Abstract
Various biological studies suggest that the corneal epithelium is maintained by active stem cells located in the limbus, the so-called limbal epithelial stem cell hypothesis. While numerous mathematical models have been developed to describe corneal epithelium wound healing, only a few have explored the process of corneal epithelium homeostasis. In this paper we present a purposefully simple stochastic mathematical model based on a chemical master equation approach, with the aim of clarifying the main factors involved in the maintenance process. Model analysis provides a set of constraints on the numbers of stem cells, division rates, and the number of division cycles required to maintain a healthy corneal epithelium. In addition, our stochastic analysis reveals noise reduction as the epithelium approaches its homeostatic state, indicating robustness to noise. Finally, recovery is analysed in the context of perturbation scenarios.










Similar content being viewed by others
References
Ahmad S (2012) Concise review: limbal stem cell deficiency, dysfunction, and distress. Stem Cells Transl Med 1(2):110–115
Alarcon T, Getto P, Marciniak-Czochra A, dM Vivanco M (2011) A model for stem cell population dynamics with regulated maturation delay. Conference Publications (Special):32–43
Artal P, Tabernero J (2008) The eye’s aplanatic answer. Nat Photon 2:586–589
Beebe D, Masters B (1996) Cell lineage and the differentiation of corneal epithelial cells. Investig Ophthalmol Vis Sci 37(9):1815–1825
Bertalanffy F, Lau C (1962) Mitotic rate and renewal time of the corneal epithelium in the rat. Arch Ophthalmol 68(4):546–550
Boman B, Fields J, Bonham-Carter O, Runquist O (2001) Computer modeling implicates stem cell overproduction in colon cancer initiation. Cancer Res 61(23):8408–8411
Cabrera C, Wagner L, Schork M, Bohrand D, Cohan B (1999) Intraocular pressure measurement in the conscious rat. Acta Ophthalmol Scand 77(1):33–36
Castro-Muñozledo F (1994) Development of a spontaneous permanent cell line of rabbit corneal epithelial cells that undergoes sequential stages of differentiation in cell culture. J Cell Sci 107(8):2343–2351
Chan E, Chen L, Rao J, Yu F, Deng S (2015) Limbal basal cell density decreases in limbal stem cell deficiency. Am J Ophthalmol 160(4):678–684
Chen J, Tseng S (1990) Corneal epithelial wound healing in partial limbal deficiency. Investig Ophthalmol Vis Sci 31(7):1301–1314
Chen J, Tseng S (1991) Abnormal corneal epithelial wound healing in partial-thickness removal of limbal epithelium. Investig Ophthalmol Vis Sci 32(8):2219–2233
Dale P, Maini P, Sherratt J (1994a) Mathematical modeling of corneal epithelial wound healing. Math Biosci 124(2):127–147
Dale P, Sherratt J, Maini P (1994b) The speed of corneal epithelial wound healing. Appl Math Lett 7(2):11–14
Daniels J, Dart J, Tuft S, Khaw P (2001) Corneal stem cells in review. Wound Repair Regen 9(6):483–494
Davanger M, Evensen A (1971) Role of the pericorneal papillary structure in renewal of corneal epithelium. Nature 229(5286):560–561
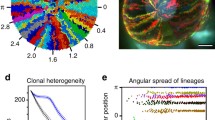
Di Girolamo N, Bobba S, Raviraj V, Delic N, Slapetova I, Nicovich P, Halliday G, Wakefield D, Whan R, Lyons J (2015) Tracing the fate of limbal epithelial progenitor cells in the murine cornea. Stem Cells 33(1):157–169
Dorá N, Hill R, Collinson J, West J (2015a) Corneal stem cells in review. Stem Cell Res 15(3):665677
Dorà N, Hill R, Collinson J, West J (2015b) Lineage tracing in the adult mouse corneal epithelium supports the limbal epithelial stem cell hypothesis with intermittent periods of stem cell quiescence. Stem Cell Res 15(3):665–677
Douvaras P, Mort R, Edwards D, Ramaesh K, Dhillon B, Morley S, Hill R, West J (2013) Increased corneal epithelial turnover contributes to abnormal homeostasis in the \(Pax6^{+/-}\) mouse model of aniridia. PLoS ONE 8(8):e71117
Dua H, Gomes J, Singh A (1994) Corneal epithelial wound healing. Br J Ophthalmol 78(5):401–408
Ebrahimi M, Taghi-Abadi E, Baharvand H (2009) Limbal stem cells in review. J Ophthalmic Vis Res 4(1):40–58
Elf J, Ehrenberg M (2003) Fast evaluation of fluctuations in biochemical networks with the linear noise approximation. Genome Res 13(11):2475–2484
Erban R, Chapman J, Maini P (2007) A practical guide to stochastic simulations of reaction-diffusion processes. arXiv preprint arXiv:0704.1908
Espana E, Grueterich M, Romano A, Touhami A, Tseng S (2002) Idiopathic limbal stem cell deficiency. Ophthalmology 109(11):2004–2010
Gerike T, Paulus U, Potten C, Loeffler M (1998) A dynamic model of proliferation and differentiation in the intestinal crypt based on a hypothetical intraepithelial growth factor. Cell Prolif 31(2):93–110
Gillespie D (1992) A rigorous derivation of the chemical master equation. Phys A Stat Mech Appl 188(1):404–425
Grima R (2008) Multiscale modeling of biological pattern formation. Curr Top Dev Biol 81:435–460
Grima R (2010) An effective rate equation approach to reaction kinetics in small volumes: theory and application to biochemical reactions in nonequilibrium steady-state conditions. J Chem Phys 133(3):035101
Grima R, Newman TJ (2004) Accurate discretization of advection–diffusion equations. Phys Rev E Stat Nonlinear Soft Matter Phys 70(3 Pt 2):036703
Hanna C, O’Brien J (1960) Cell production and migration in the epithelial layer of the cornea. Arch Ophthalmol 64(4):536–539
Johnston M, Edwards C, Bodmer W, Maini P, Chapman S (2007) Mathematical modeling of cell population dynamics in the colonic crypt and in colorectal cancer. Proc Natl Acad Sci 104(10):4008–4013
Kefalov V (2010) Encyclopedia of the eye. Encycl Eye 3:389–396
Klein A, Simons B (2011) Universal patterns of stem cell fate in cycling adult tissues. Development 138(15):3103–3111
Klyce S (1972) Electrical profiles in the corneal epithelium. J Physiol 226(2):407–429
Kruse F, Chen J, Tsai R, Tseng S (1990) Conjunctival transdifferentiation is due to the incomplete removal of limbal basal epithelium. Investig Ophthalmol Vis Sci 31(9):1903–1913
Lehrer M, Sun T, Lavker R (1998) Strategies of epithelial repair: modulation of stem cell and transit amplifying cell proliferation. J Cell Sci 111(19):2867–2875
Liaw J, Rojanasakul Y, Robinson J (1992) The effect of drug charge type and charge density on corneal transport. Int J Pharm 88(1–3):111–124
Liu L, Rando T (2011) Manifestations and mechanisms of stem cell aging. J Cell Biol 193(2):257–266
Lobo E, Delic N, Richardson A, Raviraj V, Halliday G, Di Girolamo N, Myerscough M, Lyons J (2016) Self-organized centripetal movement of corneal epithelium in the absence of external cues. Nat Commun 7:12388
Majo F, Rochat A, Nicolas M, Jaoudé G, Barrandon Y (2008) Oligopotent stem cells are distributed throughout the mammalian ocular surface. Nature 456(7219):250–254
Marciniak-Czochra A, Stiehl T, Ho A, Jäger W, Wagner W (2009) Modeling of asymmetric cell division in hematopoietic stem cellsregulation of self-renewal is essential for efficient repopulation. Stem Cells Dev 18(3):377–386
Marshall J (1985) Radiation and the ageing eye. Ophthalmic Physiol Opt 5(3):241–263
Meek K, Knupp C (2015) Corneal structure and transparency. Prog Retin Eye Res 49:1–16
Meineke F, Potten C, Loeffler M (2001) Cell migration and organization in the intestinal crypt using a lattice-free model. Cell Prolif 34(4):253–266
Morrison S, Kimble J (2006) Asymmetric and symmetric stem-cell divisions in development and cancer. Nature 441(7097):1068–1074
Mort R, Douvaras P, Morley S, Dorà N, Hill R, Collinson J, West J (2012) Stem cells and corneal epithelial maintenance: insights from the mouse and other animal models. Results Probl Cell Differ 55:357–394
Nagasaki T, Zhao J (2003) Centripetal movement of corneal epithelial cells in the normal adult mouse. Investig Ophthalmol Vis Sci 44(2):558–566
Nalapareddy K, Nattamai K, Kumar R, Karns R, Wikenheiser-Brokamp K, Sampson L, Mahe M, Sundaram N, Yacyshyn MB, Yacyshyn B et al (2017) Canonical Wnt signaling ameliorates aging of intestinal stem cells. Cell Rep 18(11):2608–2621
Oshima Y, Sakamoto T, Yamanaka I, Nishi T, Ishibashi T, Inomata H (1998) Targeted gene transfer to corneal endothelium in vivo by electric pulse. Gene Ther 5(10):1347–1354
Pal-Ghosh S, Pajoohesh-Ganji A, Brown M, Stepp M (2004) A mouse model for the study of recurrent corneal epithelial erosions: \(\alpha 9 \eta 1\) integrin implicated in progression of the disease. Investig Ophthalmol Vis Sci 45(6):1775–1788
Paulsson J (2005) Models of stochastic gene expression. Phys Life Rev 2(2):157–175
Paulus U, Potten C, Loeffler M (1992) A model of the control of cellular regeneration in the intestinal crypt after perturbation based solely on local stem cell regulation. Cell Prolif 25(6):559–578
Paulus U, Loeffler M, Zeidler J, Owen G, Potten S (1993) The differentiation and lineage development of goblet cells in the murine small intestinal crypt: experimental and modelling studies. J Cell Sci 106(2):473–483
Pellegrini G, Golisano O, Paterna P, Lambiase A, Bonini S, Rama P, De Luca M (1999) Location and clonal analysis of stem cells and their differentiated progeny in the human ocular surface. J Cell Biol 145(4):769–782
Puangsricharern V, Tseng S (1995) Cytologlogic evidence of corneal diseases with limbal stem cell deficiency. Ophthalmology 102(10):1476–1485
Rao C, Wolf D, Arkin A (2002) Control, exploitation and tolerance of intracellular noise. Nature 420(6912):231–237
Reinstein D, Archer T, Gobbe M, Coleman D, Silverman R et al (2008) Epithelial thickness in the normal cornea: three-dimensional display with artemis very high-frequency digital ultrasound. J Refract Surg 24(6):571–581
Rhee J, Nejad T, Comets O, Flannery S, Gulsoy E, Iannaccone P, Foster C (2015) Promoting convergence: the phi spiral in abduction of mouse corneal behaviors. Complexity 20(3):22–38
Richardson A, Lobo E, Delic N, Myerscough M, Lyons J, Wakefield D, Di Girolamo N (2017) Keratin-14-positive precursor cells spawn a population of migratory corneal epithelia that maintain tissue mass throughout life. Stem Cell Rep 9(4):1081–1096
Romano AC, Espana EM, Yoo SH, Budak MT, Wolosin JM, Tseng SC (2003) Different cell sizes in human limbal and central corneal basal epithelia measured by confocal microscopy and flow cytometry. Investig Ophthalmol Vis Sci 44(12):5125–5129
Ruberti J, Roy A, Roberts C (2011) Corneal structure and function. Annu Rev Biomed Eng 13:269–295
Rüfer F, Schröder A, Erb C (2005) White-to-white corneal diameter: normal values in healthy humans obtained with the orbscan II topography system. Cornea 24(3):259–261
Saghizadeh M, Kramerov A, Svendsen C, Ljubimov A (2017) Concise review: stem cells for corneal wound healing. Stem Cells (Dayton, Ohio) 35(10):2105–2114
Schnoerr D, Sanguinetti G, Grima R (2017) Approximation and inference methods for stochastic biochemical kinetics—a tutorial review. J Phys A Math Theor 50(9):093001
Shanmuganathan V, Foster T, Kulkarni B, Hopkinson A, Gray T, Powe D, Lowe J, Dua H (2007) Morphological characteristics of the limbal epithelial crypt. Br J Ophthalmol 91(4):514–519
Sharma A, Coles W (1989) Kinetics of corneal epithelial maintenance and graft loss. A population balance model. Investig Ophthalmol Vis Sci 30(9):1962–1971
Sheardown H, Cheng YL (1996) Mechanisms of corneal epithelial wound healing. Chem Eng Sci 51(19):4517–4529
Sherratt J, Murray J (1990) Models of epidermal wound healing. Proc R Soc Lond B Biol Sci 241(1300):29–36
Sherratt J, Murray J (1991) Mathematical analysis of a basic model for epidermal wound healing. J Math Biol 29(5):389–404
Sherratt J, Murray J (1992) Epidermal wound healing: the clinical implications of a simple mathematical model. Cell Transpl 1:365–371
Sun T, Tseng S, Lavker R (2010) Location of corneal epithelial stem cells. Nature 463(7284):E10–E11
Thoft R, Friend J (1983) The X, Y, Z hypothesis of corneal epithelial maintenance. Investig Ophthalmol Vis Sci 24(10):1442–1443
Thomas P, Matuschek H, Grima R (2013) How reliable is the linear noise approximation of gene regulatory networks? BMC Genom 14(Suppl 4):S5
Toropainen E (2007) Corneal epithelial cell culture model for pharmaceutical studies. PhD thesis, University of Kuopio, Finland
Tseng S et al (1989) Concept and application of limbal stem cells. Eye 3(Pt 2):141–157
Tsonis P (2011) Animal models in eye research. Academic Press, New York
Urbanowicz M, Zhao J, Nagasaki T (2011) Spatial distribution of cell divisions in the basal epithelium of mouse cornea. Technical report 52 (ARVO Meeting Abstracts April 22, 2011): E-abstract 320, Investigative Ophthalmology & Visual Science
Watsky M, Olsen T, Edelhauser H (1995) Cornea and sclera. Foundations of Duanes clinical ophthalmology 2
Wiley L, SundarRaj N, Sun T, Thoft R (1991) Regional heterogeneity in human corneal and limbal epithelia: an immunohistochemical evaluation. Investig Ophthalmol Vis Sci 32(3):594–602
Wilson A, Laurenti E, Oser G, van der Wath R, Blanco-Bose W, Jaworski M, Offner S, Dunant C, Eshkind L, Bockamp E, Lió P, MacDonald H, Trumpp A (2008) Hematopoietic stem cells reversibly switch from dormancy to self-renewal during homeostasis and repair. Cell 135:11181129
Yoon J, Ismail S, Sherwin T (2014) Limbal stem cells: central concepts of corneal epithelial homeostasis. World J Stem Cells 6(4):391–403
Zieske J (1994) Perpetuation of stem cells in the eye. Eye (London, England) 8(Pt 2):163–169
Acknowledgements
The authors would like to thank Dr. John D. West (University of Edinburgh) for his valuable help in understanding the underlying mechanisms of the corneal epithelial maintaining process and the data provided. Eleni Moraki was supported by The Maxwell Institute Graduate School in Analysis and its Applications, a Centre for Doctoral Training funded by the UK Engineering and Physical Sciences Research Council (Grant EP/L016508/01), the Scottish Funding Council, Heriot-Watt University and the University of Edinburgh. Ramon Grima would like to acknowledge funding from BBSRC Grant BB/M025551/1. Kevin J. Painter would like to acknowledge Politecnico di Torino for a Visiting Professor position and funding from BBSRC Grant BB/J015940/1.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix A Parameter estimations
1.1 A.1 Mouse
We first note that the corneal circumference of a mouse is \(\sim 10{,}000\,\upmu \hbox {m} \) (Di Girolamo et al. 2015; Dorá et al. 2015a; Dorà et al. 2015b) and a typical basal cell diameter is \(\sim 10\,\upmu \hbox {m} \) (Romano et al. 2003). If stem cells simply formed a one-cell thick ring, a total stem cell population of \(\sim 1000\) cells could be accommodated along the corneal-limbal border. Note, however, that an estimated 250–300 are active (Dorá et al. 2015a; Dorà et al. 2015b) at homeostasis. To accommodate scenarios that can range from healthy to pathological, or eye sizes from larger to smaller, we assume the number of SCa in the limbus ranges between 100 and 1000.
Although the cornea is dome-shaped, for the purposes of the model we have assumed it is a hemisphere with a circumference of approximately 10, 000 \(\upmu \hbox {m}\). Then, the radius of the corneal is \( r_{corneal}=1592\)\( \upmu \hbox {m} \), from which the corneal area is \( A_{corneal}=2 \pi r^{2}_{corneal}\)\(\upmu \hbox {m}^{2} \). Similarly, the average area occupied by a basal corneal cell (assuming that the cell is a disc in the 2D plane) is \( A_{cell}=\pi r^{2}_{cell}\)\(\upmu \hbox {m}^{2} \), where \(r_{cell}=5\)\(\upmu \hbox {m} \). Thus, an estimate of cells that can fit in the corneal epithelium is given by:
and to take into account not just the normal conditions, we can introduce the magnitude of \( 10^{5} \) as a guideline baseline value for the number of cells required to populate a small cornea.
For mouse we have a number of sources that provide indications of stem cell and TAC division rates. If it is assumed that mouse limbal epithelial SCs are equivalent to BrdU “label-retaining cells”, which include slow-cycling stem cells, it can be estimated that certain limbal epithelial SCs do not divide more often than once per two weeks (\(\sim 14\) days). This calculation follows from detectable BrdU retention for at least 10 weeks (Douvaras et al. 2013), and that BrdU is probably diluted to undetectable levels after 4–5 cell divisions (Wilson et al. 2008). However, this is quite likely to provide an approximate lower bound for division rates, as it remains quite possible that certain SCs divide significantly more quickly and may not be detected by the label-retaining cell approach. As such, the mean SC cell cycle time may be considerably less than 2 weeks. Of course division rates are ultimately bounded by the minimum length of time needed to complete the cell cycle, which would be of the order of several hours to a day. Consequently, we take a range 6 h to 16 days for (active) stem cell doubling times.
Experimental studies on the TAC cell cycle in the peripheral corneal epithelium indicate that almost \(50\%\) of basal corneal epithelial cells are in S-phase of the cell cycle, during a 24-h labelling period (Urbanowicz et al. 2011). This suggests a minimum cell doubling time of just over 2 days but it would be longer if certain TACs cycle more slowly. Similarly, an average mitotic rate of \(37\%\) of basal layer cells per day can be derived for rats from the results reported by Bertalanffy and Lau (1962) and this suggests a minimum cell doubling time of about 2.7 days. (The original results showed that \(14.5\%\) of all corneal epithelial cells divided per day and results for the mouse imply that about \(38.8\%\) of mouse corneal epithelial cells are in the basal layer (Douvaras et al. 2013)). Other experiments on the TAC cell cycle in the peripheral corneal epithelium have estimated it as approximately as 72 h for the mouse (Lehrer et al. 1998). Overall the results show that the average doubling time for TACs is about once every 2–3 days but may be longer in the central corneal epithelium (Lehrer et al. 1998). While we centre on an average rate of 2 days, for our studies we again use a range of 6 h to 16 days to include scenarios under normal and abnormal conditions.
1.2 A.2 Human
Experimental data suggests that the average corneal diameter in human eye is \( 11.71\pm 0.42 \,\hbox {mm}\), (Rüfer et al. 2005) implying a corneal circumference \(\sim 36.770\,\hbox {mm}^{2} \). In the absence of specific data, we consider an analogous case to the mouse and suppose the circumference corresponds to the corneal-limbal border. Assuming limbal corneal cells are \(10 \,\upmu \hbox {m} \) in diameter, we estimate that there is a room for \(\sim \) 3000–40000 limbal cells forming a one-cell thick ring; although (in contrast to the mouse case) some biological studies suggest that they are asymmetrically distributed (Wiley et al. 1991; Pellegrini et al. 1999; Shanmuganathan et al. 2007). If a similar fraction (to that of mouse) of this population is taken to be active, we estimate \(\sim 1000\) active stem cells (\( SC_{a} \)) in the human limbus. Again, we consider an order of magnitude range about this value (\(\sim \) 400–4000).
Using the same calculations adapted from the mouse case gives an order of magnitude of \( 10^{6} \) basal epithelial cells fitting in the human cornea.
1.3 A.3 Rat and Rabbit
To demonstrate variability across other species, we note that rat and rabbit corneas have average diameters of \(5.5 \,\upmu \hbox {m}\) (Cabrera et al. 1999) and \(14.375 \,\upmu \hbox {m}\) (Tsonis 2011) respectively. Straightforward calculations show that the circumferences will be \(17{,}270 \,\upmu \hbox {m}\) and \(45{,}138\,\upmu \hbox {m}\) respectively. Making the same assumptions as earlier, this would allow for a total of 1727 and 4513 stem cells and, if again approximately 1 / 4 are active, \(\sim 450\) and \(\sim 1200\) active stem cells for rat and rabbit respectively. Calculating an estimate for the total number of cells that can fit into the basal epithelium yields a magnitude \(\sim 10^{5} \) for rat and \(\sim 10^{6} \) for rabbit, the former the same magnitude as the mouse and the latter similar to the human eye.
For a rabbit corneal epithelium, experimental data on TAC doubling time suggests once every 18 h (3 / 4) (Castro-Muñozledo 1994). We are lacking such data for the rat eye. Nevertheless, the parameter spaces provided throughout the paper can give a rough estimate of the TAC generations required for the epithelium maintenance for each of rat and rabbit eye.
Appendix B Derivation of matrices included in Lyapunov equation
1.1 B.1 Jacobian matrix
The Jacobian matrix J can be derived from the stochastic mean system (5)–(7) obtained in Sect. 2.3. Matrix J of our n-ODEs system for the stochastic means of TACs is:
Note that \( J_{ij}= \dfrac{\partial }{\partial \phi _{j}}(\partial _{t} \phi _{i})\) where \( \phi _{i}=N_{T_{i}} \) and \( \phi _{j}=N_{T_{j}} \) with \( j=1,\ldots ,n \).
1.2 B.2 Stoichiometric matrix
For the stoichiometric matrix we are only interested in the number of TACs at each reaction. Denoting the reactions as \( r_{k,l} \) with k the reacting population (i.e. \( k=0,1,\ldots ,n \), where \( k=0 \) corresponds to the \( SC_{a} \) division to \( TAC_{1} \) and \( k=i\) the \( TAC_{i} \) divisions) and the pathway indicator is l (hence \( l=1,2,3 \)). The reactions can be written as
where \(i=1,\ldots ,n\) denotes the number of TAC generation. The stoichiometric vector for \( TAC_{1} \) is [1 −1 −1 −1 0 \( \cdots \) 0], for \( TAC_{i} \) is [0 \( \cdots \) 0 2 1 −1 −1 −1 0 \( \cdots \) 0] and for \( TAC_{n} \) is [0 \( \cdots \) 0 2 1 −1]. As an example for the stoichiometric matrix \( \mathbf {S} \), let us assume that the total number of TAC generations is 3, then
Note that in the stoichiometric matrix for n TAC generations, the number of zero elements at the start of each row (excluding the first and last row which correspond to the first and last TAC generation respectively) will be \( N_{0}=3(i-1)+2 \) with \( i=2,\ldots ,n-1 \). Hence, the position of the first non-zero element in each row (\( i=2,\ldots ,n-1 \) ) follows the sequence \( \sum _{i=2}^{n-1}3(i-1) \).
1.3 B.3 Vector of macroscopic rates
To find the vector of macroscopic rates  we recall the reactions 31-35 listed in Appendix 1 with corresponding rates:
we recall the reactions 31-35 listed in Appendix 1 with corresponding rates:
Hence, the vector  for our system is
for our system is

1.4 B.4 Diffusion matrix
For the elements of the diffusion matrix, as already discussed in the text, we used
inside the matlab code, with \(\mathbf {F} \), \( \mathbf {S} \) and \(\mathbf {S^{T}}\) determined as above.
Rights and permissions
About this article
Cite this article
Moraki, E., Grima, R. & Painter, K.J. A stochastic model of corneal epithelium maintenance and recovery following perturbation. J. Math. Biol. 78, 1245–1276 (2019). https://doi.org/10.1007/s00285-018-1308-9
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00285-018-1308-9