Abstract
Objective
To determine whether pericruciate fat pad (PCFP) signal intensity alteration and maximal area are associated with incident radiographic osteoarthritis (ROA) over 4 years in the Osteoarthritis Initiative (OAI) study.
Methods
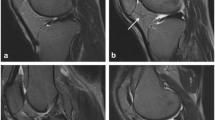
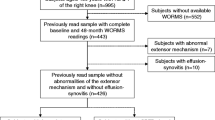
Participants were from the Osteoarthritis Initiative (OAI) study. Case knees (n = 355) were defined by incident ROA between 12 and 48 months visits and were matched by sex, age, and radiographic status with control knees (n = 355). Magnetic resonance images (MRIs) were used to assess PCFP signal intensity alteration and PCFP maximal area at P0 (time of onset of ROA), P-1 (1 year prior to P0), and baseline. Conditional logistic regression analyses were applied to assess associations between PCFP measures and the risk of incident ROA.
Results
The mean age of participants was 60.1 years and 66.9% were women. In multivariable analyses, PCFP signal intensity alteration measured at three time points (OR [95%CI]: 1.28 [1.10–1.50], 1.52 [1.30–1.78], 1.50 [1.27–1.76], respectively) and PCFP maximal area (OR [95%CI]: 1.21 [1.03–1.42], 1.27 [1.07–1.52], 1.37 [1.15–1.62], respectively) were significantly associated with incident ROA.
Conclusions
PCFP signal intensity alteration and maximal area were associated with incident ROA over 4 years, implying that they may have roles to play in ROA.
Key Points
• Pericruciate fat pad signal intensity alteration and maximal area were associated with incident ROA, implying that they may have roles to play in ROA.



Similar content being viewed by others
Abbreviations
- ACL:
-
Anterior cruciate ligament
- BMI:
-
Body mass index
- BML:
-
Bone marrow lesion
- ICC:
-
Intraclass correlation coefficient
- IPFP:
-
Infrapatellar fat pad
- KLG:
-
Kellgren Lawrence grade
- MOAKS:
-
MRI OA Knee Score
- MRI:
-
Magnetic resonance image
- OA:
-
Osteoarthritis
- OAI:
-
Osteoarthritis Initiative
- OR:
-
Odds ratio
- PCFP:
-
Pericruciate fat pad
- PCL:
-
Posterior cruciate ligament
- PFP:
-
Prefemoral fat pad
- QFP:
-
Quadriceps fat pad
- ROA:
-
Radiographic osteoarthritis
References
Hunter DJ, Bierma-Zeinstra S (2019) Osteoarthritis. Lancet 393:1745–1759
Clockaerts S, Bastiaansen-Jenniskens YM, Runhaar J et al (2010) The infrapatellar fat pad should be considered as an active osteoarthritic joint tissue: a narrative review. Osteoarthritis Cartilage 18:876–882
Zhu Z, Li J, Ruan G, Wang G, Huang C, Ding C (2018) Investigational drugs for the treatment of osteoarthritis, an update on recent developments. Expert Opin Investig Drugs 27:881–900
Grando H, Chang EY, Chen KC, Chung CB (2014) MR imaging of extrasynovial inflammation and impingement about the knee. Magn Reson Imaging Clin N Am 22:725–741
Skaf AY, Hernandez Filho G, Dirim B et al (2012) Pericruciate fat pad of the knee: anatomy and pericruciate fat pad inflammation: cadaveric and clinical study emphasizing MR imaging. Skeletal Radiol 41:1591–1596
Chang J, Liao Z, Lu M, Meng T, Han W, Ding C (2018) Systemic and local adipose tissue in knee osteoarthritis. Osteoarthritis Cartilage 26:864–871
Lapegue F, Sans N, Brun C et al (2016) Imaging of traumatic injury and impingement of anterior knee fat. Diagn Interv Imaging 97:789–807
Muñoz-Criado I, Meseguer-Ripolles J, Mellado-López M et al (2017) Human suprapatellar fat pad-derived mesenchymal stem cells induce chondrogenesis and cartilage repair in a model of severe osteoarthritis. Stem Cells Int 2017:4758930
Roemer FW, Jarraya M, Felson DT et al (2016) Magnetic resonance imaging of Hoffa’s fat pad and relevance for osteoarthritis research: a narrative review. Osteoarthritis Cartilage 24:383–397
Atukorala I, Kwoh CK, Guermazi A et al (2016) Synovitis in knee osteoarthritis: a precursor of disease? Ann Rheum Dis 75:390–395
Cai J, Xu J, Wang K et al (2015) Association between infrapatellar fat pad volume and knee structural changes in patients with knee osteoarthritis. J Rheumatol 42:1878–1884
Pan F, Han W, Wang X et al (2015) A longitudinal study of the association between infrapatellar fat pad maximal area and changes in knee symptoms and structure in older adults. Ann Rheum Dis 74:1818–1824
Wang K, Ding C, Hannon MJ et al (2018) Signal intensity alteration within infrapatellar fat pad predicts knee replacement within 5 years: data from the Osteoarthritis Initiative. Osteoarthritis Cartilage 26:1345–1350
De Maeseneer M, Wuertzer S, de Mey J, Shahabpour M (2017) The imaging findings of impingement syndromes of the lower limb. Clin Radiol 72:1014–1024
Draghi F, Torresi M, Urciuoli L, Gitto S (2017) Magnetic resonance signal abnormalities within the pericruciate fat pad: a possible secondary sign for acute anterior cruciate ligament tears. Can Assoc Radiol J 68:438–444
Lord BR, El-Daou H, Zdanowicz U, Smigielski R, Amis AA (2019) The role of fibers within the tibial attachment of the anterior cruciate ligament in restraining tibial displacement. Arthroscopy 35:2101–2111
Peterfy CG, Schneider E, Nevitt M (2008) The osteoarthritis initiative: report on the design rationale for the magnetic resonance imaging protocol for the knee. Osteoarthritis Cartilage 16:1433–1441
Roemer FW, Kwoh CK, Hannon MJ et al (2015) What comes first? Multitissue involvement leading to radiographic osteoarthritis: magnetic resonance imaging-based trajectory analysis over four years in the osteoarthritis initiative. Arthritis Rheumatol 67:2085–2096
Hunter DJ, Guermazi A, Lo GH et al (2011) Evolution of semi-quantitative whole joint assessment of knee OA: MOAKS (MRI Osteoarthritis Knee Score). Osteoarthritis Cartilage 19:990–1002
Johnson VL, Kwoh CK, Guermazi A et al (2015) Loss of anterior cruciate ligament integrity and the development of radiographic knee osteoarthritis: a sub-study of the osteoarthritis initiative. Osteoarthritis Cartilage 23:882–887
Han W, Aitken D, Zhu Z et al (2016) Signal intensity alteration in the infrapatellar fat pad at baseline for the prediction of knee symptoms and structure in older adults: a cohort study. Ann Rheum Dis 75:1783–1788
Wang K, Ding C, Hannon MJ, Chen Z, Kwoh CK, Hunter DJ (2019) Quantitative signal intensity alteration in infrapatellar fat pad predicts incident radiographic osteoarthritis: the Osteoarthritis Initiative. Arthritis Care Res (Hoboken) 71:30–38
Teichtahl AJ, Wulidasari E, Brady SR et al (2015) A large infrapatellar fat pad protects against knee pain and lateral tibial cartilage volume loss. Arthritis Res Ther 17:318
Everhart JS, Abouljoud MM, Flanigan DC (2019) Role of full-thickness cartilage defects in knee osteoarthritis (OA) incidence and progression: data from the OA Initiative. J Orthop Res 37:77–83
Crema MD, Felson DT, Roemer FW et al (2013) Peripatellar synovitis: comparison between non-contrast-enhanced and contrast-enhanced MRI and association with pain. The MOST study. Osteoarthritis Cartilage 21:413–418
Roemer FW, Guermazi A, Zhang Y et al (2009) Hoffa’s fat pad: evaluation on unenhanced MR images as a measure of patellofemoral synovitis in osteoarthritis. AJR Am J Roentgenol 192:1696–1700
Pishgar F, Guermazi A, Roemer FW, Link TM, Demehri S (2021) Conventional MRI-based subchondral trabecular biomarkers as predictors of knee osteoarthritis progression: data from the Osteoarthritis Initiative. Eur Radiol 31:3564–3573
Acknowledgements
Special thanks go to the subjects who made this study possible, the OAI investigators, POMA investigators, staff, and participants.
Funding
This work was supported by the National Natural Science Foundation of China (81773532). This study and image acquisition were funded by the OAI study and POMA study. The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) and the National Institute on Aging (NIA) lead this initiative at the National Institutes of Health (NIH). Private funding partners include Merck Research Laboratories, Novartis Pharmaceuticals Corporation, GlaxoSmithKline, and Pfizer. Private sector funding for the OAI is being managed by the Foundation for the National Institutes of Health. The POMA study was funded by the NIH’s National Heart, Lung, and Blood Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Changhai Ding, M.D. (Clinical Research Centre, Zhujiang Hospital, Southern Medical University, Guangzhou, Guangdong, China).
Conflict of interest
The authors of this manuscript declare relationships with the following companies: DJH provides consulting advice to Pfizer, Lilly, TLC bio, Merck Serono.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• nested case-control study
• multicenter study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 79.3 kb)
Rights and permissions
About this article
Cite this article
Li, Y., Li, J., Zhu, Z. et al. Signal intensity alteration and maximal area of pericruciate fat pad are associated with incident radiographic osteoarthritis: data from the Osteoarthritis Initiative. Eur Radiol 32, 489–496 (2022). https://doi.org/10.1007/s00330-021-08193-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08193-1