Abstract
Objectives
The objective of the study is to identify computed tomography (CT) findings that differentiate hepatic abscess from hepatic metastasis in a patient with a history of extrahepatic malignancy.
Materials and methods
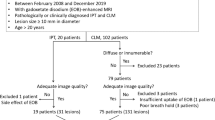
This retrospective study included 30 patients with 93 hepatic abscesses and 40 patients with 125 hepatic metastases who had a history of extrahepatic malignancy and underwent contrast-enhanced dynamic CT with arterial phase (AP) and portal venous phase (PVP). The diagnosis of hepatic abscess and hepatic metastasis was made using pathological confirmation or clinical diagnosis. Margin, patchy parenchymal enhancement, arterial rim enhancement, dynamic change of arterial rim enhancement, size discrepancy of lesions between arterial and portal phases, bile duct dilatation, perilesional hyperemia, and perilesional low density were evaluated by two radiologists independently. Significant findings for differentiating two groups were identified at univariate and multivariate analysis with nomogram for predicting hepatic abscess. Interobserver agreement was also analyzed for each variable.
Results
Multivariate analysis revealed that patchy parenchymal enhancement (P < 0.001), arterial rim enhancement persistent through PVP (P < 0.001), and perilesional hyperemia (P = 0.013) were independent significant findings to predict hepatic abscess than metastasis. Among them, arterial rim enhancement persistent through PVP showed a highest odds ratio (OR 33.73) on multivariate analysis and a highest predictor point on a nomogram for predicting hepatic abscess. When two of these three criteria were combined, 80.7% (75/93) of hepatic abscess were correctly identified, with a specificity of 85.6% (107/125). When all three criteria were satisfied, specificity was up to 100% (125/125).
Conclusions
At contrast-enhanced dynamic CT, patchy parenchymal enhancement, arterial rim enhancement persistent through PVP, perilesional hyperemia, and their combinations may be reliable CT features for differentiating hepatic abscess from metastasis in patients with a history of primary extrahepatic malignancy.





Similar content being viewed by others
Abbreviations
- CT:
-
Computed tomography
- AP:
-
Arterial phase
- PVP:
-
Portal venous phase
- MRI:
-
Magnetic resonance imaging
- HBPI:
-
Hepatobiliary phase image
- TP:
-
Transitional phase
References
Imam K, Bluemke DA (2000) MR imaging in the evaluation of hepatic metastases. Magn Reson Imaging Clin N Am 8(4):741–756
Sica GT, Ji H, Ros PR (2000) CT and MR imaging of hepatic metastases. Am J Roentgenol 174(3):691–698. https://doi.org/10.2214/ajr.174.3.1740691
Krige JEJ, Beckingham IJ (2001) Liver abscesses and hydatid disease. BMJ 322(7285):537–540
Mathieu D, Vasile N, Fagniez PL, et al. (1985) Dynamic CT features of hepatic abscesses. Radiology 154(3):749–752. https://doi.org/10.1148/radiology.154.3.3969480
Jeffrey RB Jr, Tolentino CS, Chang FC, Federle MP (1988) CT of small pyogenic hepatic abscesses: the cluster sign. AJR Am J Roentgenol 151(3):487–489. https://doi.org/10.2214/ajr.151.3.487
Vilgrain V, Esvan M, Ronot M, et al. (2016) A meta-analysis of diffusion-weighted and gadoxetic acid-enhanced MR imaging for the detection of liver metastases. Eur Radiol 26(12):4595–4615. https://doi.org/10.1007/s00330-016-4250-5
Bachler P, Baladron MJ, Menias C, et al. (2016) Multimodality imaging of liver infections: differential diagnosis and potential pitfalls. Radiographics 36(4):1001–1023. https://doi.org/10.1148/rg.2016150196
Méndez RJ, Schiebler ML, Outwater EK, Kressel HY (1994) Hepatic abscesses: MR imaging findings. Radiology 190(2):431–436. https://doi.org/10.1148/radiology.190.2.8284394
Park HJ, Kim SH, Jang KM, et al. (2013) Differentiating hepatic abscess from malignant mimickers: value of diffusion-weighted imaging with an emphasis on the periphery of the lesion. J Magn Reson Imaging 38(6):1333–1341. https://doi.org/10.1002/jmri.24112
Choi SY, Kim YK, Min JH, et al. (2017) The value of gadoxetic acid-enhanced MRI for differentiation between hepatic microabscesses and metastases in patients with periampullary cancer. Eur Radiol 27(10):4383–4393. https://doi.org/10.1007/s00330-017-4782-3
Nino-Murcia M, Olcott EW, Jeffrey RB, et al. (2000) Focal liver lesions: pattern-based classification scheme for enhancement at arterial phase CT. Radiology 215(3):746–751. https://doi.org/10.1148/radiology.215.3.r00jn03746
Kakkar C, Polnaya AM, Koteshwara P, et al. (2015) Hepatic tuberculosis: a multimodality imaging review. Insights Imaging 6(6):647–658. https://doi.org/10.1007/s13244-015-0440-y
Wooten WB, Bernardino ME, Goldstein HM (1978) Computed tomography of necrotic hepatic metastases. AJR Am J Roentgenol 131(5):839–842. https://doi.org/10.2214/ajr.131.5.839
Choi SH, Lee CH, Kim BH, et al. (2013) “Nondefect” of arterial enhancing rim on hepatobiliary phase in 3.0-T gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid-enhanced liver magnetic resonance imaging: distinguishing hepatic abscess from metastasis. J Comput Assist Tomogr 37(6):849–855. https://doi.org/10.1097/RCT.10.1097/RCT.0b013e318297211a
Balci NC, Semelka RC, Noone TC, et al. (1999) Pyogenic hepatic abscesses: MRI findings on T1- and T2-weighted and serial gadolinium-enhanced gradient-echo images. J Magn Reson Imaging 9(2):285–290
Arai K, Kawai K, Kohda W, et al. (2003) Dynamic CT of acute cholangitis: early inhomogeneous enhancement of the liver. Am J Roentgenol 181(1):115–118. https://doi.org/10.2214/ajr.181.1.1810115
Yu J-S, Rofsky NM (2006) Hepatic metastases: perilesional enhancement on dynamic MRI. Am J Roentgenol 186(4):1051–1058. https://doi.org/10.2214/AJR.04.1698
Semelka RC, Hussain SM, Marcos HB, Woosley JT (2000) Perilesional enhancement of hepatic metastases: correlation between MR imaging and histopathologic findings—initial observations. Radiology 215(1):89–94. https://doi.org/10.1148/radiology.215.1.r00mr2989
Park MS, Kim MJ, Lim JS, et al. (2009) Metastasis versus focal eosinophilic infiltration of the liver in patients with extrahepatic abdominal cancer: an evaluation with gadobenate dimeglumine-enhanced magnetic resonance imaging. J Comput Assist Tomogr 33(1):119–124. https://doi.org/10.1097/RCT.0b013e3181641b1a
Lee MH, Kim SH, Kim H, Lee MW, Lee WJ (2011) Differentiating focal eosinophilic infiltration from metastasis in the liver with gadoxetic acid-enhanced magnetic resonance imaging. Korean J Radiol 12(4):439–449. https://doi.org/10.3348/kjr.2011.12.4.439
Qian LJ, Zhu J, Zhuang ZG, et al. (2013) Spectrum of multilocular cystic hepatic lesions: CT and MR imaging findings with pathologic correlation. Radiographics 33(5):1419–1433. https://doi.org/10.1148/rg.335125063
van Leeuwen MS, Noordzij J, Feldberg MA, Hennipman AH, Doornewaard H (1996) Focal liver lesions: characterization with triphasic spiral CT. Radiology 201(2):327–336. https://doi.org/10.1148/radiology.201.2.8888219
Honda H, Matsuura Y, Onitsuka H, et al. (1992) Differential diagnosis of hepatic tumors (hepatoma, hemangioma, and metastasis) with CT: value of two-phase incremental imaging. Am J Roentgenol 159(4):735–740. https://doi.org/10.2214/ajr.159.4.1326884
Lin G, Lunderquist A, Hagerstrand I, Boijsen E (1984) Postmortem examination of the blood supply and vascular pattern of small liver metastases in man. Surgery 96(3):517–526
Mathieu D, Vasile N, Fagniez PL, et al. (1985) Dynamic CT features of hepatic abscesses. Radiology 154(3):749–752. https://doi.org/10.1148/radiology.154.3.3969480
Gabata T, Kadoya M, Matsui O, et al. (2001) Dynamic CT of hepatic abscesses. Am J Roentgenol 176(3):675–679. https://doi.org/10.2214/ajr.176.3.1760675
Pradella S, Centi N, La Villa G, Mazza E, Colagrande S (2009) Transient hepatic attenuation difference (THAD) in biliary duct disease. Abdom Imaging 34(5):626–633. https://doi.org/10.1007/s00261-008-9445-z
Lv P, Lin XZ, Li J, Li W, Chen K (2011) Differentiation of small hepatic hemangioma from small hepatocellular carcinoma: recently introduced spectral CT method. Radiology 259(3):720–729. https://doi.org/10.1148/radiol.11101425
Yu Y, He N, Sun K, et al. (2013) Differentiating hepatocellular carcinoma from angiomyolipoma of the liver with CT spectral imaging: a preliminary study. Clin Radiol 68(9):e491–497. https://doi.org/10.1016/j.crad.2013.03.027
Yu Y, Lin X, Chen K, et al. (2013) Hepatocellular carcinoma and focal nodular hyperplasia of the liver: differentiation with CT spectral imaging. Eur Radiol 23(6):1660–1668. https://doi.org/10.1007/s00330-012-2747-0
Wang Q, Shi G, Qi X, Fan X, Wang L (2014) Quantitative analysis of the dual-energy CT virtual spectral curve for focal liver lesions characterization. Eur J Radiol 83(10):1759–1764. https://doi.org/10.1016/j.ejrad.2014.07.009
Kim JE, Kim HO, Bae K, et al. (2017) Differentiation of small intrahepatic mass-forming cholangiocarcinoma from small liver abscess by dual source dual-energy CT quantitative parameters. Eur J Radiol 92:145–152. https://doi.org/10.1016/j.ejrad.2017.05.012
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2018R1C1B5030985). This work was supported by the Soonchunhyang University Research Fund.
Conflict of interest
J.G.O. declares that he has no conflict of interest. S.Y.C. declares that she has no conflict of interest. H.K.L. declares that she has no conflict of interest. M.H.L. declares that she has no conflict of interest. J.E.L. declares that she has no conflict of interest. B.H.Y. declares that she has no conflict of interest. S.S.K. declares that he has no conflict of interest. J.H.M. declares that she has no conflict of interest. B.L. declares that she has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was waived for retrospective nature of clinical and imaging data collection in this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Oh, J.G., Choi, SY., Lee, M.H. et al. Differentiation of hepatic abscess from metastasis on contrast-enhanced dynamic computed tomography in patients with a history of extrahepatic malignancy: emphasis on dynamic change of arterial rim enhancement. Abdom Radiol 44, 529–538 (2019). https://doi.org/10.1007/s00261-018-1766-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1766-y