Abstract
Objectives
To determine the utility of amide proton transfer-weighted (APTw) MR imaging in distinguishing solitary brain metastases (SBMs) from glioblastomas (GBMs).
Methods
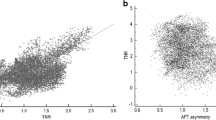
Forty-five patients with SBMs and 43 patients with GBMs underwent conventional and APT-weighted sequences before clinical intervention. The APTw parameters and relative APTw (rAPTw) parameters in the tumour core and the peritumoral brain zone (PBZ) were obtained and compared between SBMs and GBMs. The receiver-operating characteristic (ROC) curve was used to assess the best parameter for distinguishing between the two groups.
Results
The APTwmax, APTwmin, APTwmean, rAPTwmax, rAPTwmin or rAPTwmean values in the tumour core were not significantly different between the SBM and GBM groups (P = 0.141, 0.361, 0.221, 0.305, 0.578 and 0.448, respectively). However, the APTwmax, APTwmin, APTwmean, rAPTwmax, rAPTwmin or rAPTwmean values in the PBZ were significantly lower in the SBM group than in the GBM group (P < 0.001). The APTwmin values had the highest area under the ROC curve 0.905 and accuracy 85.2% in discriminating between the two neoplasms.
Conclusion
As a noninvasive imaging method, APT-weighted MR imaging can be used to distinguish SBMs from GBMs.
Key Points
• APTw values in the tumour core were not different between SBMs and GBMs.
• APTw values in peritumoral brain zone were lower in SBMs than in GBMs.
• The APTw min was the best parameter to distinguish SBMs from GBMs.




Similar content being viewed by others
Abbreviations
- GBM:
-
Glioblastoma
- SBM:
-
Solitary brain metastases
- APT:
-
Amide proton transfer
- APTw:
-
APT-weighted
- rAPTw:
-
Relative APTw
- CEST:
-
Chemical exchange-based saturation transfer
- CNAWM:
-
Contralateral normal-appearing white matter
- Gd:
-
Gadolinium
- H&E:
-
Haematoxylin and eosin
- PBZ:
-
Peritumoral brain zone
References
Wang X, Chen JX, Zhou Q et al (2016) Statistical report of central nervous system tumors histologically diagnosed in the Sichuan Province of China from 2008 to 2013: a West China Glioma Center Report. Ann Surg Oncol. doi:10.1245/s10434-016-5410-1
Ostrom QT, Gittleman H, Fulop J et al (2015) CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2008-2012. Neuro-Oncology 17:v1–iv62
Blanchet L, Krooshof PW, Postma GJ et al (2011) Discrimination between metastasis and glioblastoma multiforme based on morphometric analysis of MR images. AJNR Am J Neuroradiol 32:67–73
Yuh WT, Engelken JD, Muhonen MG, Mayr NA, Fisher DJ, Ehrhardt JC (1992) Experience with high-dose gadolinium MR imaging in the evaluation of brain metastases. AJNR Am J Neuroradiol 13:335–345
Owonikoko TK, Arbiser J, Zelnak A et al (2014) Current approaches to the treatment of metastatic brain tumours. Nat Rev Clin Oncol 11:203–222
Wen PY, Kesari S (2008) Malignant gliomas in adults. N Engl J Med 359:492–507
Lee EJ, Ahn KJ, Lee EK, Lee YS, Kim DB (2013) Potential role of advanced MRI techniques for the peritumoural region in differentiating glioblastoma multiforme and solitary metastatic lesions. Clin Radiol 68:e689–e697
Han CK, Huang SM, Guo JF, Zhuang XJ, Han HW (2015) Use of a high b-value for diffusion weighted imaging of peritumoral regions to differentiate high-grade gliomas and solitary metastases. J Magn Reson Imaging 42:80–86
Abe T, Mizobuchi Y, Sako W et al (2015) Clinical significance of discrepancy between arterial spin labeling images and contrast-enhanced images in the diagnosis of brain tumors. Magn Reson Med Sci 14:313–319
Caivano R, Lotumolo A, Rabasco P et al (2013) 3 Tesla magnetic resonance spectroscopy: cerebral gliomas vs. metastatic brain tumors. Our experience and review of the literature. Int J Neurosci 123:537–543
Mouthuy N, Cosnard G, Abarca-Quinones J, Michoux N (2012) Multiparametric magnetic resonance imaging to differentiate high-grade gliomas and brain metastases. J Neuroradiology Journal de neuroradiologie 39:301–307
Zhou J, Lal B, Wilson DA, Laterra J, van Zijl PC (2003) Amide proton transfer (APT) contrast for imaging of brain tumors. Magn Reson Med 50:1120–1126
Zhou J, Payen JF, Wilson DA, Traystman RJ, van Zijl PC (2003) Using the amide proton signals of intracellular proteins and peptides to detect pH effects in MRI. Nat Med 9:1085–1090
van Zijl PCM, Yadav NN (2011) Chemical exchange saturation transfer (CEST): what is in a name and what Isn't? Magn Reson Med 65:927–948
Jiang SS, Yu H, Wang XL et al (2016) Molecular MRI differentiation between primary central nervous system lymphomas and high-grade gliomas using endogenous protein-based amide proton transfer MR imaging at 3 Tesla. Eur Radiol 26:64–71
Zhou J, Zhu H, Lim M et al (2013) Three-dimensional amide proton transfer MR imaging of gliomas: initial experience and comparison with gadolinium enhancement. J Magn Reson Imaging 38:1119–1128
Togao O, Kessinger CW, Huang G et al (2013) Characterization of lung cancer by amide proton transfer (APT) imaging: an in-vivo study in an orthotopic mouse model. Plos One 8:e77019
Wen ZB, Hu SG, Huang FH et al (2010) MR imaging of high-grade brain tumors using endogenous protein and peptide-based contrast. Neuroimage 51:616–622
Togao O, Hiwatashi A, Yamashita K et al (2016) Grading diffuse gliomas without intense contrast enhancement by amide proton transfer MR imaging: comparisons with diffusion- and perfusion-weighted imaging. Eur Radiol. doi:10.1007/s00330-016-4328-0:1-11
Sakata A, Okada T, Yamamoto A et al (2015) Grading glial tumors with amide proton transfer MR imaging: different analytical approaches. J Neuro-Oncol 122:339–348
Jia G, Abaza R, Williams JD et al (2011) Amide proton transfer MR imaging of prostate cancer: a preliminary study. J Magn Reson Imaging 33:647–654
Klomp DWJ, Dula AN, Arlinghaus LR et al (2013) Amide proton transfer imaging of the human breast at 7T: development and reproducibility. NMR Biomed 26:1271–1277
Dula AN, Arlinghaus LR, Dortch RD et al (2013) Amide proton transfer imaging of the breast at 3 T: Establishing reproducibility and possible feasibility assessing chemotherapy response. Magn Reson Med 70:216–224
Wang J, Weygand J, Hwang KP et al (2016) Magnetic resonance imaging of glucose uptake and metabolism in patients with head and neck cancer. Scientific reports 6:30618
Yuan J, Chen S, King AD et al (2014) Amide proton transfer-weighted imaging of the head and neck at 3 T: a feasibility study on healthy human subjects and patients with head and neck cancer. NMR Biomed 27:1239–1247
Zhou JY, Tryggestad E, Wen ZB et al (2011) Differentiation between glioma and radiation necrosis using molecular magnetic resonance imaging of endogenous proteins and peptides. Nat Med 17:130–U308
Ma B, Blakeley JO, Hong X et al (2016) Applying amide proton transfer-weighted MRI to distinguish pseudoprogression from true progression in malignant gliomas. J Magn Reson Imaging 44:456–462
Tietze A, Blicher J, Mikkelsen IK et al (2014) Assessment of ischemic penumbra in patients with hyperacute stroke using amide proton transfer (APT) chemical exchange saturation transfer (CEST) MRI. NMR Biomed 27:163–174
Tee YK, Harston GWJ, Blockley N et al (2014) Comparing different analysis methods for quantifying the MRI amide proton transfer (APT) effect in hyperacute stroke patients. NMR Biomed 27:1019–1029
Zhao XN, Wen ZB, Huang FH et al (2011) Saturation power dependence of amide proton transfer image contrasts in human brain tumors and strokes at 3 T. Magn Reson Med 66:1033–1041
Li CM, Peng S, Wang R et al (2014) Chemical exchange saturation transfer MR imaging of Parkinson's disease at 3 Tesla. Eur Radiol 24:2631–2639
Zhang Y, Heo HY, Lee DH et al (2016) Selecting the reference image for registration of CEST series. J Magn Reson Imaging 43:756–761
Zhang H, Kang H, Zhao X et al (2016) Amide proton transfer (APT) MR imaging and magnetization transfer (MT) MR imaging of pediatric brain development. Eur Radiol 26:3368–3376
Allen JS, Bruss J, Brown CK, Damasio H (2005) Normal neuroanatomical variation due to age: the major lobes and a parcellation of the temporal region. Neurobiol Aging 26:1245–1260
Tan Y, Wang XC, Zhang H et al (2015) Differentiation of high-grade-astrocytomas from solitary-brain-metastases: comparing diffusion kurtosis imaging and diffusion tensor imaging. Eur J Radiol 84:2618–2624
Crisi G, Orsingher L, Filice S (2013) Lipid and macromolecules quantitation in differentiating glioblastoma from solitary metastasis: a short-echo time single-voxel magnetic resonance spectroscopy study at 3 T. J Comput Assist Tomogr 37:265–271
Lee EJ, terBrugge K, Mikulis D et al (2011) Diagnostic value of peritumoral minimum apparent diffusion coefficient for differentiation of glioblastoma multiforme from solitary metastatic lesions. AJR Am J Roentgenol 196:71–76
Ramalho J, Castillo M, AlObaidy M et al (2015) High signal intensity in globus pallidus and dentate nucleus on unenhanced T1-weighted MR images: evaluation of two linear gadolinium-based contrast agents. Radiology 276:836–844
Collidge TA, Thomson PC, Mark PB et al (2007) Gadolinium-enhanced MR imaging and nephrogenic systemic fibrosis: retrospective study of a renal replacement therapy cohort. Radiology 245:168–175
Lemee JM, Clavreul A, Aubry M et al (2015) Characterizing the peritumoral brain zone in glioblastoma: a multidisciplinary analysis. J Neuro-Oncol 122:53–61
Oh J, Cha S, Aiken AH et al (2005) Quantitative apparent diffusion coefficients and T2 relaxation times in characterizing contrast enhancing brain tumors and regions of peritumoral edema. J Magn Reson Imaging 21:701–708
Goplen D, Bougnaud S, Rajcevic U et al (2010) Alpha B-Crystallin is elevated in highly infiltrative apoptosis-resistant glioblastoma cells. Am J Pathol 177:1618–1628
Parney IF, Waldron JS, Parsa AT (2009) Flow cytometry and in vitro analysis of human glioma-associated macrophages. Laboratory investigation Journal of neurosurgery 110:572–582
Frieboes HB, Zheng X, Sun CH, Tromberg B, Gatenby R, Cristini V (2006) An integrated computational/experimental model of tumor invasion. Cancer Res 66:1597–1604
Fazi B, Felsani A, Grassi L et al (2015) The transcriptome and miRNome profiling of glioblastoma tissues and peritumoral regions highlights molecular pathways shared by tumors and surrounding areas and reveals differences between short-term and long-term survivors. Oncotarget 6:22526–22552
Acknowledgements
This study was partially supported by grants from National Natural Science Foundation of China (81171322), Guangdong Provincial Natural Science Foundation (2014A030313271, S2012010009114), Guangdong Provincial Science and Technology Project (2014A020212726), Southern Medical University clinical research project (LC2016ZD028) and the National Institutes of Health (R01EB009731, R01CA166171).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Zhibo Wen, MD.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Funding
This study is partially supported by grants from National Natural Science Foundation of China (81171322), Natural Science Foundation of Guangdong Province (2014A030313271), Guangdong Provincial Science and Technology Project (2014A020212726), Natural Science Foundation of Guangdong Province (S2012010009114), Southern Medical University clinical research project (LC2016ZD028) and the National Institutes of Health (R01EB009731, R01CA166171).
Statistics and biometry
No complex statistical methods were necessary for this article.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Rights and permissions
About this article
Cite this article
Yu, H., Lou, H., Zou, T. et al. Applying protein-based amide proton transfer MR imaging to distinguish solitary brain metastases from glioblastoma. Eur Radiol 27, 4516–4524 (2017). https://doi.org/10.1007/s00330-017-4867-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-4867-z