Abstract
Objectives
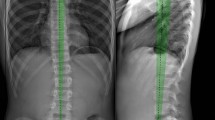
Adolescent idiopathic scoliosis (AIS) is the most common spinal disorder in children. A severity index was recently proposed to identify the stable from the progressive scoliosis at the first standardized biplanar radiographic exam. The aim of this work was to extend the validation of the severity index and to determine if curve location influences its predictive capabilities.
Methods
AIS patients with Cobb angle between 10° and 25°, Risser 0–2, and no previous treatment were included. They underwent standing biplanar radiography and 3D reconstruction of the spine and pelvis, which allowed to calculate their severity index. Patients were grouped by curve location (thoracic, thoracolumbar, lumbar). Patients were followed up until skeletal maturity (Risser ≥ 3) or brace prescription. Their outcome was compared to the prediction made by the severity index.
Results
In total, 205 AIS patients were included; 82% of them (155/189, 95% confidence interval [74–90%]) were correctly classified by the index, while 16 patients were unclassified. Positive predictive ratio was 78% and negative predictive ratio was 86%. Specificity (78%) was not significantly affected by curve location, while patients with thoracic and lumbar curves showed higher sensitivity (≥ 89%) than those with thoracolumbar curves (74%).
Conclusions
In this multicentric cohort of 205 patients, the severity index was used to predict the risk of progression from mild to moderate scoliosis, with similar results of typical major curve types. This index represents a novel tool to aid the clinician and the patient in the modulation of the follow-up and, for progressive patients, their decision for brace treatment.
Key Points
• The severity index of adolescent idiopathic scoliosis has the potential to detect patients with progressive scoliosis as early as the first exam.
• Out of 205 patients, 82% were correctly classified as either stable or progressive by the severity index.
• The location of the main curve had small effect on the predictive capability of the index.






Similar content being viewed by others
Abbreviations
- AIS:
-
Adolescent idiopathic scoliosis
- AUC:
-
Area under the curve
- ROC curve:
-
Receiver operating characteristic curve
- SOSORT:
-
Society on Scoliosis Orthopaedic and Rehabilitation Treatment
References
Konieczny MR, Senyurt H, Krauspe R (2013) Epidemiology of adolescent idiopathic scoliosis. J Child Orthop 7:3–9. https://doi.org/10.1007/s11832-012-0457-4
Kearon C, Viviani GR, Kirkley A, Killian KJ (1993) Factors determining pulmonary function in adolescent idiopathic thoracic scoliosis. Am Rev Respir Dis 148:288–294. https://doi.org/10.1164/ajrccm/148.2.288
Danielsson AJ (2013) Natural history of adolescent idiopathic scoliosis: A tool for guidance in decision of surgery of curves above 50°. J Child Orthop 7:37–41. https://doi.org/10.1007/s11832-012-0462-7
Tones M, Moss N, Polly DWJ (2006) A review of quality of life and psychosocial issues in scoliosis. Spine (Phila Pa 1976) 31:3027–3038. https://doi.org/10.1097/01.brs.0000249555.87601.fc
Negrini S, Donzelli S, Aulisa AG et al (2018) 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord 13:3. https://doi.org/10.1186/s13013-017-0145-8
Bunnell WP (1986) The natural history of idiopathic scoliosis before skeletal maturity. Spine (Phila Pa 1976) 11:773–776
Hresko MT, Talwalkar V, Schwend R et al (2016) Early detection of idiopathic scoliosis in adolescents. J Bone Joint Surg Am 98:e67. https://doi.org/10.2106/JBJS.16.00224
Illés TS, Lavaste F, Dubousset JF (2019) The third dimension of scoliosis: The forgotten axial plane. Orthop Traumatol Surg Res 105:351–359. https://doi.org/10.1016/j.otsr.2018.10.021
Skalli W, Vergari C, Ebermeyer E et al (2017) Early detection of progressive adolescent idiopathic scoliosis: A severity index. Spine (Phila Pa 1976) 42:823–830. https://doi.org/10.1097/BRS.0000000000001961
Vergari C, Gajny L, Courtois I et al (2019) Quasi-automatic early detection of progressive idiopathic scoliosis from biplanar radiography: A preliminary validation. Eur Spine J 28:1970–1976. https://doi.org/10.1007/s00586-019-05998-z
Humbert L, De Guise JA, Aubert B et al (2009) 3D reconstruction of the spine from biplanar X-rays using parametric models based on transversal and longitudinal inferences. Med Eng Phys 31:681–687. https://doi.org/10.1016/j.medengphy.2009.01.003
Bitan FD, Veliskakis KP, Campbell BC (2005) Differences in the Risser grading systems in the United States and France. Clin Orthop Relat Res 190–195. https://doi.org/10.1097/01.blo.0000160819.10767.88
Faro FD, Marks MC, Pawelek J, Newton PO (2004) Evaluation of a functional position for lateral radiograph acquisition in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 29:2284–2289
O’Brien MF, Kulklo TR, Blanke KM, Lenke LG (2008) Radiographic measurement manual. Medtronic Sofamor Danek USA, Inc
Steib J-P, Dumas R, Mitton D, Skalli W (2004) Surgical correction of scoliosis by in situ contouring: A detorsion analysis. Spine (Phila Pa 1976) 29:193–199. https://doi.org/10.1097/01.BRS.0000107233.99835.A4
Skalli W, Vergari C, Ebermeyer E et al (2017) Early detection of progressive adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 42:823–830. https://doi.org/10.1097/BRS.0000000000001961
Hajian-Tilaki K (2014) Sample size estimation in diagnostic test studies of biomedical informatics. J Biomed Inform 48:193–204. https://doi.org/10.1016/j.jbi.2014.02.013
Hosmer DW, Lemeshow S, Sturdivant RX (2013) Applied logistic regression, 3rd edn. John Wiley & Sons, Hoboken
Gajny L, Ebrahimi S, Vergari C et al (2019) Quasi-automatic 3D reconstruction of the full spine from low-dose biplanar X-rays based on statistical inferences and image analysis. Eur Spine J 28:658–664. https://doi.org/10.1007/s00586-018-5807-6
Aubert B, Vazquez C, Cresson T et al (2019) Toward automated 3D spine reconstruction from biplanar radiographs using CNN for statistical spine model fitting. IEEE Trans Med Imaging 38:2796–2806. https://doi.org/10.1109/TMI.2019.2914400
Gajny L, Ebrahimi S, Vergari C et al (2018) Quasi-automatic 3D reconstruction of the full spine from low-dose biplanar X-rays based on statistical inferences and image analysis. Eur Spine J. https://doi.org/10.1007/s00586-018-5807-6
Dolan LA, Weinstein SL, Abel MF et al (2019) Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST): Development and validation of a prognostic model in untreated adolescent idiopathic scoliosis using the simplified skeletal maturity system. Spine Deform 7:890–898.e4. https://doi.org/10.1016/j.jspd.2019.01.011
Sanders JO, Khoury JG, Kishan S et al (2008) Predicting scoliosis progression from skeletal maturity: A simplified classification during adolescence. J Bone Jt Surg 90:540–553. https://doi.org/10.2106/JBJS.G.00004
Nault ML, Mac-Thiong JM, Roy-Beaudry M et al (2014) Three-dimensional spinal morphology can differentiate between progressive and nonprogressive patients with adolescent idiopathic scoliosis at the initial presentation: A prospective study. Spine (Phila Pa 1976) 39:601–606. https://doi.org/10.1097/BRS.0000000000000284
Vergari C, Karam M, Pietton R et al (2020) Spine slenderness and wedging in adolescent idiopathic scoliosis and in asymptomatic population: An observational retrospective study. Eur Spine J 29:726–736. https://doi.org/10.1007/s00586-020-06340-8
Lindeman M, Behm K (1999) Cognitive strategies and self-esteem as predictors of brace-wear noncompliance in patients with idiopathic scoliosis and kyphosis. J Pediatr Orthop 19:493–499. https://doi.org/10.1097/00004694-199907000-00013
Illes T, Tunyogi-Csapo M, Somoskeoy S (2011) Breakthrough in three-dimensional scoliosis diagnosis: Significance of horizontal plane view and vertebra vectors. Eur Spine J 20:135–143. https://doi.org/10.1007/s00586-010-1566-8
Acknowledgements
The authors are grateful to the BiomecAM chair program on subject-specific musculoskeletal modelling (with the support of ParisTech and Yves Cotrel Foundations, Société Générale, Covea, and Proteor).
Funding
This study has received funding from the BiomecAM chair program on subject-specific musculoskeletal modelling (with the support of ParisTech and Yves Cotrel Foundations, Société Générale, Covea, and Proteor).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Wafa Skalli.
Conflict of interest
Dr. Skalli has a patent related to biplanar X-rays and associated 3D reconstruction methods, with no personal financial benefit (royalties rewarded for research and education) licensed to EOS Imaging. Dr. Vialle reports personal fees and grants (unrelated to this study) from EOS Imaging.
Statistics and biometry
Several authors have significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in:
- (N=55) Vergari et al, 2019: Quasi-automatic early detection of progressive idiopathic scoliosis from biplanar radiography a preliminary validation. European Spine Journal.
- (N=65) Skalli et al, 2017: Early detection of progressive adolescent idiopathic scoliosis a severity index. Spine.
Methodology
• prospective and retrospective
• diagnostic study
• multicenter study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vergari, C., Skalli, W., Abelin-Genevois, K. et al. Effect of curve location on the severity index for adolescent idiopathic scoliosis: a longitudinal cohort study. Eur Radiol 31, 8488–8497 (2021). https://doi.org/10.1007/s00330-021-07944-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-07944-4