Abstract
Objectives
To develop a breast biopsy marker that resists fast and slow migration and has permanent visibility under commonly used imaging modalities.
Methods
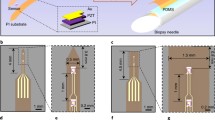
A polymer-nanoparticle composite film was prepared by embedding superparamagnetic iron oxide nanoparticles and a superelastic Nitinol wire within a flexible polyethylene matrix. MRI, mammography, and ultrasound were used to visualize the marker in agar, ex vivo chicken breast, bovine liver, brisket, and biopsy training phantoms. Fast migration caused by the “accordion effect” was quantified after simulated stereotactic, vacuum-assisted core biopsy/marker placement, and centrifugation was used to simulate accelerated long-term (i.e., slow) migration in ex vivo bovine tissue phantoms.
Results
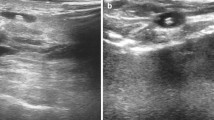
Clear marker visualization under MRI, mammography, and ultrasound was observed. After deployment, the marker partially unfolds to give a geometrically constrained structure preventing fast and slow migration. The marker can be deployed through an 11G introducer without fast migration occurring, and shows substantially less slow migration than conventional markers.
Conclusion
The polymer-nanoparticle composite biopsy marker is clearly visible on all clinical imaging modalities and does not show substantial migration, which ensures multimodal assessment of the correct spatial information of the biopsy site, allowing for more accurate diagnosis and treatment planning and improved breast cancer patient care.
Key Points
• Polymer-nanoparticle composite biopsy markers are visualized using ultrasound, MRI, and mammography.
• Embedded iron oxide nanoparticles provide tuneable contrast for MRI visualization.
• Permanent ultrasound visibility is achieved with a non-biodegradable polymer having a distinct ultrasound signal.
• Flexible polymer-based biopsy markers undergo shape change upon deployment to minimize migration.
• Non-migrating multimodal markers will help improve accuracy of pre/post-treatment planning studies.





Similar content being viewed by others
References
American College of Radiology (ACR) (2014) ACR Practice parameter for the performance of stereotactic-guided breast interventional procedures, Res 7. American College of Radiology, Reston, VA
Burbank F, Forcier N (1997) Tissue marking clip for stereotactic breast biopsy: Initial placement accuracy, long-term stability, and usefulness as a guide for wire localization. Radiology 205:407–415
Liberman L, Dershaw DD, Morris EA, Abramson AF, Thornton CM, Rosen PP (1997) Clip placement after stereotactic vacuum-assisted breast biopsy. Radiology 205:417–422
Rosen EL, Vo TT (2001) Metallic clip deployment during stereotactic breast biopsy: retrospective analysis. Radiology 218:510–516
Schell AM, Rosenkranz K, Lewis PJ (2009) Role of breast MRI in the preoperative evaluation of patients with newly diagnosed breast cancer. AJR Am J Roentgenol 192:1438–1444
Taylor KJW, Merritt C, Piccoli C et al (2002) Ultrasound as a complement to mammography and breast examination to characterize breast masses. Ultrasound Med Biol 28:19–26
Stavros AT, Thickman D, Rapp CL, Dennis MA, Parker SH, Sisney GA (1995) Solid breast nodules: use of sonography to distinguish between benign and malignant lesions. Radiology 196:123–134
Guenin MA (2000) Clip placement during sonographically guided large-core breast biopsy for mammographic-sonographic correlation. AJR Am J Roentgenol 175:1053–1055
Genson CC, Blane CE, Helvie MA, Waits SA, Chenevert TL (2007) Effects on breast MRI of artifacts caused by metallic tissue marker clips. AJR Am J Roentgenol 188:372–376
Harvey JA, Hendrick RE, Coll JM, Nicholson BT, Burkholder BT, Cohen MA (2007) Breast MR imaging artifacts: how to recognize and fix them. Radiographics 27:S131–S145
Knott PT, Mardjetko SM, Kim RH et al (2010) A comparison of magnetic and radiographic imaging artifact after using three types of metal rods: stainless steel, titanium, and vitallium. Spine J 10:789–794
Matsuura H, Inoue T, Konno H, Sasaki M, Ogasawara K, Ogawa A (2002) Quantification of susceptibility artifacts produced on high-field magnetic resonance images by various biomaterials used for neurosurgical implants. J Neurosurg 97:1472–1475
Gill A, Shellock FG (2012) Assessment of MRI issues at 3-Tesla for metallic surgical implants: findings applied to 61 additional skin closure staples and vessel ligation clips. J Cardiovasc Magn Reson 14:3
Soher BJ, Dale BM, Merkle EM (2007) A review of MR physics: 3T versus 1.5T. Magn Reson Imaging Clin N Am 15:277–290
Parikh J (2005) Delayed migration of Gel Mark Ultra clip within 15 days of 11-gauge vacuum-assisted stereotactic breast biopsy. AJR Am J Roentgenol 185:203–206
Smathers RL (2003) Marking the cavity site after stereotactic core needle breast biopsy. AJR Am J Roentgenol 180:355–356
Birdwell RL, Jackman RJ (2003) Clip or marker migration 5-10 weeks after stereotactic 11-gauge vacuum-assisted breast biopsy: report of two cases. Radiology 229:541–544
Burnside ES, Sohlich RE, Sickles EA (2001) Movement of a biopsy-site marker clip after completion of stereotactic directional vacuum-assisted breast biopsy: case report. Radiology 221:504–507
Esserman LE, Cura MA, DaCosta D (2004) Recognizing pitfalls in early and late migration of clip markers after imaging-guided directional vacuum-assisted biopsy. Radiographics 24:147–156
Harris AT (2003) Clip migration within 8 days of 11-gauge vacuum-assisted stereotactic breast biopsy: case report. Radiology 228:552–554
Parikh J (2004) Ultrasound demonstration of clip migration to skin within 6 weeks of 11-gauge vacuum-assisted stereotactic breast biopsy. Breast J 10:539–542
Philpotts LE, Lee CH (2002) Clip migration after 11-gauge vacuum-assisted stereotactic biopsy: case report. Radiology 222:794–796
Buch K, Qureshi MM, Hirsch AE, Jaffe CC, Georgian-Smith D, Hines N, Bloch BN (2014) Fast migration of breast biopsy marker placement during stereotactic core needle biopsy. Insights into Imaging 5(Suppl 1):S153. ECR 2014, Scientific Sessions, Part B. doi:10.1007/s13244-014-0317-5
Li S, Meng Lin M, Toprak MS, Kim DK, Muhammed M (2010) Nanocomposites of polymer and inorganic nanoparticles for optical and magnetic applications. Nano Rev 1:5214–5232
Hanemann T, Szabo DV (2010) Polymer-nanoparticle composites: from synthesis to modern applications. Materials 3:3468–3517
Qiao RR, Yang CH, Gao MY (2009) Superparamagnetic iron oxide nanoparticles: from preparations to in vivo MRI applications. J Mater Chem 19:6274–6293
Hu LX, He J, Hou L et al (2013) Biological evaluation of the copper/low-density polyethylene nanocomposite intrauterine device. PLoS One 8, e74128
(2007) Final report on the safety assessment of polyethylene. Int J Toxicol 26(Sup. 1):115-127
Pai SK, Whitwell G, McMurray D, Stewart TD, Stone MH (2013) Long-term results of a total knee prosthesis utilising an all polyethylene tibial component. Arch Orthop Trauma Surg 133:1143–1148
Schwenk MH (2010) Ferumoxytol: a new intravenous iron preparation for the treatment of iron deficiency anemia in patients with chronic kidney disease. Pharmacotherapy 30:70–79
Spinowitz BS, Kausz AT, Baptista J et al (2008) Ferumoxytol for treating iron deficiency anemia in CKD. J Am Soc Nephrol 19:1599–1605
Bellin MF, Roy C, Kinkel K et al (1998) Lymph node metastases: safety and effectiveness of MR imaging with ultrasmall superparamagnetic iron oxide particles- initial clinical experience. Radiology 207:799–808
Christen T, Ni W, Qiu DQ et al (2013) High-resolution cerebral blood volume imaging in humans using the blood pool contrast agent ferumoxytol. Magn Reson Med 70:705–710
Reimer P, Balzer T (2003) Ferucarbotran (Resovist): a new clinically approved RES-specific contrast agent for contrast-enhanced MRI of the liver: properties, clinical development, and applications. Eur Radiol 13:1266–1276
Reimer P, Rummeny EJ, Daldrup HE et al (1995) Clinical results with Resovist-A phase-2 clincal trial. Radiology 195:489–496
DeMartini WB, Ichikawa L, Yankaskas BC et al (2010) Breast MRI in community practice: Equipment and imaging techniques at facilities in the Breast Cancer Surveillance Consortium. J Am Coll Radiol 7:878–884
Lee CH, Dershaw DD, Kopans P et al (2010) Breast cancer screening with imaging: Recommendations from the Society of Breast Imaging and the ACR on the use of mammography, breast MRI, breast ultrasound, and other technologies for the detection of clinically occult breast cancer. J Am Coll Radiol 7:18–27
Mann RM, Kuhl CK, Kinkel K, Boetes C (2008) Breast MRI: guidelines from the European Society of Breast Imaging. Eur Radiol 18:1307–1318
Orel S (2008) Who should have breast magnetic resonance imaging evaluation? J Clin Oncol 26:703–711
Parker A, Schroen A, Brenin D (2013) MRI utilization in newly diagnosed breast cancer: a survey of practicing surgeons. Ann Surg Oncol 20:2600–2606
Siegmann KC, Speck S, Baur A et al (2009) Einsatz eines speziellen clips (Tumark® Professional) zur postinterventionellen markierung suspekter mammaläsionen nach MRT-gestützter vakuumbiopsie-erst ergebnisse. Fortschr Röntgenstr 181:147–154
Viehweg P, Fabel K, Petzold A, Friedrich K, Laniado M (2007) Einsatz des O-Twist Markers zur lokalisation von mammakarzinomen unter neoadjuvanter chemotherapie-erste ergebnisse. Fortschr Röntgenstr 179:1055–1060
Acknowledgements
The authors thank the Coulter Foundation, Boston University School of Medicine, and Boston University for support of this research. The scientific guarantors of this publication are B. Nicolas Bloch and Mark Grinstaff. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. This study has received funding by the Coulter Translational Partnership (CTP) program in Biomedical Engineering. No complex statistical methods were necessary for this paper. Institutional Review Board approval was not obtained. Institutional Review Board approval was not required because this was a technical development and prototype study using phantoms without involvement of patients or animals. None of the material or part of this study was previously published. Methodology: prospective, experimental, performed at one institution.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Kaplan, J.A., Grinstaff, M.W. & Bloch, B.N. Polymer film-nanoparticle composites as new multimodality, non-migrating breast biopsy markers. Eur Radiol 26, 866–873 (2016). https://doi.org/10.1007/s00330-015-3852-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3852-7