Abstract
Objective
The purpose of this study was to investigate the differences in facial profile development between unoperated adult cleft palate (UACP) patients and normal controls and to analyse the reasons for the differences.
Materials and Methods
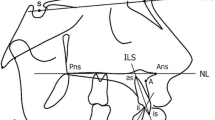
A total of 50 individuals with a unilateral cleft palate and 20 normal controls were selected to undergo angular measurement of their facial profiles. Data with significant differences between the two groups were analysed.
Results
Seven angle measurements of the facial profile showed that the mid-facial protrusion of the UACP patients had no significant differences from the control group (p > 0.05). But their angle of the medium face (N′–Trg–Sn) was significantly lower than the non-cleft controls (p < 0.05), suggesting a worse vertical development of the middle face. A significantly larger nasal tip angle (Cm–Sn/N′–Prn) for UACP patients suggested they had a rounder and blunter nasal tip (p < 0.05). The soft tissue facial angle and chin–lip angle of UACP patients had significant differences from non-cleft controls (p < 0.05), but the head position angle (Sn–Sm–THP) had no significant difference between two groups (p > 0.05), which suggested a steep mandibular plane for UACP patients but without severe retraction of the chin.
Conclusion
The development of facial protrusions in UACP patients is similar to that in normal adults, but the vertical development in the middle face is insufficient. Such hypoplasia may be related to the intrinsic deficiency of the maxilla. There is a tendency for flat nasal growth and insufficient development of the chin in UACP patients.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.




Similar content being viewed by others
Change history
23 July 2019
Due to errors introduced during the production process, Tables were published incorrectly in the original publication of this article. The correct tables are given here.
References
Semb G (1991) A study of facial growth in patients with unilateral cleft lip and palate treated by the Oslo CLP Team. Cleft Palate J 28(1):22–24
Petersonfalzone SJ (1996) The relationship between timing of cleft palate surgery and speech outcome: what have we learned, and where do we stand in the 1990s? Semin Orthod 2(3):185–189
Randall P, LaRossa DD et al (1983) Cleft palate closure at 3 to 7 months of age: a preliminary report. Plast Reconstr Surg 71(5):624–628
Kaplan I, Ben-Bassat M, Taube E et al (1982) Ten-year follow-up of simultaneous repair of cleft lip and palate in infancy. Ann Plast Surg 8(3):227–228
Friede H, Enemark H (2001) Long-term evidence for favorable midfacial growth after delayed hard palate repair in UCLP patients. Cleft Palate Craniofac J Off Publ Am Cleft Palate-Craniofac Assoc 38(4):323–326
Schweckendiek W (1978) Primary veloplasty: long-term results without maxillary deformity. A twenty-five year report. Cleft Palate J 15(3):268–274
Bardach J, Morris HL, Olin WH (1984) Late results of primary veloplasty: the Marburg project. Plast Reconstr Surg 73(2):207–218
Rohrich RJ, Rowsell AR, Johns DF et al (1996) Timing of hard palatal closure: a critical long-term analysis. Plast Reconstr Surg 98(2):236–246
Figueroa AA, Polley JW (1999) Management of severe cleft maxillary deficiency with distraction osteogenesis: procedure and results. Am J Orthod Dentofac Orthoped 115(1):1–12
Oberoi S, Hoffman WY, Chigurupati R et al (2012) Frequency of surgical correction for maxillary hypoplasia in cleft lip and palate. J Craniofac Surg 23(6):1665–1667
Olate S, Zaror C, Blythe JN et al (2016) A systematic review of soft-to-hard tissue ratios in orthognathic surgery. Part III: double jaw surgery procedures. J Cranio-Maxillofac Surg 44(10):1599–1606
Henderson JL, Larrabee WF, Krieger BD (2005) Photographic standards for facial plastic surgery. Arch Facial Plast Surg 7(5):331–339
Lee UL, Cho JB, Choung PH (2013) Simultaneous premaxillary repositioning and cheiloplasty in adult patients with unrepaired bilateral cleft lip and palate. Cleft Palate-Craniofac J 50(2):231–236
Nyberg DA, Hegge FN, Kramer D et al (1993) Premaxillary protrusion: a sonographic clue to bilateral cleft lip and palate. J Ultrasound Med 12(6):331–335
Bitter Klaus (1992) Latham’s appliance for presurgical repositioning of the protruded premaxilla in bilateral cleft lip and palate. J Cranio-Maxillofac Surg 20(3):99–110
Bardach J, Kelly KM (1990) Does interference with mucoperiosteum and palatal bone affect craniofacial growth? An experimental study in beagles. Plast Reconstr Surg 86(6):1101–1102
Wang XX, Wang X, Yi B et al (2005) Internal midface distraction in correction of severe maxillary hypoplasia secondary to cleft lip and palate. Plast Reconstr Surg 116(1):51–60
Fariña R, Diaz A et al (2018) Treatment of maxillary hypoplasia in cleft lip and palate: segmental distraction osteogenesis with hyrax device. J Craniofac Surg 29(2):1–4
Capelozza L, Taniguchi SM, Silva OGD (1993) Craniofacial morphology of adult unoperated complete unilateral cleft lip and palate patients. Cleft Palate-Craniofac J 30(4):376–381
Liao YF, Mars M (2005) Long-term effects of clefts on craniofacial morphology in patients with unilateral cleft lip and palate. Cleft Palate-Craniofac J 42(6):601–609
Shetye PR, Evans CA (2006) Midfacial morphology in adult unoperated complete unilateral cleft lip and palate patients. Angle Orthod 76(5):810–817
Cao C, Xu X, Shi B et al (2017) Is cleft severity correlated with intrinsic growth pattern? Observation from unoperated adult patients with submucous cleft palate. J Craniofac Surg 28:1451–1455
Ye B, Wu Y, Zhou Y et al (2015) A comparative cephalometric study for adult operated cleft palate and unoperated cleft palate patients. J Craniomaxillofac Surg 43(7):1218–1223
Capelozza FL, Normando AD, Og DSF (1996) Isolated influences of lip and palate surgery on facial growth: comparison of operated and unoperated male adults with UCLP. Cleft Palate-Craniofac J Off Publ Am Cleft Palate-Craniofac Assoc 33(1):51–57
Ross RB (1987) Treatment variables affecting facial growth in complete unilateral cleft lip and palate. Cleft Palate J 24(1):75–77
Liao YF, Mars M (2005) Long-term effects of lip repair on dentofacial morphology in patients with unilateral cleft lip and palate. Cleft Palate-Craniofac J Off Publ Am Cleft Palate-Craniofac Assoc 42(5):526–530
Isiekwe MC, Sowemimo GOA (1984) Cephalometric findings in a normal nigerian population sample and adult nigerians with unrepaired clefts. Cleft Palate J 21(4):323–328
Smahel Z, Polivková H, Skvarilová B et al (1992) Configuration of facial profile in adults with cleft lip with or without cleft palate. Acta Chir Plast 34(4):190–203
Malek FA, Miritz KU, Fanghnel J et al (2003) Sex-related differences in procarbazine-induced cleft palate and microgenia and the anti-teratogenic effect of prenatal folic acid supplementation in rats. Ann Anat 185(5):465–470
Fernández-Riveiro P, Smyth-Chamosa E, Suárez-Quintanilla D et al (2003) Angular photogrammetric analysis of the soft tissue facial profile. Eur J Orthod 25:393–399
Katzel EB, Basile P, Koltz PF et al (2009) Current surgical practices in cleft care: cleft palate repair techniques and postoperative care. Plast Reconstr Surg 124(3):899–906
Zhang Z, Stein M, Mercer N et al (2017) Post-operative outcomes after cleft palate repair in syndromic and non-syndromic children: a systematic review protocol. Syst Rev 6(1):52
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare that we have no conflict of interest.
Ethical Approval
The study protocol was approved by the Internal Review Board of the Department of the College of Stomatology at Guangxi Medical University.
Informed Consent
All patients signed informed consent forms.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lin, X., Li, Hy., Xie, Qt. et al. The Soft Tissue Angular Analysis of Facial Profile in Unoperated Adult Patients with Unilateral Cleft Palate. Aesth Plast Surg 43, 982–992 (2019). https://doi.org/10.1007/s00266-019-01371-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-019-01371-z