Abstract
Objective
To determine the frequency of elevated peak systolic proper hepatic artery velocity (HAV) in patients with acute cholangitis and to determine the diagnostic performance of this metric relative to existing criteria.
Methods
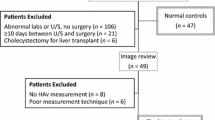
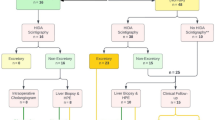
Between 9/2016 and 11/2017, 107 patients clinically suspected to have cholangitis were referred for an abdominal ultrasound. Of these, 56 patients had HAV measurements and were included in the final analysis. Clinical and imaging features, including HAV, HAV resistive index (RI), portal vein velocity (PVV), biliary dilation, and presence of an obstructive etiology were extracted. The diagnostic performance of HAV was compared to the existing available clinical criteria (Charcot’s triad and 2018 Tokyo Guidelines). Elevated HAV was defined as HAV > 100 cm/s. Presence of cholangitis was determined by the discharge summary following medical workup and admission or observation.
Results
32% had cholangitis while 68% did not. Average HAV for patients with cholangitis was 152 ± 54 cm/s versus 91 ± 44 cm/s for those without (p < 0.0001; t test). The HAV was elevated in 83% of patients with cholangitis. When considered in isolation, an elevated HAV had a high negative predictive value (90%), was more accurate (77%; 95% confidence interval 64–87%) than Charcot’s triad (73%; 60–83%), and had similar accuracy compared to 2018 Tokyo Guidelines (79%; 66–88%). Substitution of conventional imaging criteria with elevated HAV in the 2018 Tokyo Guidelines yielded the highest overall accuracy of 84% (72–92%).
Conclusion
HAV is elevated in the majority of patients with cholangitis. Substitution of an elevated HAV for conventional sonographic criteria is more accurate than existing clinical criteria in identifying patients with cholangitis.


Similar content being viewed by others
References
Hanau LH, Steigbigel NH. Acute (ascending) cholangitis. Infect Dis Clin North Am. 2000;14(3):521–546.
Abbas AK, Fausto N, Robbins SL. Robbins and Cotran pathologic basis of disease. Elsevier Saunders; 2005.
Huang T, Bass JA, Williams RD. The significance of biliary pressure in cholangitis. Arch Surg. 1969;98(5):629–632.
Clements WD, Parks R, Erwin P, Halliday MI, Barr J, Rowlands BJ. Role of the gut in the pathophysiology of extrahepatic biliary obstruction. Gut. 1996;39(4):587–593.
Sung JY, Shaffer EA, Olson ME, Leung JWC, Lam K, Costerton JW. Bacterial invasion of the biliary system by way of the portal-venous system. Hepatology. 1991;14(2):313–317.
Qureshi WA. Approach to the Patient Who Has Suspected Acute Bacterial Cholangitis. Gastroenterology Clinics of North America. 2006. p. 409–423. http://dx.doi.org/10.1016/j.gtc.2006.05.005.
Rahman SH, Larvin M, McMahon MJ, Thompson D. Clinical presentation and delayed treatment of cholangitis in older people. Dig Dis Sci. 2005;50(12):2207–2210.
Kimura Y, Takada T, Kawarada Y, et al. Definitions, pathophysiology, and epidemiology of acute cholangitis and cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007;14(1):15–26.
Csendes A, Diaz JC, Burdiles P, Maluenda F, Morales E. Risk factors and classification of acute suppurative cholangitis. Br J Surg. 1992;79(7):655–658.
Boey JH, Way LW. Acute cholangitis. Ann Surg. 1980;191(3):264–270.
Miura F, Okamoto K, Takada T, et al. Tokyo Guidelines 2018: initial management of acute biliary infection and flowchart for acute cholangitis. J Hepatobiliary Pancreat Sci. 2018;25(1):31–40.
Lai ECS, Mok FPT, Tan ESY, et al. Endoscopic Biliary Drainage for Severe Acute Cholangitis. New England Journal of Medicine. 1992. p. 1582–1586. https://doi.org/10.1056/nejm199206113262401.
Catalano OA, Sahani DV, Forcione DG, et al. Biliary infections: spectrum of imaging findings and management. Radiographics. 2009;29(7):2059–2080.
Lee JG. Diagnosis and management of acute cholangitis. Nature Reviews Gastroenterology & Hepatology. 2009. p. 533–541. https://doi.org/10.1038/nrgastro.2009.126.
Rumsey S, Winders J, MacCormick AD. Diagnostic accuracy of Charcot’s triad: a systematic review. ANZ J Surg. 2017;87(4):232–238.
Kiriyama S, Kozaka K, Takada T, et al. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25(1):17–30.
Park SM, Kim WS, Bae I-H, et al. Common bile duct dilatation after cholecystectomy: a one-year prospective study. J Korean Surg Soc. 2012;83(2):97–101.
Bachar GN, Cohen M, Belenky A, Atar E, Gideon S. Effect of aging on the adult extrahepatic bile duct: a sonographic study. J Ultrasound Med. 2003;22(9):879–882; quiz 883–885.
Jakab F, Ráth Z, Schmal F, Nagy P, Faller J. The interaction between hepatic arterial and portal venous blood flows; simultaneous measurement by transit time ultrasonic volume flowmetry. Hepatogastroenterology. 1995;42(1):18–21.
Eipel C, Abshagen K, Vollmar B. Regulation of hepatic blood flow: the hepatic arterial buffer response revisited. World J Gastroenterol. 2010;16(48):6046–6057.
Doi R, Inoue K, Kogire M, et al. Simultaneous measurement of hepatic arterial and portal venous flows by transit time ultrasonic volume flowmetry. Surg Gynecol Obstet. 1988;167(1):65–69.
Loehfelm TW, Tse JR, Jeffrey RB, Kamaya A. The utility of hepatic artery velocity in diagnosing patients with acute cholecystitis. Abdom Radiol (NY). 2018;43(5):1159–1167.
Tse JR, Jeffrey RB, Kamaya A. Performance of Hepatic Artery Velocity in Evaluation of Causes of Markedly Elevated Liver Tests. Ultrasound Med Biol. 2018;44(11):2233–2240.
Vellar ID. The blood supply of the biliary ductal system and its relevance to vasculobiliary injuries following cholecystectomy. Aust N Z J Surg. 1999;69(11):816-820.
Horrow MM, Horrow JC, Niakosari A, Kirby CL, Rosenberg HK. Is age associated with of adult extrahepatic bile duct: sonographic study. Radiology. 2001;221(2):411-414.
Wu CC, Ho YH, Chen CY. Effect of aging on common bile duct diameter: a real-time US study. J Clin Ultrasound. 1984;12(8):473-478.
Itoi T, Kamisawa T, Fujii H et al. Extrahepatic bile duct measurement by using transabdominal US in Japanese adults: multicenter prospective study. J Gastroenterol. 2013;48(9):1045-1050.
Perret RS, Sloop GD, Borne JA. Common Bile Duct Measurements in an elderly population. J Ultrasound Med. 2000;19(11):727-730.
Parulekar SG Ultrasound evaluation of common bile duct size. Radiology. 1979;133(3):703-707.
Rumack CM, Levin D. Diagnostic Ultrasound. Elsevier Health Sciences; 2018.
McArthur TA, Planz V, Fineberg NS, Berland LL, Lockhart ME. CT evaluation of common duct dilation after cholecystectomy and advancing age. Abdom Imaging. 2015;40(6):1581-1586.
Kiriyama S, Takada T, Hwang T-L, et al. Clinical application and verification of the TG13 diagnostic and severity grading criteria for acute cholangitis: an international multicenter observational study. Journal of Hepato-Biliary-Pancreatic Sciences. 2017;24(6):329-337.
Hertzberg MD B, Middleton MD W. Ultrasound: The Requisites. Elsevier Health Sciences; 2015.
Breen DJ, Rutherford EE, Stedman B, Lee-Elliot C, Hacking CN. Intrahepatic arterioportal shunting and anomalous venous drainage: understanding the CT features in the liver. Eur Radiol. 2004;14(12):2249-2260.
Thumar V, Vallurupalli VM, Robinson AL et al. Doppler ultrasound can help diagnose children with hepatic sinusoidal obstructive syndrome after hematopoietic stem cell transplantation. Ultrasound Q. 2016;32(1):58-66.
Go S, Kamaya A, Jeffrey RB, Desser TS. Duplex Doppler ultrasound of the hepatic artery: a window to diagnosis of diffuse liver pathology. 2017;36(4):725-730.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Aya Kamaya, Book royalties, Elsevier. The other authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tse, J.R., Liang, T., Jeffrey, R.B. et al. Does measurement of the hepatic artery velocity improve the sonographic diagnosis of cholangitis?. Abdom Radiol 44, 4004–4010 (2019). https://doi.org/10.1007/s00261-019-02284-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-019-02284-w