Abstract
Objective
To determine the clinical efficacy of sonographically-guided percutaneous bone drilling of the lateral epicondyle (LE) for the treatment of patients with LE.
Methods
We included 24 patients with LE who reported pain in this study. All patients underwent sonographically-guided percutaneous bone drilling of the lateral epicondyle. Follow-up sonography and physical examinations were performed 1, 3 and 6 months after the procedure. The outcome measures included sonographic findings, visual analogue scale (VAS) score, maximum voluntary grip strength (MVGS) and patient-related tennis elbow evaluation (PRTEE) score.
Results
None of the patients had immediate complications during the procedure. The area of the extensor carpi radialis brevis (ECRB) tears decreased significantly at 1 month and declined gradually over the remaining 5 months of the study (p < 0.001). The mean pain VAS score was significantly lower at 6 months than preoperatively (respectively; p < 0.001). The mean MVGS increased significantly between pretreatment and 6 months post-treatment (p < 0.001), whereas the PRTEE score decreased significantly during the same period (p < 0.001).
Conclusion
Sonographically-guided percutaneous drilling is a quick and safe treatment option for LE that can be performed in an outpatient setting.
Key Points
• Percutaneous drilling of the lateral condyle is effective for the treatment of LE.
• The area of ECRB tears can be measured by US-guided saline injection.
• US-guided percutaneous drilling is a quick and safe treatment option for LE.






Similar content being viewed by others
References
Sayegh ET, Strauch RJ (2015) Does nonsurgical treatment improve longitudinal outcomes of lateral epicondylitis over no treatment? A meta-analysis. Clin Orthop Relat Res 473:1093–1107
Smidt N, van der Windt DA (2006) Tennis elbow in primary care. BMJ 333:927–928
Lee MH, Cha JG, Jin W et al (2011) Utility of sonographic measurement of the common tensor tendon in patients with lateral epicondylitis. AJR Am J Roentgenol 196:1363–1367
Ahmad Z, Siddiqui N, Malik SS, Abdus-Samee M, Tytherleigh-Strong G, Rushton N (2013) Lateral epicondylitis: a review of pathology and management. Bone Joint J 95-b:1158–1164
du Toit C, Stieler M, Saunders R, Bisset L, Vicenzino B (2008) Diagnostic accuracy of power Doppler ultrasound in patients with chronic tennis elbow. Br J Sports Med 42:572–576
Clarke AW, Ahmad M, Curtis M, Connell DA (2010) Lateral elbow tendinopathy: correlation of ultrasound findings with pain and functional disability. Am J Sports Med 38:1209–1214
Orchard J, Kountouris A (2011) The management of tennis elbow. BMJ 342:d2687
Walz DM, Newman JS, Konin GP, Ross G (2010) Epicondylitis: pathogenesis, imaging, and treatment. Radiographics 30:167–184
Hechtman KS, Uribe JW, Botto-vanDemden A, Kiebzak GM (2011) Platelet-rich plasma injection reduces pain in patients with recalcitrant epicondylitis. Orthopedics 34:92
Mishra A, Pavelko T (2006) Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med 34:1774–1778
Connell DA, Ali KE, Ahmad M, Lambert S, Corbett S, Curtis M (2006) Ultrasound-guided autologous blood injection for tennis elbow. Skelet Radiol 35:371–377
Edwards SG, Calandruccio JH (2003) Autologous blood injections for refractory lateral epicondylitis. J Hand Surg [Am] 28:272–278
Keizer SB, Rutten HP, Pilot P, Morre HH, v Os JJ, Verburg AD (2002) Botulinum toxin injection versus surgical treatment for tennis elbow: a randomized pilot study. Clin Orthop Relat Res: 125–131
Lin CL, Lee JS, Su WR, Kuo LC, Tai TW, Jou IM (2011) Clinical and ultrasonographic results of ultrasonographically-guided percutaneous radiofrequency lesioning in the treatment of recalcitrant lateral epicondylitis. Am J Sports Med 39:2429–2435
Coleman B, Quinlan JF, Matheson JA (2010) Surgical treatment for lateral epicondylitis: a long-term follow-up of results. J Shoulder Elb Surg 19:363–367
Garden RS (1961) Tennis elbow. J Bone Joint Surg Br Vol 43-B:100–106
Barnes DE, Beckley JM, Smith J (2015) Percutaneous ultrasonic tenotomy for chronic elbow tendinosis: a prospective study. J Shoulder Elb Surg 24:67–73
Chiavaras MM, Jacobson JA (2013) Ultrasound-guided tendon fenestration. Semin Musculoskelet Radiol 17:85–90
Housner JA, Jacobson JA, Misko R (2009) Sonographically-guided percutaneous needle tenotomy for the treatment of chronic tendinosis. J Ultrasound Med 28:1187–1192
Rompe JD, Overend TJ, MacDermid JC (2007) Validation of the patient-rated tennis elbow evaluation questionnaire. J Hand Ther 20:3–10, quiz 11
Dunn JH, Kim JJ, Davis L, Nirschl RP (2008) Ten- to 14-year follow-up of the Nirschl surgical technique for lateral epicondylitis. Am J Sports Med 36:261–266
Hayashi K, Kumai T, Higashiyama I, Shinohara Y, Matsuda T, Takakura Y (2009) Repair process after fibrocartilaginous enthesis drilling: histological study in a rabbit model. J Orthop Sci 14:76–84
Schipper ON, Dunn JH, Ochiai DH, Donovan JS, Nirschl RP (2011) Nirschl surgical technique for concomitant lateral and medial elbow tendinosis: a retrospective review of 53 elbows with a mean follow-up of 11.7 years. Am J Sports Med 39:972–976
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Jang Gyu Cha.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Funding
This study has received funding by Soonchunghayng University Research Fund.
Statistics and biometry
Bo Ra Lee kindly provided statistical advice for this manuscript.
Ethical approval
Institutional Review Board approval was obtained.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Methodology
• prospective
• case-series study
Electronic supplementary material
Below is the link to the electronic supplementary material.
Video 1
US-guided saline injection into the ECRB tear site. When the injected fluid had fully collected in the hypoechoic clefts, the tendon tear in the ECRB was clearly demarcated on sonography as a hyperechoic ovoid lesion. (MP4 455 kb)
Video 2
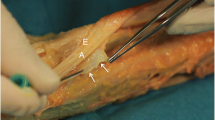
US-guided drilling procedure. The wire was then advanced through the diseased tendon site until the bony cortex was punctured just below the tear site. (MP4 509 kb)
Video 3-4
Preoperative (Video 3) and follow-up sonographic images (video 4) A 34-year-old man clinically diagnosed with lateral epicondylitis. After the injection of saline into the ECRB tendon tear, preoperative evaluation using grey-scale ultrasonography (US) showed an inflated tear as a low-echoic cyst in the extensor origin (arrows) (Video 3). The area of the tear was 0.14 cm2. Ultrasound of the extensor origin 6 months postoperatively revealed a decrease in the area of the tear (Video 4). (MP4 297 kb)
Rights and permissions
About this article
Cite this article
Yoo, S.H., Cha, J.G. & Lee, B.R. Ultrasound-guided percutaneous bone drilling for the treatment of lateral epicondylitis. Eur Radiol 28, 390–397 (2018). https://doi.org/10.1007/s00330-017-4932-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-4932-7