Abstract
Objective
This study aimed to compare the cardiac function among different sub-types of pulmonary hypertension (PH) and to explore the independent predictors of major adverse cardiovascular events (MACE).
Methods
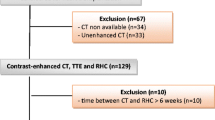
Eighty-seven PH patients diagnosed by right heart catheterization (RHC) were recruited. Patients underwent cardiac magnetic resonance (CMR) and RHC examination within 2 weeks. The CMR images were analyzed to calculate the cardiac functional parameters including right ventricle (RV) and left ventricle (LV) end-diastolic volume index (EDVI), end-systolic volume index (ESVI), stroke volume index (SVI), ejection fraction (EF), tricuspid annular plane systolic excursion (TAPSE), and myocardial mass (MM). The median follow-up time was 46.5 months (interquartile range: 26–65.5 months), and the endpoints were the occurrence of MACE.
Results
RVEDVI, LVEDVI, and LVESVI were higher in congenital heart disease–related PH (CHD-PH) than in other sub-types (p < 0.05). RVMM, RVSVI, and RVCI were highest in CHD-PH. There was no significant difference in the prognosis among different sub-types (p > 0.05). Comparing with the non-MACE group, RVEF, TAPSE, and LVSVI significantly decreased in the MACE group, while the RVESVI significantly increased (p < 0.05). TAPSE ≤ 15.65 mm and LVSVI ≤ 30.27 mL/m2 were significant independent predictors of prognosis in PH patients.
Conclusion
CHD-PH had a higher RV function reserve but lowest LVEF comparing to other subgroups. TAPSE and LVSVI could contribute to the prediction of MACE in PH patients.
Key Points
• CMR imaging is a noninvasive and accurate tool to assess ventricular function.
• CHD-PH had higher RV function reserve but lowest LVEF.
• TAPSE and LVSVI could contribute to the prediction of MACE in PH patients.





Similar content being viewed by others
Abbreviations
- BPA:
-
Balloon pulmonary angioplasty
- BSA:
-
Body surface area
- CHD:
-
Congenital heart disease
- CI:
-
Cardiac index
- CMR:
-
Cardiac magnetic resonance
- CO:
-
Cardiac output
- CTD:
-
Connective tissue disease
- CTEPH:
-
Chronic thromboembolic pulmonary hypertension
- dPAP:
-
Diastolic pulmonary arterial pressure
- ECG:
-
Electrocardiogram
- EDV:
-
End-diastolic volume
- EDVI:
-
End-diastolic volume index
- EF:
-
Ejection fraction
- ESV:
-
End-systolic volume
- ESVI:
-
End-systolic volume index
- FIESTA:
-
Fast imaging employing steady-state acquisition
- IPAH:
-
Idiopathic pulmonary arterial hypertension
- IVS:
-
Interventricular septum
- LV:
-
Left ventricle
- LVSB:
-
Leftward ventricular septal bowing
- MACE:
-
Major adverse cardiovascular events
- MM:
-
Myocardial mass
- MMI:
-
Myocardial mass index
- MPA:
-
Main pulmonary artery
- mPAP:
-
Mean pulmonary arterial pressure
- MRI:
-
Magnetic resonance imaging
- PAH:
-
Pulmonary arterial hypertension
- PAP:
-
Pulmonary arterial pressure
- PEA:
-
Pulmonary endarterectomy
- PH:
-
Pulmonary hypertension
- PVR:
-
Pulmonary vascular resistance
- RCI:
-
Right cardiac index
- RHC:
-
Right heart catheterization
- ROC:
-
Receiver operating characteristic
- RV:
-
Right ventricle
- sPAP:
-
Systolic pulmonary arterial pressure
- SV:
-
Stroke volume
- SVI:
-
Stroke volume index
- TAPSE:
-
Tricuspid annular plane systolic excursion
- TTE:
-
Transthoracic echocardiography
- WHO:
-
World Health Organization
References
Aluja Jaramillo F, Gutierrez FR, Diaz Telli FG, Yevenes Aravena S, Javidan-Nejad C, Bhalla S (2018) Approach to pulmonary hypertension: from CT to clinical diagnosis. Radiographics 38:357–373
Humbert M (2010) Pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension: pathophysiology. Eur Respir Rev 19:59–63
Escribano-Subias P, Blanco I, López-Meseguer M et al (2012) Survival in pulmonary hypertension in Spain: insights from the Spanish registry. Eur Respir J 40:596–603
Chung WJ, Park YB, Jeon CH et al (2015) Baseline characteristics of the Korean Registry of Pulmonary Arterial Hypertension. J Korean Med Sci 30:1429–1438
Zhang Z, Wang M, Yang Z et al (2017) Noninvasive prediction of pulmonary artery pressure and vascular resistance by using cardiac magnetic resonance indices. Int J Cardiol 227:915–922
Tedford RJ, Mudd JO, Girgis RE et al (2013) Right ventricular dysfunction in systemic sclerosis-associated pulmonary arterial hypertension. Circ Heart Fail 6:953–963
Overbeek MJ, Lankhaar JW, Westerhof N et al (2008) Right ventricular contractility in systemic sclerosis-associated and idiopathic pulmonary arterial hypertension. Eur Respir J 31:1160–1166
van de Veerdonk MC, Kind T, Marcus JT et al (2011) Progressive right ventricular dysfunction in patients with pulmonary arterial hypertension responding to therapy. J Am Coll Cardiol 58:2511–2519
Galie N, Humbert M, Vachiery JL et al (2016) 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: the Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J 37:67–119
Toro R, Cabeza-Letran ML, Quezada M, Rodriguez-Puras MJ, Mangas A (2016) Impaired right and left ventricular mechanics in adults with pulmonary hypertension and congenital shunts. J Cardiovasc Med 17:209–216
Gabriels C, Lancellotti P, Van De Bruaene A et al (2015) Clinical significance of dynamic pulmonary vascular resistance in two populations at risk of pulmonary arterial hypertension. Eur Heart J Cardiovasc Imaging 16:564–570
Pena E, Dennie C, Veinot J, Muniz SH (2012) Pulmonary hypertension: how the radiologist can help. Radiographics 32:9–32
Johnson RC, Datar SA, Oishi PE et al (2014) Adaptive right ventricular performance in response to acutely increased afterload in a lamb model of congenital heart disease: evidence for enhanced Anrep effect. Am J Physiol Heart Circ Physiol 306:H1222–H1230
Hopkins WE (2005) The remarkable right ventricle of patients with Eisenmenger syndrome. Coron Artery Dis 16:19–25
Li JH, Zhang HD, Wang ZZ et al (2018) Acute iloprost inhalation improves right ventricle function in pulmonary artery hypertension: a cardiac magnetic resonance study. Front Pharmacol 9:1550
Lambova S (2014) Cardiac manifestations in systemic sclerosis. World J Cardiol 6:993–1005
Hur DJ, Sugeng L (2019) Non-invasive multimodality cardiovascular imaging of the right heart and pulmonary circulation in pulmonary hypertension. Front Cardiovasc Med 6:24
Jensen AS, Broberg CS, Rydman R, et al (2015) Impaired right, left, or biventricular function and resting oxygen saturation are associated with mortality in Eisenmenger syndrome. Circ Cardiovasc Imaging 8
Sanz J, Sanchez-Quintana D, Bossone E, Bogaard HJ, Naeije R (2019) Anatomy, function, and dysfunction of the right ventricle: JACC State-of-the-Art Review. J Am Coll Cardiol 73:1463–1482
Hoette S, Creuze N, Gunther S et al (2018) RV fractional area change and TAPSE as predictors of severe right ventricular dysfunction in pulmonary hypertension: a CMR study. Lung 196:157–164
Palau-Caballero G, Walmsley J, Van Empel V, Lumens J, Delhaas T (2017) Why septal motion is a marker of right ventricular failure in pulmonary arterial hypertension: mechanistic analysis using a computer model. Am J Physiol Heart Circ Physiol 312:H691–H700
Hardziyenka M, Campian ME, Reesink HJ et al (2011) Right ventricular failure following chronic pressure overload is associated with reduction in left ventricular mass. J Am Coll Cardiol 57:921–928
Murata M, Tsugu T, Kawakami T et al (2016) Prognostic value of three-dimensional echocardiographic right ventricular ejection fraction in patients with pulmonary arterial hypertension. Oncotarget 7:86781–86790
Swift AJ, Rajaram S, Campbell MJ et al (2014) Prognostic value of cardiovascular magnetic resonance imaging measurements corrected for age and sex in idiopathic pulmonary arterial hypertension. Circ Cardiovasc Imaging 7:100–106
Mathai SC, Sibley CT, Forfia PR et al (2011) Tricuspid annular plane systolic excursion is a robust outcome measure in systemic sclerosis-associated pulmonary arterial hypertension. J Rheumatol 38:2410–2418
Ghio S, Klersy C, Magrini G et al (2010) Prognostic relevance of the echocardiographic assessment of right ventricular function in patients with idiopathic pulmonary arterial hypertension. Int J Cardiol 140:272–278
Rushmer RF, Crystal DK, Wagner C (1953) The functional anatomy of ventricular contraction. Circ Res 1:162–170
Carlsson M, Ugander M, Heiberg E, Arheden H (2007) The quantitative relationship between longitudinal and radial function in left, right, and total heart pumping in humans. Am J Physiol Heart Circ Physiol 293:H636–H644
Kovacs A, Lakatos B, Tokodi M, Merkely B (2019) Right ventricular mechanical pattern in health and disease: beyond longitudinal shortening. Heart Fail Rev 24:511–520
Li Y, Wang Y, Yang Y et al (2018) Tricuspid annular displacement measured by 2-dimensional speckle tracking echocardiography for predicting right ventricular function in pulmonary hypertension: a new approach to evaluating right ventricle dysfunction. Medicine (Baltimore) 97:e11710
Forfia PR, Fisher MR, Mathai SC et al (2006) Tricuspid annular displacement predicts survival in pulmonary hypertension. Am J Respir Crit Care Med 174:1034–1041
Corona-Villalobos CP, Kamel IR, Rastegar N et al (2015) Bidimensional measurements of right ventricular function for prediction of survival in patients with pulmonary hypertension: comparison of reproducibility and time of analysis with volumetric cardiac magnetic resonance imaging analysis. Pulm Circ 5:527–537
Ho SY, Nihoyannopoulos P (2006) Anatomy, echocardiography, and normal right ventricular dimensions. Heart 92(Suppl 1):i2–i13
Egemnazarov B, Crnkovic S, Nagy BM, Olschewski H, Kwapiszewska G (2018) Right ventricular fibrosis and dysfunction: Actual concepts and common misconceptions. Matrix Biol 68-69:507–521
Peacock AJ, Crawley S, McLure L et al (2014) Changes in right ventricular function measured by cardiac magnetic resonance imaging in patients receiving pulmonary arterial hypertension-targeted therapy: the EURO-MR study. Circ Cardiovasc Imaging 7:107–114
Knight DS, Steeden JA, Moledina S, Jones A, Coghlan JG, Muthurangu V (2015) Left ventricular diastolic dysfunction in pulmonary hypertension predicts functional capacity and clinical worsening: a tissue phase mapping study. J Cardiovasc Magn Reson 17:116
Funding
This study has received funding from the National Natural Science Youth Science Fund Project Foundation of China (81301217), Tianjin Key Project of Applied Basic and Frontier Technology Research Program (14JCZDJC57000), and “13th Fiver-Year Plan” National key R&D projects (2016YFC1300402).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dong Li.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 28 kb)
Rights and permissions
About this article
Cite this article
Ren, W., Guo, JJ., Yang, F. et al. Indication of the prognosis of pulmonary hypertension by using CMR function parameters. Eur Radiol 31, 7121–7131 (2021). https://doi.org/10.1007/s00330-021-07835-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-07835-8