Abstract
Objective
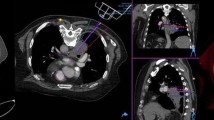
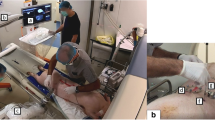
To compare the accuracy of a robotic interventional radiologist (IR) assistance platform with a standard freehand technique for computed-tomography (CT)-guided biopsy and simulated radiofrequency ablation (RFA).
Methods
The accuracy of freehand single-pass needle insertions into abdominal phantoms was compared with insertions facilitated with the use of a robotic assistance platform (n = 20 each). Post-procedural CTs were analysed for needle placement error. Percutaneous RFA was simulated by sequentially placing five 17-gauge needle introducers into 5-cm diameter masses (n = 5) embedded within an abdominal phantom. Simulated ablations were planned based on pre-procedural CT, before multi-probe placement was executed freehand. Multi-probe placement was then performed on the same 5-cm mass using the ablation planning software and robotic assistance. Post-procedural CTs were analysed to determine the percentage of untreated residual target.
Results
Mean needle tip-to-target errors were reduced with use of the IR assistance platform (both P < 0.0001). Reduced percentage residual tumour was observed with treatment planning (P = 0.02).
Conclusion
Improved needle accuracy and optimised probe geometry are observed during simulated CT-guided biopsy and percutaneous ablation with use of a robotic IR assistance platform. This technology may be useful for clinical CT-guided biopsy and RFA, when accuracy may have an impact on outcome.
Key points:
• A recently developed robotic intervention radiology assistance platform facilitates CT-guided interventions.
• Improved accuracy of complex needle insertions is achievable.
• IR assistance platform use can improve target ablation coverage.





Similar content being viewed by others
Abbreviations
- IR:
-
Interventional radiologist
- RFA:
-
Radiofrequency ablation
References
Wood BJ, Ramkaransingh JR, Fojo T et al (2002) Percutaneous tumor ablation with radiofrequency. Cancer 94:443–451
Chintapalli KN, Montgomery RS, Hatab M et al (2012) Radiation dose management: part 1, minimizing radiation dose in CT-guided procedures. AJR Am J Roentgenol 198:W347–W351
Magnusson A, Akerfeldt D (1991) CT-guided core biopsy using a new guidance device. Acta Radiol 32:83–85
Onik G, Cosman ER, Wells THJ et al (1988) CT-guided aspirations for the body: comparison of hand guidance with stereotaxis. Radiology 166:389–394
Bertot LC, Sato M, Tateishi R et al (2011) Mortality and complication rates of percutaneous ablative techniques for the treatment of liver tumors: a systematic review. Eur Radiol 21:2584–2596
Tiong L, Maddern GJ (2011) Systematic review and meta-analysis of survival and disease recurrence after radiofrequency ablation for hepatocellular carcinoma. Br J Surg 98:1210–1224
Salhab M, Canelo R (2011) An overview of evidence-based management of hepatocellular carcinoma: a meta-analysis. J Cancer Res Ther 7:463
Cirocchi R, Trastulli S, Boselli C et al (2012) Radiofrequency ablation in the treatment of liver metastases from colorectal cancer. Cochrane Database Syst Rev 6, CD006317
Best SL, Park SK, Yaacoub RF et al (2012) Long-term outcomes of renal tumor radio frequency ablation stratified by tumor diameter: size matters. JURO 187:1183–1189
Hui GC, Tuncali K, Tatli S et al (2008) Comparison of percutaneous and surgical approaches to renal tumor ablation: metaanalysis of effectiveness and complication rates. J Vasc Interv Radiol 19:1311–1320
Pleguezuelo M, Marelli L, Misseri M et al (2008) TACE versus TAE as therapy for hepatocellular carcinoma. Expert Rev Anticancer Ther 8:1623–1641
Minami Y, Kudo M (2011) Radiofrequency ablation of hepatocellular carcinoma: a literature review. Int J Hepatol 2011:1–9
Solomon SB, Patriciu A, Bohlman ME et al (2002) Robotically driven interventions: a method of using CT fluoroscopy without radiation exposure to the physician. Radiology 225:277–282
Patriciu A, Awad M, Solomon SB et al (2005) Robotic assisted radio-frequency ablation of liver tumors—randomized patient study. Med Image Comput Comput Assist Interv 8:526–533
Stoffner R, Augschöll C, Widmann G et al (2009) Accuracy and feasibility of frameless stereotactic and robot-assisted CT-based puncture in interventional radiology: a comparative phantom study. Rofo 181:851–858
Cleary K, Melzer A, Watson V et al (2006) Interventional robotic systems: applications and technology state of the art. Minim Invasive Ther Allied Technol 15:101–113
Schulz B, Eichler K, Siebenhandl P et al (2012) Accuracy and speed of robotic assisted needle interventions using a modern cone beam computed tomography intervention suite: a phantom study. Eur Radiol 23:198–204
Zangos S, Melzer A, Eichler K et al (2011) MR-compatible assistance system for biopsy in a high-field-strength system: initial results in patients with suspicious prostate lesions. Radiology 259:903–910
Schell B, Eichler K, Mack MG et al (2012) Robot-assisted biopsies in a high-field MRI system—first clinical results. Rofo 184:42–47
Stoll M, Boettger T, Schulze C, Hastenteufel M (2012) Transfer of methods from radiotherapy planning to ablation planning with focus on uncertainties and robustness. Biomed Tech (Berl). doi:10.1515/bmt-2012-4279
Lehmann KS, Frericks BB, Holmer C et al (2011) In vivo validation of a therapy planning system for laser-induced thermotherapy (LITT) of liver malignancies. Int J Color Dis 26:799–808
McCreedy ES, Cheng R, Hemler PF et al (2006) Radio frequency ablation registration, segmentation, and fusion tool. IEEE Trans Inf Technol Biomed 10:490–496
Covidien (2009) Cool-tipTM RF ablation system [Pamphlet]. Covidien, Boulder
Kobayashi K, Bhargava P, Raja S et al (2012) Image-guided biopsy: what the interventional radiologist needs to know about PET/CT. Radiographics 32:1483–1501
Solomon SB, Silverman SG (2010) Imaging in interventional oncology. Radiology 257:624–640
Wood BJ, Locklin JK, Viswanathan A et al (2007) Technologies for guidance of radiofrequency ablation in the multimodality interventional suite of the future. J Vasc Interv Radiol 18:9–24
Wood BJ, Zhang H, Durrani A et al (2005) Navigation with electromagnetic tracking for interventional radiology procedures: a feasibility study. J Vasc Interv Radiol 16:493–505
Hong CW, Xu S, Imbesi KL, Wood BJ (2013) Integrated laser-guided CT biopsy. Clin Imaging. doi:10.1016/j.clinimag.2013.08.006
Wood BJ, Kruecker J, Abi-Jaoudeh N et al (2010) Navigation systems for ablation. J Vasc Interv Radiol 21:S257–S263
Su L-M, Stoianovici D, Jarrett TW et al (2002) Robotic percutaneous access to the kidney: comparison with standard manual access. J Endourol 16:471–475
Acknowledgements
A year-long research fellowship for Y.K. was made possible through the National Institutes of Health (NIH) Medical Research Scholars Program, a public-private partnership supported jointly by the NIH and generous contributions to the Foundation for the NIH from Pfizer Inc., The Leona M. and Harry B. Helmsley Charitable Trust, and the Howard Hughes Medical Institute, as well as other private donors. For a complete list, please visit the Foundation website at http://www.fnih.org/work/programs-development/medical-research-scholars-program). The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
X.S.: No potential conflicts of interest to disclose.
G.V. is a full-time salaried employee (Principle Systems Architect, ATO) of Perfint Healthcare Pvt. Ltd. Perfint Healthcare owns intellectual property related to technologies used in this published work, including USPTO # US20130072784, US20120190970, US20130085380, etc. For detailed information, please visit the company website, www.perfinthealthcare.com.
B.J.W. and A.M.V: This research was supported by the NIH Intramural Research Program and the NIH Center for Interventional Oncology. The interventional radiologist assistance platform was supplied by Perfint Healthcare Pvt. Ltd. (Chennai, India) under a Materials Transfer Agreement between the NIH Center for Interventional Oncology and Perfint Healthcare. NIH and Perfint Healthcare have discussed details of a draft Cooperative Research and Development Agreement (CRADA). The content does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products or organisations imply endorsement by the U.S. Government.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koethe, Y., Xu, S., Velusamy, G. et al. Accuracy and efficacy of percutaneous biopsy and ablation using robotic assistance under computed tomography guidance: a phantom study. Eur Radiol 24, 723–730 (2014). https://doi.org/10.1007/s00330-013-3056-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-013-3056-y