Abstract
Objectives
To develop a nomogram based on postoperative clinical and ultrasound findings to quantify the probability of central compartment lymph node metastases (CLNM).
Methods
A total of 952 patients with histologically confirmed papillary thyroid carcinoma (PTC) were included in this retrospective study and assigned to three groups based on sex and age. The strongest predictors for CLNM were selected according to ultrasound imaging features, and an ultrasound (US) signature was constructed. By incorporating clinical characteristics, a predictive model presented as a nomogram was developed, and its performance was assessed with respect to calibration, discrimination and clinical usefulness.
Results
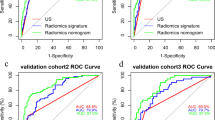
Predictors contained in the nomogram included US signature, US-reported LN status and age. The US signature was constructed with tumour size and microcalcification. The nomogram showed excellent calibration in the training dataset, with an AUC of 0.826 (95% CI, 0.765–0.887) for male patients, 0.818 (95% CI, 0.746–0.890) for young females and 0.808 (95% CI, 0.757–0.859) for elder females. For male and young female patients, application of the nomogram to the validation cohort revealed good discrimination, with AUCs of 0.813 (95% CI, 0.722–0.904) and 0.814 (95% CI, 0.712–0.915), respectively. Conversely, for elderly female patients, the nomogram failed to show good performance with an AUC of 0.742 (95% CI, 0.661–0.823).
Conclusion
This ultrasound-based nomogram may serve as a useful clinical tool to provide valuable information for treatment decisions, especially for male and younger female patients.
Key Points
• Age, gender, US-reported LN status and US signature were the strongest predictors of CLNM in PTC patients and informed the development of a predictive nomogram.
• Microcalcification was the strongest predictor in the US signature, as CLMN was identified in approximately 92% of patients characterised by diffuse microcalcification.
• Stratified by sex and age, this nomogram achieved good performance in predicting CLNM, especially in male and young female patients. This prediction tool may be useful as an imaging marker for identifying CLNM preoperatively in PTC patients and as a guide for personalised treatment.






Similar content being viewed by others
Abbreviations
- ATA:
-
American Thyroid Association
- CI:
-
Confidence interval
- CLND:
-
Central compartment lymph node dissection
- CLNM:
-
Central compartment lymph node metastases
- LASSO:
-
Least absolute shrinkage and selection operator
- LN:
-
Lymph node
- PTC:
-
Papillary thyroid carcinoma
References
Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin 69:7–34
Lee YK, Hong N, Park SH et al (2019) The relationship of comorbidities to mortality and cause of death in patients with differentiated thyroid carcinoma. Sci Rep 9:11435
Zhao L, Pang P, Zang L et al (2019) Features and trends of thyroid cancer in patients with thyroidectomies in Beijing, China between 1994 and 2015: a retrospective study. BMJ Open 9:e023334
Wu X, Li B, Zheng C, He X (2018) Risk factors for central lymph node metastases in patients with papillary microcarcinoma. Endocr Pract 24:1057–1062
Xu Y, Xu L, Wang J (2018) Clinical predictors of lymph node metastasis and survival rate in papillary thyroid microcarcinoma: analysis of 3607 patients at a single institution. J Surg Res 221:128–134
Feng JW, Yang XH, Wu BQ, Sun DL, Jiang Y, Qu Z (2019) Predictive factors for central lymph node and lateral cervical lymph node metastases in papillary thyroid carcinoma. Clin Transl Oncol. https://doi.org/10.1007/s12094-019-02076-0
Lee J, Song Y, Soh EY (2014) Central lymph node metastasis is an important prognostic factor in patients with papillary thyroid microcarcinoma. J Korean Med Sci 29:48–52
Haugen BR, Alexander EK, Bible KC et al (2016) 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 26:1–133
Conzo G, Tartaglia E, Avenia N et al (2016) Role of prophylactic central compartment lymph node dissection in clinically N0 differentiated thyroid cancer patients: analysis of risk factors and review of modern trends. World J Surg Oncol 14:149
Michalaki M, Bountouris P, Roupas ND et al (2016) Low-risk papillary thyroid carcinoma patients who underwent near-total thyroidectomy without prophylactic central compartment lymph node dissection and were ablated with low-dose 50mCi RAI had excellent 10-year prognosis. Hormones (Athens) 15:511–517
Ito Y, Miyauchi A, Kudo T, Kihara M, Fukushima M, Miya A (2017) The effectiveness of prophylactic modified neck dissection for reducing the development of lymph node recurrence of papillary thyroid carcinoma. World J Surg 41:2283–2289
Viola D, Materazzi G, Valerio L et al (2015) Prophylactic central compartment lymph node dissection in papillary thyroid carcinoma: clinical implications derived from the first prospective randomized controlled single institution study. J Clin Endocrinol Metab 100:1316–1324
Aydin OU, Soylu L, Ozbas S et al (2016) The risk of hypoparathyroidism after central compartment lymph node dissection in the surgical treatment of pT1, N0 thyroid papillary carcinoma. Eur Rev Med Pharmacol Sci 20:1781–1787
Takami H, Ito Y, Okamoto T, Onoda N, Noguchi H, Yoshida A (2014) Revisiting the guidelines issued by the Japanese Society of Thyroid Surgeons and Japan Association of endocrine surgeons: a gradual move towards consensus between Japanese and western practice in the management of thyroid carcinoma. World J Surg 38:2002–2010
Cho SJ, Suh CH, Baek JH, Chung SR, Choi YJ, Lee JH (2019) Diagnostic performance of CT in detection of metastatic cervical lymph nodes in patients with thyroid cancer: a systematic review and meta-analysis. Eur Radiol 29:4635–4647
Lee DH, Kim YK, Yu HW, Choi JY, Park SY, Moon JH (2019) Computed tomography (CT) for detecting cervical lymph node metastasis in patients who have papillary thyroid microcarcinoma with tumor characteristics appropriate for active surveillance. Thyroid. https://doi.org/10.1089/thy.2019.0100
Liu Z, Xun X, Wang Y et al (2014) MRI and ultrasonography detection of cervical lymph node metastases in differentiated thyroid carcinoma before reoperation. Am J Transl Res 6(2):147–154
Hwang HS, Orloff LA (2011) Efficacy of preoperative neck ultrasound in the detection of cervical lymph node metastasis from thyroid cancer. Laryngoscope 121:487–491
Stulak JM, Grant CS, Farley DR et al (2006) Value of preoperative ultrasonography in the surgical management of initial and reoperative papillary thyroid cancer. Arch Surg 141:489–494 discussion 494-496
Yeh MW, Bauer AJ, Bernet VA et al (2015) American Thyroid Association statement on preoperative imaging for thyroid cancer surgery. Thyroid 25:3–14
Siddiqui S, White MG, Antic T et al (2016) Clinical and pathologic predictors of lymph node metastasis and recurrence in papillary thyroid microcarcinoma. Thyroid 26:807–815
Wang Y, Guan Q, Xiang J (2018) Nomogram for predicting central lymph node metastasis in papillary thyroid microcarcinoma: a retrospective cohort study of 8668 patients. Int J Surg 55:98–102
Nie X, Tan Z, Ge M (2017) Skip metastasis in papillary thyroid carcinoma is difficult to predict in clinical practice. BMC Cancer 17:702
Adler DD, Carson PL, Rubin JM, Quinn-Reid D (1990) Doppler ultrasound color flow imaging in the study of breast cancer: preliminary findings. Ultrasound Med Biol 16:553–559
Fisher SB, Perrier ND (2018) The incidental thyroid nodule. CA Cancer J Clin 68:97–105
Wu LM, Gu HY, Qu XH et al (2012) The accuracy of ultrasonography in the preoperative diagnosis of cervical lymph node metastases in patients with papillary thyroid carcinoma: a meta-analysis. Eur J Radiol 81:1798–1805
Sauerbrei W, Royston P, Binder H (2007) Selection of important variables and determination of functional form for continuous predictors in multivariable model building. Stat Med 26:5512–5528
Kramer AA, Zimmerman JE (2007) Assessing the calibration of mortality benchmarks in critical care: the Hosmer-Lemeshow test revisited. Crit Care Med 35:2052–2056
Thompson AM, Turner RM, Hayen A et al (2014) A preoperative nomogram for the prediction of ipsilateral central compartment lymph node metastases in papillary thyroid cancer. Thyroid 24:675–682
Oh HS, Park S, Kim M et al (2017) Young age and male sex are predictors of large-volume central neck lymph node metastasis in clinical N0 papillary thyroid microcarcinomas. Thyroid 27:1285–1290
Xu SY, Yao JJ, Zhou W, Chen L, Zhan WW (2019) Clinical characteristics and ultrasonographic features for predicting central lymph node metastasis in clinically node-negative papillary thyroid carcinoma without capsule invasion. Head Neck 41:3984–3991
Ito Y, Miyauchi A, Kihara M, Higashiyama T, Kobayashi K, Miya A (2014) Patient age is significantly related to the progression of papillary microcarcinoma of the thyroid under observation. Thyroid 24:27–34
Wang F, Zhao S, Shen X et al (2018) BRAF V600E confers male sex disease-specific mortality risk in patients with papillary thyroid cancer. J Clin Oncol 36:2787–2795
Al Afif A, Williams BA, Rigby MH et al (2015) Multifocal papillary thyroid cancer increases the risk of central lymph node metastasis. Thyroid 25:1008–1012
Huang XP, Ye TT, Zhang L et al (2018) Sonographic features of papillary thyroid microcarcinoma predicting high-volume central neck lymph node metastasis. Surg Oncol 27:172–176
Zhao L, Yan H, Pang P et al (2019) Thyroid nodule size calculated using ultrasound and gross pathology as predictors of cancer: a 23-year retrospective study. Diagn Cytopathol 47:187–193
Bai Y, Zhou G, Nakamura M et al (2009) Survival impact of psammoma body, stromal calcification, and bone formation in papillary thyroid carcinoma. Mod Pathol 22:887–894
Ferreira LB, Lima RT, Bastos A et al (2018) OPNa overexpression is associated with matrix calcification in thyroid cancer cell lines. Int J Mol Sci. https://doi.org/10.3390/ijms19102990
Pyo JS, Kang G, Kim DH, Park C, Kim JH, Sohn JH (2013) The prognostic relevance of psammoma bodies and ultrasonographic intratumoral calcifications in papillary thyroid carcinoma. World J Surg 37:2330–2335
Jang JY, Kim DS, Park HY et al (2019) Preoperative serum VEGF-C but not VEGF-A level is correlated with lateral neck metastasis in papillary thyroid carcinoma. Head Neck 41:2602–2609
Tu DG, Chang WW, Jan MS, Tu CW, Lu YC, Tai CK (2016) Promotion of metastasis of thyroid cancer cells via NRP-2-mediated induction. Oncol Lett 12:4224–4230
Vickers AJ, Cronin AM, Elkin EB, Gonen M (2008) Extensions to decision curve analysis, a novel method for evaluating diagnostic tests, prediction models and molecular markers. BMC Med Inform Decis Mak 8:53
Xu JM, Xu XH, Xu HX et al (2016) Prediction of cervical lymph node metastasis in patients with papillary thyroid cancer using combined conventional ultrasound, strain elastography, and acoustic radiation force impulse (ARFI) elastography. Eur Radiol 26:2611–2622
Lee JH, Ha EJ, Kim JH (2019) Application of deep learning to the diagnosis of cervical lymph node metastasis from thyroid cancer with CT. Eur Radiol 29:5452–5457
Acknowledgements
The National Natural Science Foundation of China (NSFC), the Natural Science Foundation of Beijing, China (BJNSF) and the Innovation Cultivation Fund Project of the Seventh Medical Center of the PLA General Hospital are gratefully acknowledged. Yukun Luo, Qing Song, Ling Ren, Ying Zhang, Fang Xie, Yan Zhang, Jie Tang, Yaqiong Zhu and Zhuang Jin are gratefully acknowledged.
Funding
This study received funding from the National Natural Science Foundation of China (81771834 and 81901746); the Natural Science Foundation of Beijing, China (7194318); and the Innovation Cultivation Fund Project of the Seventh Medical Center of the PLA General Hospital (2015-LC-05).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Yukun Luo.
Conflict of interest
The authors of this manuscript declare no relationship with any company whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• Diagnostic or prognostic study
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Tian, X., Song, Q., Xie, F. et al. Papillary thyroid carcinoma: an ultrasound-based nomogram improves the prediction of lymph node metastases in the central compartment. Eur Radiol 30, 5881–5893 (2020). https://doi.org/10.1007/s00330-020-06906-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-06906-6