Abstract
Objectives
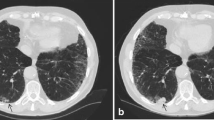
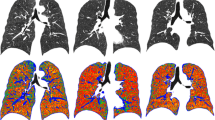
To evaluate interobserver agreement and time-trend in chest CT assessment of emphysema, airways, and interstitial abnormalities in a lung cancer screening cohort.
Methods
Visual assessment of baseline and fifth-year examination of 1990 participants was performed independently by two observers. Results were standardised by means of an electronic score sheet; kappa and time-trend analyses were performed.
Results
Interobserver agreement was substantial in early emphysema diagnosis; highly significant (p < 0.001) time-trends in both emphysema presence and grading were found (higher prevalence and grade of emphysema in late CT examinations). Significant progression in emphysema was seen in continuous smokers, but not in former smokers. Agreement on centrilobular emphysema subtype was substantial; agreement on paraseptal subtype, moderate. Agreement on panlobular and mixed subtypes was only fair. Agreement was fair regarding airway analysis. Interstitial abnormalities were infrequent in the cohort, and agreement on these was fair to moderate. A highly significant time-trend was found regarding interstitial abnormalities, which were more frequent in late examinations.
Conclusions
Visual scoring of chest CT is able to characterise the presence, pattern, and progression of early emphysema. Continuous smokers progress; former smokers do not.
Key Points
• Substantial interobserver consistency in determining early-stage emphysema in low-dose CT.
• Longitudinal analyses show clear time-trends for emphysema presence and grading.
• For continuous smokers, progression of emphysema was seen in all lung zones.
• For former smokers, progression of emphysema was undetectable by visual assessment.
• Onset and progression of interstitial abnormalities are visually detectable.


Similar content being viewed by others
Abbreviations
- CT:
-
Computed tomography
- COPD:
-
Chronic obstructive pulmonary disease
- HU:
-
Hounsfield units
- ILD:
-
Interstitial lung disease
- UIP:
-
Usual interstitial pneumonia
References
Lynch DA, Godwin JD, Safrin S et al (2005) High-resolution computed tomography in idiopathic pulmonary fibrosis: diagnosis and prognosis. Am J Respir Crit Care Med 4:488–493
Gietema HA, Muller NL, Fauerbach PV et al (2011) Quantifying the extent of emphysema: factors associated with radiologists’ estimations and quantitative indices of emphysema severity using the ECLIPSE cohort. Acad Radiol 6:661–671
Sverzellati N, Devaraj A, Desai SR et al (2011) Method for minimizing observer variation for the quantitation of high-resolution computed tomographic signs of lung disease. J Comput Assist Tomogr 5:596–601
Hansell DM (2001) Computed tomography of diffuse lung disease: functional correlates. Eur Radiol 9:1666–1680
Mets OM, Smit EJ, Mohamed Hoesein FA et al (2012) Visual versus automated evaluation of chest computed tomography for the presence of chronic obstructive pulmonary disease. PLoS One 7:e42227
Rabe KF, Hurd S, Anzueto A et al (2007) Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 6:532–555
Gurney JW, Jones KK, Robbins RA et al (1992) Regional distribution of emphysema: correlation of high-resolution CT with pulmonary function tests in unselected smokers. Radiology 2:457–463
Kakinuma R, Ashizawa K, Kuriyama K et al (2012) Measurement of focal ground-glass opacity diameters on CT images: interobserver agreement in regard to identifying increases in the size of ground-glass opacities. Acad Radiol 4:389–394
Watadani T, Sakai F, Johkoh T et al (2013) Interobserver variability in the CT assessment of honeycombing in the lungs. Radiology 3:936–944
Barr RG, Berkowitz EA, Bigazzi F et al (2012) A combined pulmonary-radiology workshop for visual evaluation of COPD: study design, chest CT findings and concordance with quantitative evaluation. COPD 2:151–159
Grenier P, Mourey-Gerosa I, Benali K et al (1996) Abnormalities of the airways and lung parenchyma in asthmatics: CT observations in 50 patients and inter- and intraobserver variability. Eur Radiol 2:199–206
Ng CS, Desai SR, Rubens MB et al (1999) Visual quantitation and observer variation of signs of small airways disease at inspiratory and expiratory CT. J Thorac Imaging 4:279–285
Thomsen LH, Dirksen A, Shaker SB et al (2014) Analysis of FEV decline in relatively healthy heavy smokers: implications of expressing changes in FEV in relative terms. COPD 11:96–104
Shaker SB, Dirksen A, Lo P et al (2012) Factors influencing the decline in lung density in a Danish lung cancer screening cohort. Eur Respir J 5:1142–1148
Pedersen JH, Ashraf H, Dirksen A et al (2009) The Danish randomized lung cancer CT screening trial–overall design and results of the prevalence round. J Thorac Oncol 5:608–614
Hansell DM, Bankier AA, MacMahon H et al (2008) Fleischner Society: glossary of terms for thoracic imaging. Radiology 3:697–722
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 1:159–174
Lo P, Sporring J, Ashraf H, Pedersen JJ, de Bruijne M (2010) Vessel-guided airway tree segmentation: a voxel classification approach. Med Image Anal 4:527–538
Dijkstra AE, Postma DS, ten Hacken N et al (2013) Low-dose CT measurements of airway dimensions and emphysema associated with airflow limitation in heavy smokers: a cross sectional study. Respir Res 14:11
Wille MMW, Petersen J, Dirksen A, Pedersen JH, De Bruijne M (2013) Airway distensibility in chronic obstructive pulmonary disease – evaluation by CT airway segmentation and lung density measurement based on the Danish Lung Cancer Screening Trial. AJRCCM:A2871
Hasegawa M, Nasuhara Y, Onodera Y et al (2006) Airflow limitation and airway dimensions in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 12:1309–1315
Kazantzi A, Costaridou L, Skiadopoulos S et al (2014) Automated 3D iotanterstitial lung disease epsilonxtent quantification: performance evaluation and correlation to PFTs. J Digit Imaging 27(3):380–391
Acknowledgments
The scientific guarantor of this publication is Professor Asger Dirksen, MD, DMSc. The authors of this manuscript declare no relationship with any companies whose products or services may be related to the subject matter of the article. This study has received funding from the Danish Ministry of Interior and Health. One of the authors has significant statistical expertise. Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Some study subjects or cohorts have been previously reported in studies regarding lung cancer screening, nodule characteristics, lung function, and lung density in the Danish Lung Cancer Screening Trial. However, visual assessment of emphysema, airway abnormalities, and interstitial abnormalities was not previously performed, and thus the data of this study are new and have not yet been published. All relevant references are disclosed. Methodology: prospective randomised intervention trial, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wille, M.M.W., Thomsen, L.H., Dirksen, A. et al. Emphysema progression is visually detectable in low-dose CT in continuous but not in former smokers. Eur Radiol 24, 2692–2699 (2014). https://doi.org/10.1007/s00330-014-3294-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3294-7