Abstract
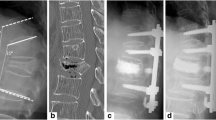
Delayed vertebral collapse after osteoporotic spinal fractures may cause progressive kyphosis, neurological deficits, and chronic back pain. We treated 14 consecutive patients with posterolateral decompression and posterior reconstruction and followed them over a period ranging from 24 to 54 months. The mean age was 67 (range: 62–72) years and the fracture level was T12 and L1. Seven patients were graded as Frankel stage C and seven as stage D. The mean segmental kyphotic angle was 22.6° (7–29°) preoperatively, 4.4° (1–6°) postoperatively, and 6.8° (2–15°) at the final follow-up. The pain score on a visual analogue scale improved from 9.5 preoperatively to 2.7 postoperatively, and the neurological status improved in all patients. Bone fusion was present 9 months after operation. Of four surgical complications, two were dural tears, one a superficial infection, and there was one death due to an acute adrenal insufficiency. Posterolateral decompression with posterior reconstruction is a useful treatment for patients with delayed osteoporotic vertebral collapse.
Résumé
Le collapsus vertébral secondaire, après une fracture vertébrale ostéoporotique, peut créer une cyphose progressive, un déficit neurologique et des lombalgies chroniques. Nous avons traité 14 malades consécutifs par décompression postérolaterale et reconstruction postérieure et les avons suivis de 24 à 54 mois. L'âge moyen était 67 (62–72) années. Le niveau de la fracture était T12 et L1. Sept malades ont été notés comme Frankel stade C et sept comme stade D. L'angle cyphotique segmentaire moyen était 22.6° (7–29°) avant l'opération, 4.4° (1–6°) postopératoire, et 6.8° (2–15°) au dernier examen. Le score de la douleur sur une échelle analogue visuelle s'est amélioré de 9.5 en préopératoire à 2.7 en postopératoire. Le statut neurologique a été amélioré chez tous les malades. La fusion osseuse était visible 9 mois après la chirurgie. Il y avait quatre complications chirurgicales, deux brèches duremériennes, une infection superficielle et un décés dû à une insuffisance surrénale aiguë. La décompression posterolateral avec reconstruction postérieure est une bonne option de traitement chez les malades avec collapsus vertébral différé.


Similar content being viewed by others
References
Arciero RA, Leung KY, Pierce JH (1989) Spontaneous unstable burst fracture of the thoracolumbar spine in osteoporosis. Spine 14: 114–117
Brower AC, Downey EF Jr (1981) Kummel disease: Report of a case with serial radiographs. Radiology 1341: 363–364
Chou LH, Knight RQ (1997) Idiopathic avascular necrosis of a vertebral body. Spine 22: 1928–1932
Hasegawa K, Homma T, Uchiyama S, Takahashi H (1988) Vertebral pseudarthrosis in the osteoporotic spine. Spine 23: 2201–2206
Hermann G, Goldblatt J, Desnick RJ (1984) Case reports, Kummell disease: delayed collapse of the traumatized spine in a patient with Gaucher Type 1 disease. Br J Radiol 57: 833–835
Hu SS (1997) Internal fixation in the osteoporotic spine. Spine 22: 43–48
Kaneda K, Asano S, Hashimoto T, Satoh S, Fujiya M (1992) The treatment of osteoporotic-posttraumatic vertebral collapse using the Kaneda device and bioactive ceramic vertebral prosthesis. Spine 17: 295–303
Kempinsky WH (1958) Osteoporotic kyphosis with paraplegia. Neurology 8: 181–186
Kim SW, Chung YK (2001) The surgical reconstruction of osteoporotic vertebral fractures. J Kor Soc Fracture 14: 30–36
Maldague BE, Noel HM, Malgehm JJ (1978) The intravertebral vacuum cleft. Radiology 129: 23–29
Malghem J, Maldague B, Labaisse MA, Dooms G, Duprez T, Devogelaer JP, Vande Berg B (1993) Intravertebral vacuum cleft: changes in content after supine position. Radiology 187: 483–487
Parfitt AM, Duncan H (1982) Metabolic bone disease affecting the spine. In: Rothman RH , Simone FA (eds) The spine, vol 2, 2nd edn. Saunders, Philadelphia, pp 828–830
Salomon C, Chopin D, Benoist M (1988) Spinal cord compression: An exceptional complication of spinal osteoporosis. Spine 13: 222–224
Shikata J, Yamamuro T, Ida H, Shimizu K, Yoshikawa J (1990) Surgical treatment for paraplegia resulting from vertebral fractures in senile osteoporosis. Spine 5: 485–489
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, KT., Suk, KS., Kim, JM. et al. Delayed vertebral collapse with neurological deficits secondary to osteoporosis. International Orthopaedics (SICOT) 27, 65–69 (2003). https://doi.org/10.1007/s00264-002-0418-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-002-0418-5