Abstract
Objectives
To compare image quality and radiation dose between dual-energy subtraction (DES)–based bone suppression images (D-BSIs) and software-based bone suppression images (S-BSIs).
Methods
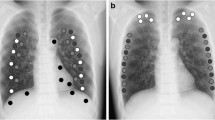
Chest radiographs (CXRs) of forty adult patients were obtained with the two X-ray devices, one with DES and one with bone suppression software. Three image quality metrics (relative mean absolute error (RMAE), peak signal-to-noise ratio (PSNR), and structural similarity index (SSIM)) between original CXR and BSI for each of D-BSI and S-SBI groups were calculated for each bone and soft tissue areas. Two readers rated the visual image quality for original CXR and BSI for each of D-BSI and S-SBI groups. The dose area product (DAP) values were recorded. Paired t test was used to compare the image quality and DAP values between D-BSI and S-BSI groups.
Results
In bone areas, S-BSIs had better SSIM values than D-BSI (94.57 vs. 87.77) but worse RMAE and PSNR values (0.50 vs. 0.20; 20.93 vs. 34.37) (all p < 0.001). In soft tissue areas, S-BSIs had better SSIM values than D-BSI (97.56 vs. 91.42) but similar RMAE and PSNR values (0.29 vs. 0.27; 31.35 vs. 29.87) (all p < 0.001). Both readers gave S-BSIs significantly higher image quality scores than D-BSI (p < 0.001). The mean DAP in software-related images (0.98 dGy·cm2) was significantly lower than that in the DES-related images (1.48 dGy·cm2) (p < 0.001).
Conclusion
Bone suppression software significantly improved the image quality of bone suppression images with a relatively lower radiation dose, compared with dual-energy subtraction technique.
Key Points
• Bone suppression software preserves structure similarity of soft tissues better than dual-energy subtraction technique in bone suppression images.
• Bone suppression software achieves superior image quality for lung lesions than dual-energy subtraction technique in bone suppression images.
• Bone suppression software can decrease the radiation dose over the hardware-based image processing technique.






Similar content being viewed by others
Change history
21 January 2020
The Supplementary Information file has been exchanged.
Abbreviations
- aPSNR:
-
Adjusted value of peak signal-to-noise ratio
- aRMAE:
-
Adjusted value of relative mean absolute error
- aSSIM:
-
Adjusted value of structural similarity index
- BSI:
-
Bone suppression image
- CXR:
-
Chest radiograph
- DAP:
-
Dose area product
- D-BSI:
-
Dual-energy subtraction-based bone suppression images
- DES:
-
Dual-energy subtraction
- PSNR:
-
Peak signal-to-noise ratio
- RMAE:
-
Relative mean absolute error
- S-BSI:
-
Software-based bone suppression images
- SSIM:
-
Structural similarity index
References
Li F, Engelmann R, Doi K, MacMahon H (2008) Improved detection of small lung cancers with dual-energy subtraction chest radiography. AJR Am J Roentgenol 190:886–891
MacMahon H, Li F, Engelmann R, Roberts R, Armato S (2008) Dual energy subtraction and temporal subtraction chest radiography. J Thorac Imaging 23:77–85
Oda S, Awai K, Funama Y et al (2010) Detection of small pulmonary nodules on chest radiographs: efficacy of dual-energy subtraction technique using flat-panel detector chest radiography. Clin Radiol 65:609–615
Szucs-Farkas Z, Schick A, Cullmann JL et al (2013) Comparison of dual-energy subtraction and electronic bone suppression combined with computer-aided detection on chest radiographs: effect on human observers’ performance in nodule detection. AJR Am J Roentgenol 200:1006–1013
Schalekamp S, van Ginneken B, Koedam E et al (2014) Computer-aided detection improves detection of pulmonary nodules in chest radiographs beyond the support by bone-suppressed images. Radiology 272:252–261
Urbaneja A, Dodin G, Hossu G et al (2018) Added value of bone subtraction in dual-energy digital radiography in the detection of pneumothorax: impact of reader expertise and medical specialty. Acad Radiol 25:82–87
Li F, Engelmann R, Pesce LL, Doi K, Metz CE, MacMahon H (2011) Small lung cancers: improved detection by use of bone suppression imaging—comparison with dual-energy subtraction chest radiography. Radiology 261:937–949
Li F, Engelmann R, Pesce L, Armato SG, MacMahon H (2012) Improved detection of focal pneumonia by chest radiography with bone suppression imaging. Eur Radiol 22:2729–2735
Schalekamp S, Karssemeijer N, Cats AM et al (2016) The effect of supplementary bone-suppressed chest radiographs on the assessment of a variety of common pulmonary abnormalities. J Thorac Imaging 31:119–125
Kodama N, Van Loc T, Hai PT et al (2018) Effectiveness of bone suppression imaging in the diagnosis of tuberculosis from chest radiographs in Vietnam: an observer study. Clin Imaging 51:196–201
Hong G-S, Do K-H, Lee CW (2019) Added value of bone suppression image in the detection of subtle lung lesions on chest radiographs with regard to reader’s expertise. J Korean Med Sci 34:e250
Fischbach F, Freund T, Röttgen R, Engert U, Felix R, Ricke J (2003) Dual-energy chest radiography with a flat-panel digital detector: revealing calcified chest abnormalities. AJR Am J Roentgenol 181:1519–1524
Kuhlman JE, Collins J, Brooks GN, Yandow DR, Broderick LS (2006) Dual-energy subtraction chest radiography: what to look for beyond calcified nodules. Radiographics 26:79–92
Oda S, Awai K, Suzuki K et al (2009) Performance of radiologists in detection of small pulmonary nodules on chest radiographs: effect of rib suppression with a massive-training artificial neural network. AJR Am J Roentgenol 193:W397–W402
Freedman MT, Lo S-CB, Seibel JC, Bromley CM (2011) Lung nodules: improved detection with software that suppresses the rib and clavicle on chest radiographs. Radiology 260:265–273
Schalekamp S, van Ginneken B, Meiss L et al (2013) Bone suppressed images improve radiologists’ detection performance for pulmonary nodules in chest radiographs. Eur J Radiol 82:2399–2405
Miyoshi T, Yoshida J, Aramaki N et al (2017) Effectiveness of bone suppression imaging in the detection of lung nodules on chest radiographs. J Thorac Imaging 32:398–405
Li F, Hara T, Shiraishi J, Engelmann R, MacMahon H, Doi K (2011) Improved detection of subtle lung nodules by use of chest radiographs with bone suppression imaging: receiver operating characteristic analysis with and without localization. AJR Am J Roentgenol 196:W535–W541
Chen Y, Gou X, Feng X et al (2019) Bone suppression of chest radiographs with cascaded convolutional networks in wavelet domain. IEEE Access 7:8346–8357
De Crop A, Bacher K, Van Hoof T et al (2012) Correlation of contrast-detail analysis and clinical image quality assessment in chest radiography with a human cadaver study. Radiology 262:298–304
Wang Z, Bovik AC, Sheikh HR, Simoncelli EP (2004) Image quality assessment: from error visibility to structural similarity. IEEE Trans Image Process 13:600–612
Oh DY, Yun ID (2018) Learning bone suppression from dual energy chest X-rays using adversarial networks. arXiv preprint arXiv:1811.02628
Liang J, Tang Y-X, Tang Y-B, Xiao J, Summers RM (2020) Bone suppression on chest radiographs with adversarial learning. Medical imaging: computer-aided diagnosis 1131409
Matsubara N, Teramoto A, Saito K, Fujita H (2020) Bone suppression for chest X-ray image using a convolutional neural filter. Phys Eng Sci Med 43:97–108
Wang Z, Bovik AC (2002) A universal image quality index. IEEE Signal Process Lett 9:81–84
Wang Z, Bovik AC (2002) Why is image quality assessment so difficult? In Proceedings of IEEE international conference on acoustics, speech, and signal processing (ICASSP) 4:3313–3316
Moorthy AK, Wang Z, Bovik AC (2011) Visual perception and quality assessment. In: Cristobal G, Schelkens P, Thienpont H (eds) Optical and digital image processing, 1st edn. Wiley-VCH, Weinheim, p419–439
Brooks AC, Zhao X, Pappas TN (2008) Structural similarity quality metrics in a coding context: exploring the space of realistic distortions. IEEE Trans Image Process 17:1261–1273
MacMahon H, Engelmann R, Behlen FM et al (1999) Computer-aided diagnosis of pulmonary nodules: results of a large-scale observer test. Radiology 213:723–726
Quekel LG, Kessels AG, Goei R, van Engelshoven JM (2001) Detection of lung cancer on the chest radiograph: a study on observer performance. Eur J Radiol 39:111–116
Monnier-Cholley L, Carrat F, Cholley BP, Tubiana J-M, Arrivé L (2004) Detection of lung cancer on radiographs: receiver operating characteristic analyses of radiologists’, pulmonologists’, and anesthesiologists’ performance. Radiology 233:799–805
Acknowledgments
The authors are grateful to Jooae Choe, MD, Hye Jeon Hwang, MD, and Eun Young Kim, MD, for participating as readers.
Funding
This study has received funding by Samsung Electronics Co., Ltd.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Kyung-Hyun Do, MD, PhD.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
This prospective study was conducted according to the principles of the Declaration of Helsinki. The study protocol was approved by the Institutional Review Board Committee of the Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea (No. 2018-1348).
Methodology
• prospective
• case-control study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 133 kb)
Rights and permissions
About this article
Cite this article
Hong, GS., Do, KH., Son, AY. et al. Value of bone suppression software in chest radiographs for improving image quality and reducing radiation dose. Eur Radiol 31, 5160–5171 (2021). https://doi.org/10.1007/s00330-020-07596-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07596-w