM Perfusion Study Group and the European Consortium for ASL in Dementia. Magn Reson Imaging 73:102–116
Razek AAKA (2019) Multi-parametric MR imaging using pseudo-continuous arterial-spin labeling and diffusion-weighted MR imaging in differentiating subtypes of parotid tumors. Magn Reson Imaging 63:55–59
Yamamoto T, Kimura H, Hayashi K, Imamura Y, Mori M (2018) Pseudo-continuous arterial spin labeling MR images in Warthin tumors and pleomorphic adenomas of the parotid gland: qualitative and quantitative analyses and their correlation with histopathologic and DWI and dynamic contrast enhanced MRI findings. Neuroradiology 60:803–812
Wang DJJ, Alger JR, Qiao JX et al (2013) Multi-delay multi-parametric arterial spin-labeled perfusion MRI in acute ischemic stroke-comparison with dynamic susceptibility contrast enhanced perfusion imaging. Neuroimage Clin 3:1–7
Maclntosh BJ, Lindsay AC, Kylintireas I et al (2010) Multiple inflow pulsed arterial spin-labeling reveals delays in the arterial arrival time in minor stroke and transient ischemic attack. AJNR Am J Neuroradiol 31:1892–1894
Zhu L, Wang J, Shi H, Tao X (2019) Multimodality fMRI with perfusion, diffusion-weighted MRI and 1H-MRS in the diagnosis of lympho-associated benign and malignant lesions of the parotid gland. J Magn Reson Imaging 49:423–432
Dong Y, Lei GW, Wang SW, Zheng SW, Ge Y, Wei FC (2014) Diagnostic value of CT perfusion imaging for parotid neoplasms. Dentomaxillofac Radiol 43:20130237
Razek AAKA, Helmy E (2021) Multi-parametric arterial spin labeling and diffusion-weighted imaging in differentiation of metastatic from reactive lymph nodes in head and neck squamous cell carcinoma. Eur Arch Otorhinolaryngol 278:2529–2535
Sun Z, Hu S, Ge Y, Jin L, Huang J, Dou W (2021) Can arterial spin labeling perfusion imaging be used to differentiate nasopharyngeal carcinoma from nasopharyngeal lymphoma? J Magn Reson Imaging 53:1140–1148
Santos WPD, Gomes JPP, Nussi AD et al (2020) Morphology, volume, and density characteristics of the parotid glands before and after chemoradiation therapy in patients with head and neck tumors. Int J Dent. https://doi.org/10.1155/2020/8176260
Funding
This work was supported by the National Natural Science Foundation of China (81771796 to FY Wu), Jiangsu Province’s Young Medical Talents Program (QNRC 2016560 to Xu XQ), and Outstanding Young and Middle-aged Talents Support Program of The First Affiliated Hospital of Nanjing Medical University (Jiangsu Province Hospital).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Xiao-Quan Xu.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hu, H., Chen, L., Zhu, LN. et al. Influence of post-label delay time on the performance of 3D pseudo-continuous arterial spin labeling magnetic resonance imaging in the characterization of parotid gland tumors. Eur Radiol 32, 1087–1094 (2022). https://doi.org/10.1007/s00330-021-08220-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08220-1