Abstract
Background
Magnetic resonance imaging (MRI) is the diagnostic cornerstone for precisely identifying acute ischaemic strokes and locating vascular occlusions, especially since mechanical thrombectomy has become a reference treatment. We observed that a post-contrast three-dimensional turbo-spin-echo T1-weighted sequence showed striking post-contrast vascular hyperintensities (PCVH) in ischaemic territories. We aimed to evaluate the prevalence and the meaning of this finding.
Methods
This retrospective single centre study included 130 consecutive patients admitted for acute ischaemic stroke with a 3-T MRI performed in the first 12 h of symptom onset from September 2014 through September 2016. Two neuroradiologists blinded to clinical data analysed the first MRI assessments. The association between PCVH and clinical, radiological and follow-up findings was assessed, as well as inter- and intra-observer agreements.
Results
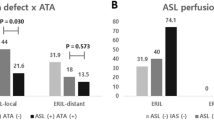
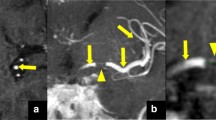
Of 130 patients, 105 (81%) had PCVH in the ischaemic territory. PCVH were associated with the presence of thrombus on susceptibility weighted imaging (p < 0.0001) and vascular occlusions on MR angiography (p < 0.0001). All patients with a visible thrombus had PCVH closely surrounding the clot. PCVH were associated with higher initial (p < 0.01) and follow-up (p < 0.01) National Institutes of Health Stroke Scale score, and higher mRS score (p < 0.05). Thrombectomy was the reference treatment for all patients with arterial occlusions. Inter- and intra-observer agreements for the detection of PCVH were excellent (κ = 0.95 and κ = 0.91, respectively).
Conclusions
PCVH during acute strokes are a striking sensitive and reproducible tool for diagnosing and locating vascular occlusions. It may help triage patients who can benefit from thrombectomy.
Key points
• Post-contrast vascular hyperintensities (PCVH) are a sensitive MR finding in acute stroke
• PCVH are strongly associated with the presence and location of arterial occlusions
• Inter- and intra-observer agreements for the detection of PCVH are excellent
• PCVH are visible even in the case of significant motion artefacts
• PCVH may help triage patients who can benefit from mechanical thrombectomy




Similar content being viewed by others
Abbreviations
- FVH:
-
FLAIR Vascular Hyperintensities
- MSDE:
-
Motion Sensitised Driven Equilibrium
- MT:
-
Mechanical Thrombectomy
- NIHSS:
-
National Institutes of Health Stroke Scale
- PCVH:
-
Post-contrast Vascular Hyperintensities
References
Mukherjee D, Patil CG (2011) Epidemiology and the global burden of stroke. World Neurosurg 76:S85–S90
Nogueira RG, Jadhav AP, Haussen DC et al (2018) Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 378:11–21
Jovin TG, Chamorro A, Cobo E et al (2015) Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 372:2296–2306
Haute Autorité de Santé (2016) Thrombectomie des artères intracrâniennes par voie endovasculaire, France. https://www.has-sante.fr/portail/upload/docs/application/pdf/2016-11/rapport_thrombectomie.pdf. Accessed 12 Nov 2017
Powers WJ, Derdeyn CP, Biller J et al (2015) 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment. Stroke 46:3020–3035
European Stroke Organisation (ESO) Executive Committee, ESO Writing Committee (2008) Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis 25:457–507
Schellinger PD, Bryan RN, Caplan LR et al (2010) Evidence-based guideline: The role of diffusion and perfusion MRI for the diagnosis of acute ischemic stroke: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology 75:177–185
Chalela JA, Kidwell CS, Nentwich LM et al (2007) Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison. Lancet 369:293–298
Haute Autorité de Santé (2009) Accident vasculaire cérébral (AVC): prise en charge précoce, France. https://www.has-sante.fr/portail/upload/docs/application/pdf/2009-07/avc_prise_en_charge_precoce_-_recommandations.pdf. Accessed 12 Nov 2017
Schaefer PW, Pulli B, Copen WA et al (2015) Combining MRI with NIHSS thresholds to predict outcome in acute ischemic stroke: value for patient selection. AJNR Am J Neuroradiol 36:259–264
Hodel J, Leclerc X, Rodallec M et al (2013) Fluid-attenuated inversion recovery vascular hyperintensities are not visible using 3D CUBE FLAIR sequence. Eur Radiol 23:1963–1969
Smith WS, Tsao JW, Billings ME et al (2006) Prognostic significance of angiographically confirmed large vessel intracranial occlusion in patients presenting with acute brain ischemia. Neurocrit Care 4:14–17
von Elm E, Altman DG, Egger M et al (2008) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61:344–349
R Core Team (2015) R: a language and environment for statistical computing. http://www.r-project.org/. Accessed 4 Nov 2017
Yoo AJ, Verduzco LA, Schaefer PW et al (2009) MRI-based selection for intra-arterial stroke therapy: value of pretreatment diffusion-weighted imaging lesion volume in selecting patients with acute stroke who will benefit from early recanalization. Stroke 40:2046–2054
Friedrich B, Gawlitza M, Schob S et al (2015) Distance to thrombus in acute middle cerebral artery occlusion. Stroke 46:692–696
Campbell BCV (2016) Clot length assessment in stroke therapy decisions. Stroke 47:643–644
Oppenheim C, Naggara O, Arquizan C et al (2005) MRI of acute ischemic stroke. J Radiol 86:1069–1078
Yoneyama M, Nakamura M, Takahara T et al (2014) Improvement of T1 contrast in whole-brain black-blood imaging using motion-sensitized driven-equilibrium prepared 3D turbo spin echo (3D MSDE-TSE). Magn Reson Med Sci 13:61–65
Acknowledgments
Laura McMaster provided professional English-language medical editing of this article. Malek Ben Maacha provided valuable data about mechanical thrombectomy devices.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Julien Savatovsky.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Marie Astrid Metten kindly provided statistical advice for this manuscript.
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• observational
• performed at one institution
Rights and permissions
About this article
Cite this article
Duron, L., Savatovsky, J., Obadia, M. et al. Magnetic resonance post-contrast vascular hyperintensities at 3 T: a new highly sensitive sign of vascular occlusion in acute ischaemic stroke. Eur Radiol 28, 2903–2913 (2018). https://doi.org/10.1007/s00330-018-5312-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5312-7