Abstract
Purpose
To develop and test radiomics models based on manually corrected or automatically gained masks on ADC maps for pelvic lymph node metastasis (PLNM) prediction in patients with prostate cancer (PCa).
Methods
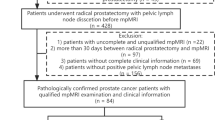
A primary cohort of 474 patients with PCa who underwent prostate mpMRI were retrospectively enrolled for PLNM prediction between January 2017 and January 2020. They were then randomly split into training/validation (n = 332) and test (n = 142) groups for model development and internal testing. Four radiomics models were developed using four masks (manually corrected/automatic prostate gland and PCa lesion segmentation) based on the ADC maps using the primary cohort. Another cohort of 128 patients who underwent radical prostatectomy (RP) with extended pelvic lymph node dissection (ePLND) for PCa was used as the testing cohort between February 2020 and October 2021. The performance of the models was evaluated in terms of discrimination and clinical usefulness using the area under the curve (AUC) and decision curve analysis (DCA). The optimal radiomics model was further compared with Memorial Sloan Kettering Cancer Center (MSKCC) and Briganti 2017 nomograms, and PI-RADS assessment.
Results
17 (13.28%) Patients with PLNM were included in the testing cohort. The radiomics model based on the mask of automatically segmented prostate obtained the highest AUC among the four radiomics models (0.73 vs. 0.63 vs. 0.70 vs. 0.56). Briganti 2017, MSKCC nomograms, and PI-RADS assessment-yielded AUCs of 0.69, 0.71, and 0.70, respectively, and no significant differences were found compared with the optimal radiomics model (P = 0.605–0.955).
Conclusion
The radiomics model based on the mask of automatically segmented prostate offers a non-invasive method to predict PLNM for patients with PCa. It shows comparable accuracy to the current MKSCC and Briganti nomograms.





Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
The codes used for the model development are available from the corresponding author on reasonable request.
References
Preisser F, van den Bergh RCN, Gandaglia G, et al. Effect of Extended Pelvic Lymph Node Dissection on Oncologic Outcomes in Patients with D'Amico Intermediate and High Risk Prostate Cancer Treated with Radical Prostatectomy: A Multi-institutional Study. J Urol. 2020, 203(2):338–43. doi: https://doi.org/10.1097/ju.0000000000000504
Bianchi L, Gandaglia G, Fossati N, et al. Pelvic lymph node dissection in prostate cancer: indications, extent and tailored approaches. Urologia. 2017,84(1):9–19. doi: https://doi.org/10.5301/uro.5000139
Van Huele A, Poelaert F, Fonteyne V, et al. Pelvic lymph node dissection in prostate cancer staging: evaluation of morbidity and oncological outcomes. Acta Chir Belg. 2019, 119(2):103–9. doi: https://doi.org/10.1080/00015458.2018.1470294
Briganti A, Blute ML, Eastham JH, et al. Pelvic lymph node dissection in prostate cancer. Eur Urol. 2009, 55(6):1251–65. doi: https://doi.org/10.1016/j.eururo.2009.03.012
Briganti A, Larcher A, Abdollah F, et al. Updated nomogram predicting lymph node invasion in patients with prostate cancer undergoing extended pelvic lymph node dissection: the essential importance of percentage of positive cores. Eur Urol. 2012, 61(3):480–7. doi: https://doi.org/10.1016/j.eururo.2011.10.044
Gandaglia G, Fossati N, Zaffuto E, et al. Development and Internal Validation of a Novel Model to Identify the Candidates for Extended Pelvic Lymph Node Dissection in Prostate Cancer. Eur Urol. 2017, 72(4):632–40. doi: https://doi.org/10.1016/j.eururo.2017.03.049
Gandaglia G, Ploussard G, Valerio M, et al. A Novel Nomogram to Identify Candidates for Extended Pelvic Lymph Node Dissection Among Patients with Clinically Localized Prostate Cancer Diagnosed with Magnetic Resonance Imaging-targeted and Systematic Biopsies. Eur Urol. 2019, 75(3):506–14. doi: https://doi.org/10.1016/j.eururo.2018.10.012
Kim D, Hanna MG, Vanderbilt C, et al. Pathology Informatics Education during the COVID-19 Pandemic at Memorial Sloan Kettering Cancer Center (MSKCC). Acta Med Acad. 2021, 50(1):136–42. doi: https://doi.org/10.5644/ama2006-124.331
Stabile A, Dell'Oglio P, Gandaglia G, et al. Not All Multiparametric Magnetic Resonance Imaging-targeted Biopsies are Equal: The Impact of the Type of Approach and Operator Expertise on the Detection of Clinically Significant Prostate Cancer. Eur Urol Oncol. 2018, 1(2):120–8. doi: https://doi.org/10.1016/j.euo.2018.02.002
Kasabwala K, Patel N, Cricco-Lizza E, et al. The Learning Curve for Magnetic Resonance Imaging/Ultrasound Fusion-Guided Prostate Biopsy. Eur Urol Oncol. 2019, 2(2):135–40. doi: https://doi.org/10.1016/j.euo.2018.07.005
Sun Y, Reynolds HM, Parameswaran B, et al. Multiparametric MRI and radiomics in prostate cancer: a review. Australas Phys Eng Sci Med. 2019, 42(1):3–25. doi: https://doi.org/10.1007/s13246-019-00730-z
Rogers W, Thulasi Seetha S, Refaee TAG, et al. Radiomics: from qualitative to quantitative imaging. Br J Radiol. 2020, 93(1108):20190948. doi: https://doi.org/10.1259/bjr.20190948
Hou Y, Bao J, Song Y, et al. Integration of clinicopathologic identification and deep transferrable image feature representation improves predictions of lymph node metastasis in prostate cancer. EBioMedicine. 2021, 68:103395. doi: https://doi.org/10.1016/j.ebiom.2021.103395
Schelb P, Kohl S, Radtke JP, et al. Classification of Cancer at Prostate MRI: Deep Learning versus Clinical PI-RADS Assessment. Radiology. 2019, 293(3):607–17. doi: https://doi.org/10.1148/radiol.2019190938
Laukamp KR, Thiele F, Shakirin G, et al. Fully automated detection and segmentation of meningiomas using deep learning on routine multiparametric MRI. Eur Radiol. 2019, 29(1):124–32. doi: https://doi.org/10.1007/s00330-018-5595-8
Barentsz JO, Richenberg J, Clements R, et al. ESUR prostate MR guidelines 2012. Eur Radiol. 2012,22(4):746–57. doi: https://doi.org/10.1007/s00330-011-2377-y
Anttinen M, Ettala O, Malaspina S, et al. A Prospective Comparison of (18)F-Prostate-Specific Membrane Antigen-1007 Positron Emission Tomography Computed Tomography, Whole-body 1.5 T Magnetic Resonance Imaging with Diffusion-Weighted Imaging, and Single-Photon Emission Computed Tomography/Computed Tomography with Traditional Imaging in Primary Distant Metastasis Staging of Prostate Cancer (PROSTAGE). Eur Urol Oncol. 2021, 4(4):635–44. doi: https://doi.org/10.1016/j.euo.2020.06.012
Van Damme J, Tombal B, Collette L, et al. Comparison of (68)Ga-Prostate Specific Membrane Antigen (PSMA) Positron Emission Tomography Computed Tomography (PET-CT) and Whole-Body Magnetic Resonance Imaging (WB-MRI) with Diffusion Sequences (DWI) in the Staging of Advanced Prostate Cancer. Cancers (Basel). 2021, 13(21). doi: https://doi.org/10.3390/cancers13215286
Zhu Y, Wei R, Gao G, et al. Fully automatic segmentation on prostate MR images based on cascaded fully convolution network. J Magn Reson Imaging. 2019, 49(4):1149–56. doi: https://doi.org/10.1002/jmri.26337
Zhu L, Gao G, Liu Y, et al. Feasibility of integrating computer-aided diagnosis with structured reports of prostate multiparametric MRI. Clin Imaging. 2020, 60(1):123–30. doi: https://doi.org/10.1016/j.clinimag.2019.12.010
Song Y, Zhang J, Zhang YD, et al. FeAture Explorer (FAE): A tool for developing and comparing radiomics models. PLoS ONE. 2020, 15(8):e0237587. doi: https://doi.org/10.1371/journal.pone.0237587
Turkbey B, Rosenkrantz AB, Haider MA, et al. Prostate Imaging Reporting and Data System Version 2.1: 2019 Update of Prostate Imaging Reporting and Data System Version 2. Eur Urol. 2019, 76(3):340–51. doi: https://doi.org/10.1016/j.eururo.2019.02.033
Mohler JL, Antonarakis ES, Armstrong AJ, et al. Prostate Cancer, Version 2.2019, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Cancer Netw. 2019, 17(5):479–505. doi: https://doi.org/10.6004/jnccn.2019.0023
Draulans C, Everaerts W, Isebaert S, et al. Development and External Validation of a Multiparametric Magnetic Resonance Imaging and International Society of Urological Pathology Based Add-On Prediction Tool to Identify Prostate Cancer Candidates for Pelvic Lymph Node Dissection. J Urol. 2020, 203(4):713–8. doi: https://doi.org/10.1097/ju.0000000000000652
Brembilla G, Dell'Oglio P, Stabile A, et al. Preoperative multiparametric MRI of the prostate for the prediction of lymph node metastases in prostate cancer patients treated with extended pelvic lymph node dissection. Eur Radiol. 2018, 28(5):1969–76. doi: https://doi.org/10.1007/s00330-017-5229-6
Park SY, Shin SJ, Jung DC, et al. PI-RADS version 2: Preoperative role in the detection of normal-sized pelvic lymph node metastasis in prostate cancer. Eur J Radiol. 2017, 91:22–8. doi: https://doi.org/10.1016/j.ejrad.2017.03.009
Bourbonne V, Vallières M, Lucia F, et al. MRI-Derived Radiomics to Guide Post-Operative Management for High-Risk Prostate Cancer. Front Oncol. 2019, 9:807. doi: https://doi.org/10.3389/fonc.2019.00807
Wibmer A, Hricak H, Gondo T, et al. Haralick texture analysis of prostate MRI: utility for differentiating non-cancerous prostate from prostate cancer and differentiating prostate cancers with different Gleason scores. Eur Radiol. 2015, 25(10):2840–50. doi: https://doi.org/10.1007/s00330-015-3701-8
Bourbonne V, Jaouen V, Nguyen TA, et al. Development of a Radiomic-Based Model Predicting Lymph Node Involvement in Prostate Cancer Patients. Cancers (Basel). 2021, 13(22). doi: https://doi.org/10.3390/cancers13225672
Lohmann P, Bousabarah K, Hoevels M, et al. Radiomics in radiation oncology—basics, methods, and limitations. Strahlenther Onkol. 2020, 196(10):848–55. doi: https://doi.org/10.1007/s00066-020-01663-3
Van Poppel H, Roobol MJ, Chapple CR, et al. Prostate-Specific Antigen Testing as Part of a Risk-Adapted Early Detection Strategy for Prostate Cancer: European Association of Urology Position and Recommendations for 2021. Eur Urol. 2021, 80(6):703–11. doi: https://doi.org/10.1016/j.eururo.2021.07.024
Hou Y, Bao ML, Wu CJ, et al. A machine learning-assisted decision-support model to better identify patients with prostate cancer requiring an extended pelvic lymph node dissection. BJU Int. 2019, 124(6):972–83. doi: https://doi.org/10.1111/bju.14892
Fehr D, Veeraraghavan H, Wibmer A, et al. Automatic classification of prostate cancer Gleason scores from multiparametric magnetic resonance images. Proc Natl Acad Sci U S A. 2015, 112(46):E6265–73. doi: https://doi.org/10.1073/pnas.1505935112
Gandaglia G, Martini A, Ploussard G, et al. External Validation of the 2019 Briganti Nomogram for the Identification of Prostate Cancer Patients Who Should Be Considered for an Extended Pelvic Lymph Node Dissection. Eur Urol. 2020, 78(2):138–42. doi: https://doi.org/10.1016/j.eururo.2020.03.023
Shaish H, Kang SK, Rosenkrantz AB. The utility of quantitative ADC values for differentiating high-risk from low-risk prostate cancer: a systematic review and meta-analysis. Abdom Radiol (NY). 2017, 42(1):260–70. doi: https://doi.org/10.1007/s00261-016-0848-y
Funding
This study was supported by Capital’s Funds for Health Improvement and Research (2020-2-40710).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by XL and ZS. XL performed manual annotation under the supervision of XW. XW, YZ, and XZ performed data interpretation and statistical analysis. The first draft of the manuscript was written by XL and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Xiangpeng Wang and Yaofeng Zhang are from a medical technical corporation provided technical support for model development. The authors declare that they have no competing interests.
Ethical approval
This study was approved by the Local Institutional Ethical Committee.
Informed consent
The need for written informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, X., Wang, X., Zhang, Y. et al. Preoperative prediction of pelvic lymph nodes metastasis in prostate cancer using an ADC-based radiomics model: comparison with clinical nomograms and PI-RADS assessment. Abdom Radiol 47, 3327–3337 (2022). https://doi.org/10.1007/s00261-022-03583-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-022-03583-5