Abstract
Objectives
Chemical shift encoding-based water–fat MRI derived proton density fat fraction (PDFF) of the paraspinal muscles has been emerging as a surrogate marker in subjects with sarcopenia, lower back pain, injuries and neuromuscular disorders. The present study investigates the performance of paraspinal muscle PDFF and cross-sectional area (CSA) in predicting isometric muscle strength.
Methods
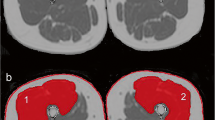
Twenty-six healthy subjects (57.7% women; age: 30 ± 6 years) underwent 3T axial MRI of the lumbar spine using a six-echo 3D spoiled gradient echo sequence for chemical shift encoding-based water–fat separation. Erector spinae and psoas muscles were segmented bilaterally from L2 level to L5 level to determine CSA and PDFF. Muscle flexion and extension maximum isometric torque values [Nm] at the back were measured with an isokinetic dynamometer.
Results
Significant correlations between CSA and muscle strength measurements were observed for erector spinae muscle CSA (r = 0.40; p = 0.044) and psoas muscle CSA (r = 0.61; p = 0.001) with relative flexion strength. Erector spinae muscle PDFF correlated significantly with relative muscle strength (extension: r = -0.51; p = 0.008; flexion: r = -0.54; p = 0.005). Erector spinae muscle PDFF, but not CSA, remained a statistically significant (p < 0.05) predictor of relative extensor strength in multivariate regression models (R2adj = 0.34; p = 0.002).
Conclusions
PDFF measurements improved the prediction of paraspinal muscle strength beyond CSA. Therefore, chemical shift encoding-based water–fat MRI may be used to detect subtle changes in the paraspinal muscle composition.
Key Points
• We investigated the association of paraspinal muscle fat fraction based on chemical shift encoding-based water–fat MRI with isometric strength measurements in healthy subjects.
• Erector spinae muscle PDFF correlated significantly with relative muscle strength.
• PDFF measurements improved prediction of paraspinal muscle strength beyond CSA.




Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- CSA:
-
Cross-sectional area
- ESL:
-
Left erector spinae muscles
- ESR:
-
Right erector spinae muscles
- IPAQ:
-
International Physical Activity Questionnaire
- LBP:
-
Lower back pain
- MFI:
-
Muscle fat infiltration
- MVIC:
-
Maximum voluntary isometric contraction
- NMD:
-
Neuromuscular diseases
- PDFF:
-
Proton density fat fraction
- PL:
-
Left psoas muscle
- PR:
-
Right psoas muscle
- RMSCV:
-
Root mean square coefficients of variation
- ROIs:
-
Regions of interest
References
Hicks GE, Simonsick EM, Harris TB et al (2005) Cross-sectional associations between trunk muscle composition, back pain, and physical function in the health, aging and body composition study. J Gerontol A Biol Sci Med Sci 60:882–887
Fisher MJ, Meyer RA, Adams GR, Foley JM, Potchen EJ (1990) Direct relationship between proton T2 and exercise intensity in skeletal muscle MR images. Invest Radiol 25:480–485
Shellock FG, Fukunaga T, Mink JH, Edgerton VR (1991) Acute effects of exercise on MR imaging of skeletal muscle: concentric vs eccentric actions. AJR Am J Roentgenol 156:765–768
Takahashi H, Kuno S, Miyamoto T et al (1994) Changes in magnetic resonance images in human skeletal muscle after eccentric exercise. Eur J Appl Physiol Occup Physiol 69:408–413
Mendez-Villanueva A, Suarez-Arrones L, Rodas G et al (2016) MRI-Based Regional Muscle Use during Hamstring Strengthening Exercises in Elite Soccer Players. PLoS One 11:e0161356
Crawford RJ, Filli L, Elliott JM et al (2016) Age- and Level-Dependence of Fatty Infiltration in Lumbar Paravertebral Muscles of Healthy Volunteers. AJNR Am J Neuroradiol 37:742–748
Dahlqvist JR, Vissing CR, Hedermann G, Thomsen C, Vissing J (2017) Fat Replacement of Paraspinal Muscles with Aging in Healthy Adults. Med Sci Sports Exerc 49:595–601
Heymsfield SB, Gonzalez MC, Lu J, Jia G, Zheng J (2015) Skeletal muscle mass and quality: evolution of modern measurement concepts in the context of sarcopenia. Proc Nutr Soc 74:355–366
Karampinos DC, Baum T, Nardo L et al (2012) Characterization of the regional distribution of skeletal muscle adipose tissue in type 2 diabetes using chemical shift-based water/fat separation. J Magn Reson Imaging 35:899–907
Kjaer P, Bendix T, Sorensen JS, Korsholm L, Leboeuf-Yde C (2007) Are MRI-defined fat infiltrations in the multifidus muscles associated with low back pain? BMC Med 5:2–2
Teichtahl AJ, Urquhart DM, Wang Y et al (2015) Fat infiltration of paraspinal muscles is associated with low back pain, disability, and structural abnormalities in community-based adults. Spine J 15:1593–1601
D'Hooge R, Cagnie B, Crombez G, Vanderstraeten G, Dolphens M, Danneels L (2012) Increased intramuscular fatty infiltration without differences in lumbar muscle cross-sectional area during remission of unilateral recurrent low back pain. Man Ther 17:584–588
Fischer MA, Nanz D, Shimakawa A et al (2013) Quantification of muscle fat in patients with low back pain: comparison of multi-echo MR imaging with single-voxel MR spectroscopy. Radiology 266:555–563
Elliott JM, Courtney DM, Rademaker A, Pinto D, Sterling MM, Parrish TB (2015) The Rapid and Progressive Degeneration of the Cervical Multifidus in Whiplash: An MRI Study of Fatty Infiltration. Spine (Phila Pa 1976) 40:E694–E700
Maly MR, Calder KM, Macintyre NJ, Beattie KA (2013) Relationship of intermuscular fat volume in the thigh with knee extensor strength and physical performance in women at risk of or with knee osteoarthritis. Arthritis Care Res (Hoboken) 65:44–52
Sun D, Liu P, Cheng J, Ma Z, Liu J, Qin T (2017) Correlation between intervertebral disc degeneration, paraspinal muscle atrophy, and lumbar facet joints degeneration in patients with lumbar disc herniation. BMC Musculoskelet Disord 18:167
Janssen BH, Voet NBM, Nabuurs CI et al (2014) Distinct Disease Phases in Muscles of Facioscapulohumeral Dystrophy Patients Identified by MR Detected Fat Infiltration. PLoS One 9:e85416
Dahlqvist JR, Vissing CR, Thomsen C, Vissing J (2014) Severe paraspinal muscle involvement in facioscapulohumeral muscular dystrophy. Neurology 83:1178–1183
D'Aprile P, Tarantino A, Jinkins JR, Brindicci D (2007) The value of fat saturation sequences and contrast medium administration in MRI of degenerative disease of the posterior/perispinal elements of the lumbosacral spine. Eur Radiol 17:523–531
Kumar Y, Hayashi D (2016) Role of magnetic resonance imaging in acute spinal trauma: a pictorial review. BMC Musculoskelet Disord 17:310
Crawford RJ, Cornwall J, Abbott R, Elliott JM (2017) Manually defining regions of interest when quantifying paravertebral muscles fatty infiltration from axial magnetic resonance imaging: a proposed method for the lumbar spine with anatomical cross-reference. BMC Musculoskelet Disord 18:25
Smith AC, Parrish TB, Abbott R et al (2014) Muscle-fat MRI: 1.5 Tesla and 3.0 Tesla versus histology. Muscle Nerve 50:170–176
Hadar H, Gadoth N, Heifetz M (1983) Fatty replacement of lower paraspinal muscles: normal and neuromuscular disorders. AJR Am J Roentgenol 141:895–898
Doherty TJ (2003) Invited review: Aging and sarcopenia. J Appl Physiol (1985) 95:1717–1727
Fortin M, Macedo LG (2013) Multifidus and paraspinal muscle group cross-sectional areas of patients with low back pain and control patients: a systematic review with a focus on blinding. Phys Ther 93:873–888
Fortin M, Videman T, Gibbons LE, Battie MC (2014) Paraspinal muscle morphology and composition: a 15-yr longitudinal magnetic resonance imaging study. Med Sci Sports Exerc 46:893–901
Valentin S, Licka T, Elliott J (2015) Age and side-related morphometric MRI evaluation of trunk muscles in people without back pain. Man Ther 20:90–95
Fortin M, Yuan Y, Battié MC (2013) Factors Associated With Paraspinal Muscle Asymmetry in Size and Composition in a General Population Sample of Men. Phys Ther 93:1540–1550
Shahidi B, Parra CL, Berry DB et al (2017) Contribution of Lumbar Spine Pathology and Age to Paraspinal Muscle Size and Fatty Infiltration. Spine (Phila Pa 1976) 42:616–623
Goodpaster BH, Carlson CL, Visser M et al (2001) Attenuation of skeletal muscle and strength in the elderly: The Health ABC Study. J Appl Physiol (1985) 90:2157–2165
Goodpaster BH, Park SW, Harris TB et al (2006) The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci 61:1059–1064
Baum T, Inhuber S, Dieckmeyer M et al (2016) Association of quadriceps muscle fat with isometric strength measurements in healthy males using chemical shift encoding-based water-fat magnetic resonance imaging. J Comput Assist Tomogr 40:447–451
Stark T, Walker B, Phillips JK, Fejer R, Beck R (2011) Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: a systematic review. Pm r 3:472–479
Moreau CE, Green BN, Johnson CD, Moreau SR (2001) Isometric back extension endurance tests: a review of the literature. J Manipulative Physiol Ther 24:110–122
Guedes DP, Lopes CC, Guedes JERP (2005) Reprodutibilidade e validade do Questionário Internacional de Atividade Física em adolescentes. Revista Brasileira de Medicina do Esporte 11:151–158
Kurtze N, Rangul V, Hustvedt BE (2008) Reliability and validity of the international physical activity questionnaire in the Nord-Trondelag health study (HUNT) population of men. BMC Med Res Methodol 8:63
Karampinos DC, Yu H, Shimakawa A, Link TM, Majumdar S (2011) T1-corrected fat quantification using chemical shift-based water/fat separation: application to skeletal muscle. Magn Reson Med 66:1312–1326
Gluer CC, Blake G, Lu Y, Blunt BA, Jergas M, Genant HK (1995) Accurate assessment of precision errors: how to measure the reproducibility of bone densitometry techniques. Osteoporos Int 5:262–270
Roth R, Donath L, Kurz E, Zahner L, Faude O (2017) Absolute and relative reliability of isokinetic and isometric trunk strength testing using the IsoMed-2000 dynamometer. Phys Ther Sport 24:26–31
Miller AEJ, MacDougall JD, Tarnopolsky MA, Sale DG (1993) Gender differences in strength and muscle fiber characteristics. Eur J Appl Physiol Occup Physiol 66:254–262
Horvath JJ, Austin SL, Case LE et al (2015) Correlation between quantitative whole-body muscle magnetic resonance imaging and clinical muscle weakness in pompe disease. Muscle Nerve 51:722–730
Willis TA, Hollingsworth KG, Coombs A et al (2013) Quantitative Muscle MRI as an Assessment Tool for Monitoring Disease Progression in LGMD2I: A Multicentre Longitudinal Study. PLoS One 8:e70993
Willis TA, Hollingsworth KG, Coombs A et al (2014) Quantitative Magnetic Resonance Imaging in Limb-Girdle Muscular Dystrophy 2I: A Multinational Cross-Sectional Study. PLoS One 9:e90377
Kumar D, Karampinos DC, MacLeod TD et al (2014) Quadriceps intramuscular fat fraction rather than muscle size is associated with knee osteoarthritis. Osteoarthritis Cartilage 22:226–234
Colloca CJ, Hinrichs RN (2005) The biomechanical and clinical significance of the lumbar erector spinae flexion-relaxation phenomenon: a review of literature. J Manipulative Physiol Ther 28:623–631
Funding
This study has received funding by Philips Healthcare, the German Research Foundation (DFG-SFB824/A9) and TUM Faculty of Medicine KKF grant H01.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Thomas Baum, MD.
Conflict of interest
The authors of this manuscript declare relationships with the following companies: Philips Healthcare.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Prospective
• Cross-sectional study
• Performed at one institution
Rights and permissions
About this article
Cite this article
Schlaeger, S., Inhuber, S., Rohrmeier, A. et al. Association of paraspinal muscle water–fat MRI-based measurements with isometric strength measurements. Eur Radiol 29, 599–608 (2019). https://doi.org/10.1007/s00330-018-5631-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5631-8