Abstract
Objectives
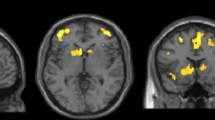
To apply three-dimensional multifrequency MR-elastography (3DMRE) for the measurement of local cerebral viscoelasticity changes in patients with Parkinson's disease (PD) and progressive supranuclear palsy (PSP).
Methods
T1-weighted anatomical imaging and 3DMRE were performed in 17 PD and 20 PSP patients as well as 12 controls. Two independent viscoelasticity parameters, |G*| and φ, were reconstructed combining seven harmonic vibration frequencies (30–60 Hz). Spatially averaged values were compared by one-way ANOVA, groups were compared using unpaired t test and Mann-Whitney test, respectively. Correlation between clinical data and parameters of brain elasticity and volume were calculated by Pearson’s correlation coefficient.
Results
In patients, |G*| was significantly reduced in the frontal and mesencephalic regions (p < 0.05). Beyond that, reduced mesencephalic |G*| discriminated PSP from PD (p < 0.05). Neurodegeneration causes significant brain atrophy (p < 0.01) and is pronounced in PSP patients (p < 0.05 vs. PD). Reduced brain viscoelasticity is correlated with brain atrophy in PSP (r=0.64, p=0.002) and PD (r=0.65, p=0.005) patients but not in controls.
Conclusions
MRE-measured viscoelasticity reflects local structural changes of brain tissue in PSP and in PD and provides a useful parameter to differentiate neurodegenerative movement disorders based on imaging examinations.
Key points
• 3D multifrequency MR-elastography reveals diffuse regional changes in brain viscoelasticity in neurodegenerative disorders.
• Reduced mesencephalic viscoelasticity separates PD and PSP.
• Reduced brain viscoelasticity and brain atrophy as independent hallmarks of neurodegeneration hypothesized.


Similar content being viewed by others
Abbreviations
- |G*|:
-
Magnitude of the complex shear modulus
- 3DMRE:
-
Three-dimensional magnetic resonance elastography
- FoV:
-
Field of view
- GM, WM:
-
Cortical grey matter, white matter
- MEG:
-
Motion-encoding gradients
- MRE:
-
Magnetic resonance elastography
- PD:
-
Parkinson’s disease
- PSP:
-
Progressive supranuclear palsy
- PSPRS:
-
PSP rating scale
- ROI:
-
Regions-of-interest
- UPDRS part III :
-
Motor part of the MDS-Unified Parkinson’s Disease Rating Scale
- φ:
-
Phase angle of the complex shear modulus
References
Dickson DW, Fujishiro H, Orr C et al (2009) Neuropathology of non-motor features of Parkinson disease. Parkinsonism Relat Disord 15:S1–S5
Hoglinger GU, Respondek G, Stamelou M et al (2017) Clinical diagnosis of progressive supranuclear palsy: The movement disorder society criteria. Mov Disord. https://doi.org/10.1002/mds.26987
Respondek G, Stamelou M, Kurz C et al (2014) The phenotypic spectrum of progressive supranuclear palsy: a retrospective multicenter study of 100 definite cases. Mov Disord 29:1758–1766
Schrag A, Good CD, Miszkiel K et al (2000) Differentiation of atypical parkinsonian syndromes with routine MRI. Neurology 54:697–702
Mahlknecht P, Hotter A, Hussl A, Esterhammer R, Schocke M, Seppi K (2010) Significance of MRI in diagnosis and differential diagnosis of Parkinson's disease. Neurodegener Dis 7:300–318
Hiscox LV, Johnson CL, Barnhill E et al (2016) Magnetic resonance elastography (MRE) of the human brain: technique, findings and clinical applications. Phys Med Biol 61:R401–R437
Wuerfel J, Paul F, Beierbach B et al (2010) MR-elastography reveals degradation of tissue integrity in multiple sclerosis. Neuroimage 49:2520–2525
Streitberger KJ, Sack I, Krefting D et al (2012) Brain viscoelasticity alteration in chronic-progressive multiple sclerosis. PLoS ONE 7:e29888
Streitberger KJ, Fehlner A, Pache F et al (2017) Multifrequency magnetic resonance elastography of the brain reveals tissue degeneration in neuromyelitis optica spectrum disorder. Eur Radiol 27:2206–2215
Murphy MC, Jones DT, Jack CR Jr et al (2016) Regional brain stiffness changes across the Alzheimer's disease spectrum. Neuroimage Clin 10:283–290
ElSheikh M, Arani A, Perry A et al (2017) MR Elastography Demonstrates Unique Regional Brain Stiffness Patterns in Dementias. AJR Am J Roentgenol 209:403–408
Hain EG, Klein C, Munder T et al (2016) Dopaminergic Neurodegeneration in the Mouse Is Associated with Decrease of Viscoelasticity of Substantia Nigra Tissue. PLoS One 11:e0161179
Lipp A, Trbojevic R, Paul F et al (2013) Cerebral magnetic resonance elastography in supranuclear palsy and idiopathic Parkinson's disease. Neuroimage Clin 3:381–387
Schregel K, Wuerfel E, Garteiser P et al (2012) Demyelination reduces brain parenchymal stiffness quantified in vivo by magnetic resonance elastography. Proc Natl Acad Sci U S A 109:6650–6655
Hughes AJ, Ben-Shlomo Y, Daniel SE, Lees AJ (1992) What features improve the accuracy of clinical diagnosis in Parkinson's disease: a clinicopathologic study. Neurology 42:1142–1146
Litvan I, Bhatia KP, Burn DJ et al (2003) Movement Disorders Society Scientific Issues Committee report: SIC Task Force appraisal of clinical diagnostic criteria for Parkinsonian disorders. Mov Disord 18:467–486
Goetz CG, Tilley BC, Shaftman SR et al (2008) Movement Disorder Society-sponsored revision of the Unified Parkinson's Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord 23:2129–2170
Golbe LI, Ohman-Strickland PA (2007) A clinical rating scale for progressive supranuclear palsy. Brain 130:1552–1565
Streitberger KJ, Reiss-Zimmermann M, Freimann FB et al (2014) High-resolution mechanical imaging of glioblastoma by multifrequency magnetic resonance elastography. PLoS One 9:e110588
Hirsch S, Klatt D, Freimann F, Scheel M, Braun J, Sack I (2013) In vivo measurement of volumetric strain in the human brain induced by arterial pulsation and harmonic waves. Magn Reson Med 70:671–683
Hirsch S, Guo J, Reiter R et al (2014) MR elastography of the liver and the spleen using a piezoelectric driver, single-shot wave-field acquisition, and multifrequency dual parameter reconstruction. Magn Reson Med 71:267–277
Rump J, Klatt D, Braun J, Warmuth C, Sack I (2007) Fractional encoding of harmonic motions in MR elastography. Magn Reson Med 57:388–395
Papazoglou S, Xu C, Hamhaber U et al (2009) Scatter-based magnetic resonance elastography. Phys Med Biol 54:2229–2241
Fehlner A, Behrens JR, Streitberger KJ et al (2016) Higher-resolution MR elastography reveals early mechanical signatures of neuroinflammation in patients with clinically isolated syndrome. J Magn Reson Imaging 44:51–58
Hirsch S, Braun J, Sack I (2017) Magnetic Resonance Elastography: Physical Background and Medical Applications. Wiley-VCH
Avants BB, Tustison NJ, Song G, Cook PA, Klein A, Gee JC (2011) A reproducible evaluation of ANTs similarity metric performance in brain image registration. Neuroimage 54:2033–2044
Resnick SM, Pham DL, Kraut MA, Zonderman AB, Davatzikos C (2003) Longitudinal magnetic resonance imaging studies of older adults: a shrinking brain. J Neurosci 23:3295–3301
Sack I, Beierbach B, Wuerfel J et al (2009) The impact of aging and gender on brain viscoelasticity. Neuroimage 46:652–657
Sack I, Streitberger KJ, Krefting D, Paul F, Braun J (2011) The influence of physiological aging and atrophy on brain viscoelastic properties in humans. PLoS ONE 6:e23451
Arani A, Murphy MC, Glaser KJ et al (2015) Measuring the effects of aging and sex on regional brain stiffness with MR elastography in healthy older adults. Neuroimage 111:59–64
Massey LA, Micallef C, Paviour DC et al (2012) Conventional magnetic resonance imaging in confirmed progressive supranuclear palsy and multiple system atrophy. Mov Disord 27:1754–1762
Fehlner A, Hirsch S, Weygandt M et al (2017) Increasing the spatial resolution and sensitivity of magnetic resonance elastography by correcting for subject motion and susceptibility-induced image distortions. J Magn Reson Imaging 46:134–141
Dittmann F, Hirsch S, Tzschatzsch H, Guo J, Braun J, Sack I (2016) In vivo wideband multifrequency MR elastography of the human brain and liver. Magn Reson Med 76:1116–1126
Funding
This study has received funding by the German Research Foundation (DFG Sa901/17) to Ingolf Sack. Parts of the study were supported by the European Union’s Horizon 2020 Programme (ID 668039, EU FORCE – Imaging the Force of Cancer) and German Federal Ministry of Education and Research (BMBF 01GQ1408)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Ingolf Sack.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Ethical approval
Institutional Review Board approval was obtained.
Informed consent
Written informed consent was obtained from all subjects in this study.
Methodology
• prospective
• observational
• performed at one institution.
Electronic supplementary material
ESM 1
(DOCX 28 kb)
Rights and permissions
About this article
Cite this article
Lipp, A., Skowronek, C., Fehlner, A. et al. Progressive supranuclear palsy and idiopathic Parkinson’s disease are associated with local reduction of in vivo brain viscoelasticity. Eur Radiol 28, 3347–3354 (2018). https://doi.org/10.1007/s00330-017-5269-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-5269-y