Abstract
Objectives
To establish a prediction model for evaluating the axillary lymph node (ALN) status of patients with T1/T2 invasive breast cancer based on radiomics analysis of US images of primary breast lesions.
Methods
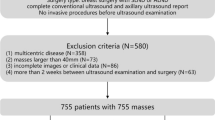
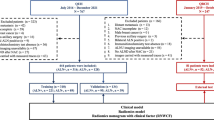
Between August 2016 and November 2018, a total of 343 patients with histologically proven malignant breast tumors were included in this study and randomly assigned to the training and validation groups at a ratio of 7:3. ALN tumor burden was defined as low (< 3 metastatic ALNs) or high (≥ 3 metastatic ALNs). Radiomics features were obtained using the PyRadiomics package, and the radiomics score was established by least absolute shrinkage and selection operator regression. A nomogram combining the breast cancer US radiomics score with patient age and lesion size was generated based on the multivariate logistic regression results.
Results
In the training and validation cohorts, 29.1% (69/237) and 32.08% (34/106) of patients were pathologically diagnosed with more than 2 metastatic ALNs, respectively. The radiomics score consisted of 16 US features, and patient age and lesion diameter identified by US were included to construct the model. The AUC of the model was 0.846 (95% CI, 0.790–0.902) for the training cohort and 0.733 (95% CI, 0.613–0.852) for the validation cohort. The calibration curves showed good agreement between the predictions and observations.
Conclusions
Our novel nomogram demonstrates high accuracy in predicting ALN tumor burden in breast cancer patients. We also suggest further development of PyRadiomics to improve US radiomics.
Key Points
• A nomogram based on US was developed to predict ALN tumor burden (low, < 3 metastatic ALNs; high, ≥ 3 metastatic ALNs).
• The nomogram could assist clinicians in evaluating treatment strategies for T1/T2 invasive breast cancer.






Similar content being viewed by others
Abbreviations
- 2D:
-
Two-dimensional
- ALN:
-
Axillary lymph node
- ALND:
-
Axillary lymph node dissection
- ASCO:
-
American Society of Clinical Oncology
- LASSO:
-
Least absolute shrinkage and selection operator
- SLNB:
-
Sentinel lymph node biopsy
- VIF:
-
Variance inflation factor
References
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM (2010) Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 127:2893–2917
Zuo TT, Zheng RS, Zeng HM, Zhang SW, Chen WQ (2017) Female breast cancer incidence and mortality in China, 2013. Thorac Cancer 8:214–218
DeSantis C, Ma J, Bryan L, Jemal A (2014) Breast cancer statistics, 2013. CA Cancer J Clin 64:52–62
Harbeck N, Gnant M (2017) Breast cancer. Lancet 389:1134–1150
Rao R, Euhus D, Mayo HG, Balch C (2013) Axillary node interventions in breast cancer: a systematic review. JAMA 310:1385–1394
Lucci A, McCall LM, Beitsch PD et al (2007) Surgical complications associated with sentinel lymph node dissection (SLND) plus axillary lymph node dissection compared with SLND alone in the American College of Surgeons Oncology Group Trial Z0011. J Clin Oncol 25:3657–3663
Abass MO, Gismalla MDA, Alsheikh AA, Elhassan MMA (2018) Axillary lymph node dissection for breast cancer: efficacy and complication in developing countries. J Glob Oncol 4:1–8
Manca G, Rubello D, Tardelli E et al (2016) Sentinel lymph node biopsy in breast cancer: indications, contraindications, and controversies. Clin Nucl Med 41:126–133
Giuliano AE, Ballman KV, McCall L et al (2017) Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (Alliance) randomized clinical trial. JAMA 318:918–926
Lyman GH, Somerfield MR, Bosserman LD, Perkins CL, Weaver DL, Giuliano AE (2017) Sentinel lymph node biopsy for patients with early-stage breast cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 35:561–564
Valente SA, Levine GM, Silverstein MJ et al (2012) Accuracy of predicting axillary lymph node positivity by physical examination, mammography, ultrasonography, and magnetic resonance imaging. Ann Surg Oncol 19:1825–1830
Alvarez S, Anorbe E, Alcorta P, Lopez F, Alonso I, Cortes J (2006) Role of sonography in the diagnosis of axillary lymph node metastases in breast cancer: a systematic review. AJR Am J Roentgenol 186:1342–1348
Engohan-Aloghe C, Hottat N, Noel JC (2010) Accuracy of lymph nodes cell block preparation according to ultrasound features in preoperative staging of breast cancer. Diagn Cytopathol 38:5–8
Cools-Lartigue J, Meterissian S (2012) Accuracy of axillary ultrasound in the diagnosis of nodal metastasis in invasive breast cancer: a review. World J Surg 36:46–54
Chen X, He Y, Wang J et al (2018) Feasibility of using negative ultrasonography results of axillary lymph nodes to predict sentinel lymph node metastasis in breast cancer patients. Cancer Med. https://doi.org/10.1002/cam4.1606
Zhu Y, Zhou W, Jia XH, Huang O, Zhan WW (2018) Preoperative axillary ultrasound in the selection of patients with a heavy axillary tumor burden in early-stage breast cancer: what leads to false-positive results? J Ultrasound Med 37:1357–1365
Ahmed M, Jozsa F, Baker R, Rubio IT, Benson J, Douek M (2017) Meta-analysis of tumour burden in pre-operative axillary ultrasound positive and negative breast cancer patients. Breast Cancer Res Treat 166:329–336
Gillies RJ, Kinahan PE, Hricak H (2016) Radiomics: images are more than pictures, they are data. Radiology 278:563–577
Lambin P, Leijenaar RTH, Deist TM et al (2017) Radiomics: the bridge between medical imaging and personalized medicine. Nat Rev Clin Oncol 14:749–762
Valdora F, Houssami N, Rossi F, Calabrese M, Tagliafico AS (2018) Rapid review: radiomics and breast cancer. Breast Cancer Res Treat 169:217–229
Carter CL, Allen C, Henson DE (1989) Relation of tumor size, lymph node status, and survival in 24,740 breast cancer cases. Cancer 63:181–187
Weigel MT, Dowsett M (2010) Current and emerging biomarkers in breast cancer: prognosis and prediction. Endocr Relat Cancer 17:R245–R262
Giuliano AE, Barth AM, Spivack B, Beitsch PD, Evans SW (1996) Incidence and predictors of axillary metastasis in T1 carcinoma of the breast. J Am Coll Surg 183:185–189
Hu HT, Wang Z, Huang XW et al (2019) Ultrasound-based radiomics score: a potential biomarker for the prediction of microvascular invasion in hepatocellular carcinoma. Eur Radiol 29:2890–2901
Qiu SQ, Zeng HC, Zhang F et al (2016) A nomogram to predict the probability of axillary lymph node metastasis in early breast cancer patients with positive axillary ultrasound. Sci Rep 6:21196
Xie X, Tan W, Chen B et al (2018) Preoperative prediction nomogram based on primary tumor miRNAs signature and clinical-related features for axillary lymph node metastasis in early-stage invasive breast cancer. Int J Cancer 142:1901–1910
Yu FH, Wang JX, Ye XH, Deng J, Hang J, Yang B (2019) Ultrasound-based radiomics nomogram: a potential biomarker to predict axillary lymph node metastasis in early-stage invasive breast cancer. Eur J Radiol 119:108658
van Griethuysen JJM, Fedorov A, Parmar C et al (2017) Computational radiomics system to decode the radiographic phenotype. Cancer Res 77:e104–e107
Tibshirani R (1996) Regression shrinkage and selection via the lasso. J R Stat Soc B 58:267–288
Meretoja TJ, Heikkila PS, Mansfield AS et al (2014) A predictive tool to estimate the risk of axillary metastases in breast cancer patients with negative axillary ultrasound. Ann Surg Oncol 21:2229–2236
Rizzo S, Botta F, Raimondi S et al (2018) Radiomics: the facts and the challenges of image analysis. Eur Radiol Exp 2:36
Brattain LJ, Telfer BA, Dhyani M, Grajo JR, Samir AE (2018) Machine learning for medical ultrasound: status, methods, and future opportunities. Abdom Radiol (NY) 43:786–799
Veeraraghavan H, Dashevsky BZ, Onishi N et al (2018) Appearance constrained semi-automatic segmentation from DCE-MRI is reproducible and feasible for breast cancer radiomics: a feasibility study. Sci Rep 8:4838
Acknowledgments
We thank Rui Liu for his suggestion on application of PyRadiomics.
Funding
This study has received funding by Special Fund for National Natural Sciences Foundation of China (81771855) and CAMS Innovation Fund for Medical Sciences (2017-I2M-1-006).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Qingli Zhu and Yuxin Jiang.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the institutional review board.
Ethical approval
Institutional review board approval was obtained.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 16 kb)
Rights and permissions
About this article
Cite this article
Gao, Y., Luo, Y., Zhao, C. et al. Nomogram based on radiomics analysis of primary breast cancer ultrasound images: prediction of axillary lymph node tumor burden in patients. Eur Radiol 31, 928–937 (2021). https://doi.org/10.1007/s00330-020-07181-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07181-1