Abstract
Objectives
Magnetic resonance imaging (MRI) aids diagnosis in cystic fibrosis (CF) but its use in quantitative severity assessment is under research. This study aims to assess changes in signal intensity (SI) and lung volumes (Vol) during functional MRI and their use as a severity assessment tool in CF patients.
Methods
The CF intra-hospital standard chest 1.5 T MRI protocol comprises of very short echo-time sequences in submaximal in- and expiration for functional information. Quantitative measurements (Vol/SI at in- and expiration, relative differences (Vol_delta/SI_delta), and cumulative histograms for normalized SI values across the expiratory lung volume) were assessed for correlation to pulmonary function: lung clearance index (LCI) and forced expiratory volume in 1 s (FEV1).
Results
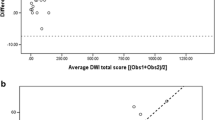
In 49 patients (26 male, mean age 17 ± 7 years) significant correlation of Vol_delta and SI_delta (R = 0.86; p < 0.0001) during respiration was observed. Individual cumulated histograms enabled severity disease differentiation (mild, severe) to be visualized (defined by functional parameter: LCI > 10). The expiratory volume at a relative SI of 100% correlated significantly to LCI (R = 0.676 and 0.627; p < 0.0001) and FEV1 (R = − 0.847 and − 0.807; p < 0.0001). Clustering patients according to Vol_SI_100 showed that an amount of ≤ 4% was related to normal, while an amount of > 4% was associated with pathological pulmonary function values.
Conclusion
Functional pulmonary MRI provides a radiation-free severity assessment tool and can contribute to early detection of lung impairment in CF. Lung volume with SI below 100% of the inspiratory volume represents overinflated tissue; an amount of 4% of the expiratory lung volume was a relevant turning point.
Key Points
• Signal intensity and lung volumes are used as potential metric parameters for lung impairment.
• Quantification of trapped air impacts on therapy management.
• Functional pulmonary MRI can contribute to early detection of lung impairment.




Similar content being viewed by others
Abbreviations
- CF:
-
Cystic fibrosis
- CT:
-
Computer tomography
- FEV1 :
-
Forced expiratory volume in 1 s
- LCI:
-
Lung clearance index
- MRI:
-
Magnetic resonance imaging
- PFT:
-
Pulmonary function test
- SI:
-
Signal intensity
- SI/Vol_delta:
-
Signal intensity/volume difference between in- and expiration
- SI/Vol_in/ex:
-
In-/expiratory signal intensity
- Vol:
-
Lung volumetry
References
O’Sullivan BP, Freedman SD (2009) Cystic fibrosis. Lancet 373(9678):1891–1904. https://doi.org/10.1016/S0140-6736(09)60327-5
Kerem E, Reisman J, Corey M, Canny GJ, Levison H (1992) Prediction of mortality in patients with cystic fibrosis. N Engl J Med 326(18):1187–1191. https://doi.org/10.1056/nejm199204303261804
Horsley A (2009) Lung clearance index in the assessment of airways disease. Respir Med 103(6):793–799. https://doi.org/10.1016/j.rmed.2009.01.025
VanDevanter DR, Wagener JS, Pasta DJ et al (2010) Pulmonary outcome prediction (POP) tools for cystic fibrosis patients. Pediatr Pulmonol 45(12):1156–1166. https://doi.org/10.1002/ppul.21311
Kraemer R, Blum A, Schibler A, Ammann RA, Gallati S (2005) Ventilation inhomogeneities in relation to standard lung function in patients with cystic fibrosis. Am J Respir Crit Care Med 171(4):371–378. https://doi.org/10.1164/rccm.200407-948OC
Gustafsson PM, Aurora P, Lindblad A (2003) Evaluation of ventilation maldistribution as an early indicator of lung disease in children with cystic fibrosis. Eur Respir J 22(6):972–979
Ellemunter H, Fuchs SI, Unsinn KM et al (2010) Sensitivity of lung clearance index and chest computed tomography in early CF lung disease. Respir Med 104(12):1834–1842. https://doi.org/10.1016/j.rmed.2010.06.010
Schaefer JF, Hector A, Schmidt K et al (2017) A semiquantitative MRI-score can predict loss of lung function in patients with cystic fibrosis: preliminary results. Eur Radiol. https://doi.org/10.1007/s00330-017-4870-4
Owens CM, Aurora P, Stanojevic S et al (2011) Lung clearance index and HRCT are complementary markers of lung abnormalities in young children with CF. Thorax 66(6):481–488. https://doi.org/10.1136/thx.2010.150375
Wielputz MO, Mall MA (2015) Imaging modalities in cystic fibrosis: emerging role of MRI. Curr Opin Pulm Med 21(6):609–616. https://doi.org/10.1097/MCP.0000000000000213
Teufel M, Ketelsen D, Fleischer S et al (2013) Comparison between high-resolution CT and MRI using a very short echo time in patients with cystic fibrosis with extra focus on mosaic attenuation. Respiration 86(4):302–311. https://doi.org/10.1159/000343085
Biederer J, Heussel CP, Puderbach M, Wielpuetz MO (2014) Functional magnetic resonance imaging of the lung. Semin Respir Crit Care Med 35(1):74–82. https://doi.org/10.1055/s-0033-1363453
Bauman G, Puderbach M, Heimann T et al (2013) Validation of Fourier decomposition MRI with dynamic contrast-enhanced MRI using visual and automated scoring of pulmonary perfusion in young cystic fibrosis patients. Eur J Radiol 82(12):2371–2377. https://doi.org/10.1016/j.ejrad.2013.08.018
Morbach AE, Gast KK, Schmiedeskamp J et al (2006) Microstructure of the lung: diffusion measurement of hyperpolarized 3Helium. Z Med Phys 16(2):114–122
Boss A, Schaefer S, Martirosian P, Claussen CD, Schick F, Schaefer JF (2008) Magnetic resonance imaging of lung tissue: influence of body positioning, breathing and oxygen inhalation on signal decay using multi-echo gradient-echo sequences. Invest Radiol 43(6):433–438. https://doi.org/10.1097/RLI.0b013e3181690191
Puderbach M, Eichinger M, Gahr J et al (2007) Proton MRI appearance of cystic fibrosis: comparison to CT. Eur Radiol 17(3):716–724. https://doi.org/10.1007/s00330-006-0373-4
Zapke M, Topf HG, Zenker M et al (2006) Magnetic resonance lung function--a breakthrough for lung imaging and functional assessment? A phantom study and clinical trial. Respir Res 7:106. https://doi.org/10.1186/1465-9921-7-106
Sheikh K, Guo F, Capaldi DP et al (2017) Ultrashort echo time MRI biomarkers of asthma. J Magn Reson Imaging 45(4):1204–1215. https://doi.org/10.1002/jmri.25503
Fuchs SI, Ellemunter H, Eder J et al (2012) Feasibility and variability of measuring the lung clearance index in a multi-center setting. Pediatr Pulmonol 47(7):649–657. https://doi.org/10.1002/ppul.21610
Fuchs SI, Eder J, Ellemunter H, Gappa M (2009) Lung clearance index: normal values, repeatability, and reproducibility in healthy children and adolescents. Pediatr Pulmonol 44(12):1180–1185. https://doi.org/10.1002/ppul.21093
Plathow C, Schoebinger M, Fink C et al (2005) Evaluation of lung volumetry using dynamic three-dimensional magnetic resonance imaging. Invest Radiol 40(3):173–179
Bankier AA, O’Donnell CR, Mai VM et al (2004) Impact of lung volume on MR signal intensity changes of the lung parenchyma. J Magn Reson Imaging 20(6):961–966. https://doi.org/10.1002/jmri.20198
Bauman G, Pusterla O, Santini F, Bieri O (2018) Dynamic and steady-state oxygen-dependent lung relaxometry using inversion recovery ultra-fast steady-state free precession imaging at 1.5 T. Magn Reson Med 79(2):839–845. https://doi.org/10.1002/mrm.26739
Dorlochter L, Nes H, Fluge G, Rosendahl K (2003) High resolution CT in cystic fibrosis--the contribution of expiratory scans. Eur J Radiol 47(3):193–198
Kanhere N, Couch MJ, Kowalik K et al (2017) Correlation of LCI with hyperpolarized 129Xe magnetic resonance imaging in pediatric CF subjects. Am J Respir Crit Care Med. https://doi.org/10.1164/rccm.201611-2228LE
Altes TA, Meyer CH, Mata JF et al (2017) Hyperpolarized helium-3 magnetic resonance lung imaging of non-sedated infants and young children: a proof-of-concept study. Clin Imaging 45:105–110. https://doi.org/10.1016/j.clinimag.2017.04.004
Lamarre A, Reilly BJ, Bryan AC, Levison H (1972) Early detection of pulmonary function abnormalities in cystic fibrosis. Pediatrics 50(2):291–298
Leutz-Schmidt P, Stahl M, Sommerburg O et al (2018) Non-contrast enhanced magnetic resonance imaging detects mosaic signal intensity in early cystic fibrosis lung disease. Eur J Radiol 101:178–183. https://doi.org/10.1016/j.ejrad.2018.02.023
Tepper LA, Ciet P, Caudri D, Quittner AL, Utens EM, Tiddens HA (2016) Validating chest MRI to detect and monitor cystic fibrosis lung disease in a pediatric cohort. Pediatr Pulmonol 51(1):34–41. https://doi.org/10.1002/ppul.23328
Stahl M, Wielputz MO, Graeber SY et al (2017) Comparison of lung clearance index and magnetic resonance imaging for assessment of lung disease in children with cystic fibrosis. Am J Respir Crit Care Med 195(3):349–359. https://doi.org/10.1164/rccm.201604-0893OC
Veldhoen S, Weng AM, Knapp J et al (2017) Self-gated non-contrast-enhanced functional lung MR imaging for quantitative ventilation assessment in patients with cystic fibrosis. Radiology 283(1):242–251. https://doi.org/10.1148/radiol.2016160355
Svedberg M, Gustafsson PM, Robinson PD, Rosberg M, Lindblad A (2017) Variability of lung clearance index in clinically stable cystic fibrosis lung disease in school age children. J Cyst Fibros. https://doi.org/10.1016/j.jcf.2017.08.004
Kligerman SJ, Henry T, Lin CT, Franks TJ, Galvin JR (2015) Mosaic attenuation: etiology, methods of differentiation, and pitfalls. Radiographics 35(5):1360–1380. https://doi.org/10.1148/rg.2015140308
Acknowledgments
We would like to separately acknowledge with gratitude the substantial work of the late Dr. Riethmueller toward this project and his meaningful close collaboration. We would also like to thank Dr. Andrew Dickinson for his help editing this manuscript.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Prof. JF Schäfer.
Conflict of interest
The authors declare that they have no conflict of interest.
Statistics and biometry
One of the authors has significant statistical expertise and no complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all patients in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 5736 kb)
Rights and permissions
About this article
Cite this article
Fleischer, S., Kraus, M.S., Gatidis, S. et al. New severity assessment in cystic fibrosis: signal intensity and lung volume compared to LCI and FEV1: preliminary results. Eur Radiol 30, 1350–1358 (2020). https://doi.org/10.1007/s00330-019-06462-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06462-8