Abstract
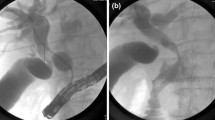
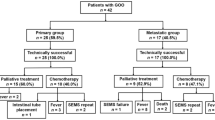
Many patients with malignant gastroduodenal obstruction have an unresectable primary lesion and distant metastases, which may prompt palliative management to allow the patient to eat and to improve the quality of life. Intraluminal metallic stent implantation (MSI) under fluoroscopic guidance has been reported to be an effective option for symptomatic relief in these patients, with a good safety record. An alternative, dual interventional therapy (DIT), has been used during the last decade, in which prosthesis insertion is followed by intra-arterial chemotherapy via the tumor-feeding arteries. The aim of this study was to compare success rates, complication rates, and survival time between MSI and DIT in patients who presented with gastroduodenal obstruction from advanced upper gastrointestinal tract cancer. All consecutive patients with malignant gastroduodenal obstruction seen at our center between October 2002 and August 2007 were retrospectively studied. Patients were treated palliatively by either MSI or DIT by the patient’s or the next of kin’s decision. Outcomes included technical and clinical success, complication rates, and survival. Of the 164 patients with malignant gastric and duodenal outlet obstructions, 80 (49%) underwent stent insertion as the primary therapy, while the remaining 84 (51%) received DIT. Clinical characteristics were similar between the two groups. In the MSI cohort initial stent implantation was successful in 73 patients (91%), two stents were used in 5 patients, and delayed additional stent insertion for stent obstruction related to tumor overgrowth was required in 3 patients during follow-up. In the DIT cohort the technical success rate was 94%, 3 patients required two stents, and stent obstruction occurred in 2 patients after initial stent placement. Early postprocedural clinical success, indicated by average dysphagia score, improved significantly in both groups: MSI group, from 4.56 to 1.51 (P < 0.01); and DIT group, from 4.38 to 1.48 (p < 0.01). There were no short-term complications. Late complications including hematemesis (n = 3), migration (n = 12), and stent occlusion due to tumor overgrowth (n = 5) were evenly distributed between the groups. In the DIT group chemotherapy-induced neutropenia and transient renal dysfunction were detected in six patients, which improved after symptomatic management. Mean survival time after the procedure was 5.9 and 11.1 months for MSI and DIT, respectively (P < 0.001). In conclusion, both MSI and DIT offer effective palliation for malignant gastroduodenal obstruction, but DIT appears to offer superior survival over MSI alone. Ideally, a prospective randomized trial comparing these two techniques should be carried out to validate this result.




Similar content being viewed by others
References
Weaver DW, Wiencek RG, Bouwman DL et al (1987) Gastrojejunostomy: is it helpful for patients with pancreatic cancer? Surgery 102:608–613
van Wagensveld BA, Coene PP, van Gulik TM et al (1997) Outcome of palliative biliary and gastric bypass surgery for pancreatic head carcinoma in 126 patients. Br J Surg 84:1402–1406
Lillemoe KD, Cameron JL, Hardacre JM et al (1999) Is prophylactic gastrojejunostomy indicated for unresectable periampullary cancer? A prospective randomized trial. Ann Surg 230:322–328
Keymling M, Wagner HJ, Vakil N et al (1993) Relief of malignant duodenal obstruction by percutaneous insertion of a metal stent. Gastrointest Endosc 39:439–441
Song HY, Yang DH, Kuh JH et al (1993) Obstructing cancer of the gastric antrum: palliative treatment with covered metallic stents. Radiology 187:357–358
Jung GS, Song HY, Kang SG et al (2000) Malignant gastroduodenal obstuctions: treatment by means of a covered expandable metallic stent-initial experience. Radiology 216:758–763
Lopera JE, Alvarez O, Castano R et al (2001) Initial experience with Song’s covered duodenal stent in the treatment of malignant gastroduodenal obstruction. J Vasc Interv Radiol 12:1297–1303
Nevitt AW, Vida F, Kozarek RA et al (1998) Expandable metallic prostheses for malignant obstructions of gastric outlet and proximal small bowel. Gastrointest Endosc 47:271–276
Razzaq R, Laasch HU, England R et al (2001) Expandable metal stents for the palliation of malignant gastroduodenal obstruction. Cardiovasc Intervent Radiol 24:313–318
Lopera JE, Brazzini A, Gonzales A et al (2004) Gastroduodenal stent placement: current status. Radiographics 24:1561–1573
Bessoud B, de Baere T, Denys A et al (2005) Malignant gastroduodenal obstruction: palliation with self-expanding metallic stents. J Vasc Interv Radiol 16:247–253
Stawowy M, Kruse A, Mortensen FV et al (2007) Endoscopic stenting for malignant gastric outlet obstruction. Surg Laparosc Endosc Percutan Tech 17:5–9
Lowe AS, Beckett CG, Jowett S et al (2007) Self-expandable metal stent placement for the palliation of malignant gastroduodenal obstruction: experience in a large, single, UK centre. Clin Radiol 62:738–744
Jung GS, Song HY, Seo TS et al (2002) Malignant gastric outlet obstructions: treatment by means of coaxial placement of uncovered and covered expandable nitinol stents. J Vasc Interv Radiol 13:274–283
Song HY, Shin JH, Yoon CJ et al (2004) A dual expandable nitinol stent: experience in 102 patients with malignant gastroduodenal strictures. J Vasc Interv Radiol 15:1443–1449
Zhang CW, Zou SC, Shi D et al (2004) Clinical significance of preoperative regional intra-arterial infusion chemotherapy for advanced gastric cancer. World J Gastroenral 10:3070–3072
Iida T, Hirata N, Hirakawa M et al (2003) Preoperative intraartirial infusion chemotherapy for advanced gastric cancer—a retrospective review of four cases. Radiat Med 21:172–177
Kitamura M, Arai K, Iwasaki Y (1996) Arterial infusion chemotherapy for advanced gastric cancer by sequential MTX/5-FU. Gan To Kagaku Ryoho 23:1464–1466
Tokairin Y, Nagahama T, Maruyama M (2002) A case of pyloric or antral malignant stenosis treated with arterial infusion chemotherapy and palliative therapy—self-expandable metal stents through gastrostomy. Gan To Kagaku Ryoho 29(12):2395–2398
Acknowledgments
We thank S. O. Trerotola, M.D., University of Pennsylvania Medical Center, Philadelphia, for editorial assistance in checking and revising the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, Z., Chen, K., Gong, J. et al. Combined Arterial Infusion and Stent Implantation Compared with Metal Stent Alone in Treatment of Malignant Gastroduodenal Obstruction. Cardiovasc Intervent Radiol 32, 1011–1018 (2009). https://doi.org/10.1007/s00270-009-9674-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-009-9674-8