Abstract
Background
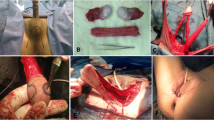
The inverted peno-scrotal flap method is considered the standard method of vaginoplasty in male-to-female genital reassignment surgery. Though with numerous advantages, the method has its limitations regarding skin texture, lack of inherent lubrication, and that the tissues for creating the labia depend on the amount of tissues remaining after vaginoplasty. Our purpose was to describe the procedure and outcome of vaginoplasty applying a new technique: autologous buccal micro-mucosa free graft combined with posterior scrotal flap transfer, which could solve some of the problems the previous methods had.
Methods
Nine male-to-female transsexual patients received our new method of vaginoplasty from July 2010–October 2015. We described the details of the surgical procedure and evaluated the long-term anatomical and functional outcomes.
Results
In a mean clinical follow-up period of 25.3 months and phone interview follow-up of 50.3 months, we observed that the neovaginas in the nine cases were all of sufficient volume, lined with mucosa, with natural mucosal discharge. The oral donor sites resulted in no visible scars or malfunction. Eight patients experienced uneventful postoperative periods, while one patient suffered from scrotal flap prolapse. All the patients were sexually active and reported sexual satisfaction, with no need of lubrication.
Conclusion
The reported technique achieves the outcomes of creating a neovagina of sufficient volume, without serious stenosis in long-term follow-up. The neovagina is lined with mucosa and has appropriate lubrication as well as good sexual sensation. The reported method is easy and economical to perform and retains enough tissues for vulvoplasty to achieve a superior cosmetic appearance, with rare risk of complications and donor area malfunction. Additionally, this technique is feasible and advantageous to the patients who have insufficient peno-scrotal skin for neovaginal lining as well as those with unfavorable previous vaginoplasty. All of these indicate that this technique is a promising option for vaginoplasty in male-to-female transsexual surgery.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.










Similar content being viewed by others
References
Leclere FM, Casoli V, Baudet J, Weigert R (2015) Description of the Baudet surgical technique and introduction of a systematic method for training surgeons to perform male-to-female sex reassignment surgery. Aesthet Plast Surg 39:927–934
Kanhai RC (2016) Sensate vagina pedicled-spot for male-to-female transsexuals: the experience in the first 50 patients. Aesthet Plast Surg 40:284–287
Gennaro Selvaggi PC, De Cuypere Griet et al (2005) Gender identity disorder: general overview and surgical treatment for vaginoplasty in male-to-female transsexuals. Plast Reconstr Surg 116:135e–145e
Selvaggi G, Bellringer J (2011) Gender reassignment surgery: an overview. Nat Rev Urol 8:274–282
Raigosa M, Avvedimento S, Yoon TS, Cruz-Gimeno J, Rodriguez G, Fontdevila J (2015) Male-to-female genital reassignment surgery: a retrospective review of surgical technique and complications in 60 patients. J Sex Med 12:1837–1845
Fang RHCC, Ma S (1992) A new methods for clitoroplasty in male-to-female sex reassignment surgery. Plast Reconstr Surg 89:679–682
Puppo V (2011) Embryology and anatomy of the vulva: the female orgasm and women’s sexual health. Eur J Obstet Gynecol Reprod Biol 154:3–8
Zhang CY, Cui HX (2002) The female reproductive system. In: Zheng SJ, Huang Y, Wu JB (eds) The anotomy measurements of Chinese People. People’s Medical Publishing House, Beijing, pp 206–227
Cao Y, Li Q, Zhou C, Li F, Li S, Zhou Y (2015) Measurements of female genital appearance in Chinese adults seeking genital cosmetic surgery: a preliminary report from a gynecological center. Int Urogynecol J 26:729–735
Taylor GI, Townsend P, Corlett R (1979) Superiority of the deep circumflex iliac vessels as the supply for free groin flaps. Plast Reconstr Surg 64:745–759
Millard DR Jr (1986) Tissue losses should be replaced in kind. In: Millard DR Jr (ed) Principalization of plastic surgery. Lippincott Williams & Wilkins Inc., Boston, pp 191–228
Lin WC (2003) Use of autologous buccal mucosa for vaginoplasty: a study of eight cases. Hum Reprod 18:604–607
Yesim Ozgenel G, Ozcan M (2003) Neovaginal construction with buccal mucosal grafts. Plast Reconstr Surg 111:2250–2254
Zhao M, Li P, Li S, Li Q (2009) Use of autologous micro-mucosa graft for vaginoplasty in vaginal agenesis. Ann Plast Surg 63:645–649
Li FY, Xu YS, Zhou CD, Zhou Y, Li SK, Li Q (2014) Long-term outcomes of vaginoplasty with autologous buccal micro-mucosa. Obstet Gynecol 123:951–956
Wangjiraniran B, Selvaggi G, Chokrungvaranont P, Jindarak S, Khobunsongserm S, Tiewtranon P (2015) Male-to-female vaginoplasty: Preecha’s surgical technique. J Plast Surg Hand Surg 49:153–159
Dekker JJ, Hage JJ, Karim RB, Bloemena E (2007) Do histologic changes in the skin-lined neovagina of male-to-female transsexuals really occur? Ann Plast Surg 59:546–549
Morrison SD, Satterwhite T, Grant DW, Kirby J, Laub DR Sr, VanMaasdam J (2015) Long-term outcomes of rectosigmoid neocolporrhaphy in male-to-female gender reassignment surgery. Plast Reconstr Surg 136:386–394
Guerrissi JO, Belmonte J (2004) Surgical treatment of dry eye syndrome: conjunctival graft of the minor salivary gland. Craniofac Surg 15:6–10
Cheung LKSN, Tideman H (1994) The epithelialization process of the temporalis myofascial flap in maxillary reconstruction. J Craniomaxillofac Surg 22:84
Zhang ML, Wang CY, Chang ZD, Cao DX, Han X (1986) Microskin grafting. II. Clinical report. Burns Incl Therm Inj 12:544–548
Mardovin WMS, Eppinger M, Finley RK (1992) Micrografts: the “super” expansion graft. J Burn Care Rehabil 13:556–559
Zhang ML, Chang ZD, Han X, Zhu M (1986) Microskin grafting. I animal experiments. Burns Incl Therm Inj 12:540–543
Lin SD, Lai CS, Chou CK, Tsai CW, Wu KF, Chang CW (1992) Microskin autograft with pigskin xenograft overlay: a preliminary report of studies on patients. Burns 18:321–325
Dessy LA, Mazzocchi M, Corrias F, Ceccarelli S, Marchese C, Scuderi N (2014) The use of cultured autologous oral epithelial cells for vaginoplasty in male-to-female transsexuals: a feasibility, safety, and advantageousness clinical pilot study. Plast Reconstr Surg 133:158–161
Grafenberg E (1950) The role of urethra in female orgasm. Int J Sexol 3:145–148
Funding
The study was funded by “PUMC Youth Fund” and “the Fundamental Research Funds for the Central Universities” (Grant Number 3332015059).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Wei, SY., Li, FY., Li, Q. et al. Autologous Buccal Micro-Mucosa Free Graft combined with Posterior Scrotal Flap Transfer for Vaginoplasty in Male-To-Female Transsexuals: A Pilot Study. Aesth Plast Surg 42, 188–196 (2018). https://doi.org/10.1007/s00266-017-0977-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-017-0977-x