Abstract
Cystic dystrophy of heterotopic pancreas is a rare condition that means cystic changes of normal pancreatic tissue, placed in unusual locations, commonly in the duodenal wall. We report a case of CDHP in stomach, histologically confirmed after surgery. We show the correlation between radiological and anatomopathological findings, and also review the current literature about reported cases of this exceptional disease.
Similar content being viewed by others
Heterotopic pancreatic tissue is an aberrant focus of normally developed pancreatic tissue that lacks anatomic and vascular continuity with the main organ and can be found in various locations. Autopsy studies suggest that ectopic pancreatic tissue is quite common (1% to over 13%) but its clinical manifestation is very rare [1]. Most ectopic pancreatic tissue is discovered endoscopically in the duodenum, jejunum and stomach (particularly antrum). Other locations may include ileum, liver, spleen, biliary tract, mesentery, or umbilicus [2]. Commonly, it is anatomically located in the submucosa, but some can be found in the muscularis or serosa. Ectopic pancreatic tissue can undergo similar changes as the pancreas proper, particularly pancreatitis, cystic degeneration, and even ectopic pancreatic cancer formation.
Cystic dystrophy of heterotopic pancreas (CDHP) is very uncommon. It has been described after short series based on surgical specimens. Its natural history is not well known, except its reported relation with chronic pancreatitis [3, 4]. Abdominal radiological studies on the basis of endoscopic ultrasound (EUS), barium contrast studies, computed tomography (CT) and magnetic resonance (MR) offer an optimal approach of this disease before surgical management [3]. However, an accurate diagnosis will require the anatomopathological demonstration of focal disorganization in the wall of the gut, with one or more cystic formations mostly located in the interior of the submucosa or muscularis propria [3].
We present a patient with CDHP within the wall of the gastric body and antrum, who underwent successfully surgical treatment. Abdominal barium-contrasted studies, CT and MR were preoperatively performed. Anatomopathological examination of the biopsy specimen confirmed the definitive diagnosis. To our knowledge, there are no reported cases of radiological and pathological correlation of CDHP in the stomach in the English literature.
Case history
A 38-year-old woman was first seen in our hospital in August 2005 with the complaint of abdominal pain, vomiting after food intake, and weight loss. The diagnosis of acute pancreatitis was initially suspected. She had referred previous episodes of pancreatitis for approximately the past 2 years.
Physical examination was unremarkable, and hematologic examination showed no additional findings.
Endoultrasound was performed, and cystic changes within the gastric wall at the level of the lesser curvature were seen.
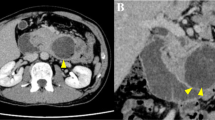
Unenhanced CT examination revealed multiple foci of calcifications within an enlarged gastric wall at the level of the lesser curvature (Fig. 1). After administration of iodinated contrast agent, multiple cysts were seen at the same location, with moderate to strong post-contrast enhancement (Fig. 2).
Abdominal MR confirmed the CT findings, demonstrating multiple cysts along the lesser curvature of the enlarged gastric wall (Fig. 3).
The patient successfully underwent partial gastrectomy (Fig. 4). The postoperative course was uneventful, and the patient was discharged after a few days.
Histological examination finally confirmed ectopic pancreas tissue with cystic changes in the gastric wall.
Discussion
In almost 70% of the patients, ectopic pancreatic tissue is found in the upper GI tract. Among these, the most commonly reported location is the duodenum (periampullary area) [5–7]; less frequent locations are esophagus [8–10], jejunum and ileum [11] and stomach. Histologic examination must reveal ectopic pancreatic tissue composed of acinar and ductal tissue without distribution of islets (Heinrich type II) [12], or cystically dilated duct structures (Heinrich type III) [13].
Most patients with ectopic pancreas are asymptomatic. Clinical findings are due to either primary manifestations from pathologic changes or secondary manifestations from obstruction or compression by the mass effect of the ectopic tissue. Primary manifestations may include episodes of acute pancreatitis, pancreatic cancer, cysts and abscess formation. Secondary manifestations include intussusception, obstructive jaundice/cholestasis and pyloric obstruction and GI bleeding, caused by disruption of submucosal vessels [12].
Cystic dystrophy of heterotopic pancreas (CDHP) is very uncommon. It has been described in short series and case reports on the basis of surgical specimens [3, 4, 15]. In a series of 109 patients [3], it was found involving duodenum (91%), gastric antrum (9%), and jejunum (1%); most of them had more than two cysts and the diameter of the largest was 15 mm. Associated calcifications were found in 11% of the cases, 95% of them in association of chronic pancreatitis.
Its natural history is not well known, except its reported relationship with alcoholism and chronic pancreatitis, although it may appear as an independent disease in almost one-third of the cases [3, 4]. In the reported cases, majority of patients were men (men 90%; relationship men/women 11/1) and the most commonly complaining symptoms were abdominal pain, acute pancreatitis, vomiting after food intake, weight loss [3, 4, 14]. Less frequently reported symptoms were diabetes, cholestasis/jaundice, malabsorption and digestive bleeding [3, 14]. Excepting pancreatic insufficiency, most symptoms are common in both types (with and without chronic pancreatitis/alcoholism) [3]. Furthermore, for some authors CDHP is a manifestation of chronic pancreatitis, in a focus of aberrant pancreatic tissue, which would explain the strong relationship between both entities [14].
Abdominal radiological studies, based on barium contrast studies, endoscopic ultrasound (EUS), computed tomography (CT) and magnetic resonance (MR) offer an optimal approach of this disease before surgical management, as they may demonstrate small cystic formations (often diameter less than 1–1.5 cm), within the enlarged and thickened wall of the duodenum or stomach [3, 14, 15]. Endoscopic ultrasound (EUS), especially with 20 MHz mini probes, may offer an accurate diagnosis as it shows cystic cavities and diffuse intramural infiltration of the submucosa and muscularis propria (fourth hypoechoic layer), allows measurement of the thickened duodenal or gastric wall (commonly between 15–20 mms), and may detect islets of aberrant pancreatic tissue [14, 15].
Preoperative differential diagnosis must be done with other entities characterized by cystic changes, as pancreatic pseudocyst (without a proper wall), gastrointestinal duplication cyst (with a complete five layer wall), gastrointestinal or pancreatic cystic neoplasms (with solid tissue components) or choledococele [14]. However, an accurate diagnosis requires the anatomopathological demonstration of focal disorganization in the wall of the gut, with one or more cystic formations mostly located in the interior of the submucosal or muscularis propria [3, 15].
Non-surgical treatment includes gastric aspiration and intravenous administration of somatostatine or octreotid. If symptoms persist, both endoscopic and surgical resection can be indicated [14].
Although in 11 reported cases of heterotopic pancreas in the stomach [13, 16–25], different complications were described such as pseudocyst, abscess, lithiasis/calcifications, acute pancreatitis or adenocarcinoma, none was properly considered as CDHP. Furthermore, to our knowledge, only four reported cases in the English literature [4, 15, 26, 27] specifically consider CDHP as a proper disease, but occurring in the duodenal wall.
We present the exceptional case of CDHP with calcifications in the lesser curvature of the stomach, along the body and antrum of the gastric wall. The patient was a non-alcoholic young woman who complained of recurrent episodes of pancreatitis, abdominal pain and vomiting. After preoperative radiological examination (including barium contrast studies, abdominal CT and MR), the diagnosis of CDHP was first suspected; histological confirmation was made after successful partial gastrectomy, with a complete clinical recovery of the patient.
References
Prasad TR, Gupta SD, Bhatnagar V (2001) Ectopic pancreas associated with a choledochal cyst and extrahepatic biliary atresia. Pediatr Surg Int 17:552–554
Rizzo RJ, Szucs RA, Turner MA (1995) Congenital abnormalities of the pancreas and biliary tree in adults. Radiographics 15:49–68
Rebours V, Lévy P, Vullierme MP, et al. (2005) Histoire naturelle de la dystrophie kystique sur páncreas aberrant (oral communication). SNFGE, April, pp 596–597
Pessaux P, Lada P, Etienne S, et al. (2006) Duodenopancreatectomy for cystic dystrophy in heterotopic pancreas of the duodenal wall. Gastroenterol Clin Biol 30(1):24–28
Vay Liang WG, Emanuel L, Eugene PD, et al. (1993) The pancreas. 52nd edn. New York: Raven Press, p 1033
Chen CH, Yang CC, Yeh YH, et al. (2001) Ectopic pancreas located in the major duodenal papilla: case report and review. Gastrointest Endosc 53:121–123
Laughlin EH, Keown ME, Jackson JE (1983) Heterotopic pancreas obstructing the ampulla of Vater. Arch Surg 118:979–980
Gananadha S (2005) A unique case of pancreatitis and retention cyst in esophageal heterotopic pancreas. Surg Laparosc Endosc Percutan Tech 15(6):345–347
Goto J, Ohashi S, Okamura S, et al. (2005) Heterotopic pancreas in the esophagus diagnosed by EUS-guided FNA. Gastroint Endosc 62:1894–1898
Roshe J, Buono ED, Domenico D, et al. (1996) Anaplastic carcinoma arising in ectopic pancreas of the distal esophagus. J Clin Gastroenterol 22:242–247
Yenon K (2005) Aberrant pancreas with a double intestinal location. Ann Chir 130 (6, 7):414–416
Tanemura A, Yano T, Tamaki H, et al. (2005) Ectopic pancreas in the minor duodenal papilla presenting as upper-GI bleeding. Gastrointest Endosc 62:571–573
Emerson L (2004) Adenocarcinoma arising in association with gastric heterotopic pancreas: A case report and review of the literature. J Surg Oncol 87(1):53–57
Fischer D (2002) Cystic pseudotumours of the pancreas (oral communication). ANGH, December (26):701–704
Jovanovich I (2004) EUS miniprobes in diagnosis of cystic dystrophy of duodenal wall in heterotopic pancreas: a case report. World J Gastroenterol 10(17):2609–2612
Rubbia-Brandt L (2004) An unusual case of gastric heterotopic pancreas. JOP 5(6):484–487
Yamashita K (2005) Image of the month: a gastric heterotopic pancreas with cystic change. Gastroenterology 129(5):1374
Sukumar N (2004) Heterotopic pancreas in the stomach. Med J Malaysia 59 (4):541–543
De Vogelaere K (2005) Laparoscopic wedge resection for gastric ectopic pancreas Surch Laparosc Endosc Percutan Tech 15 (3):166–168
Lee HY (2003) Lithiasis in a heterotopic pancreas of the stomach. J Comput Assist Tomogr 27(1):85–87
Hirasaki S (2005) Acute pancreatitis occurring in gastric aberrant pancreas treated with surgery and proved by histological examination. Intern Med 44(11):1169–1173
Sciume C (2004) Aberrant pancreas: a rare cause of epigastralgia. Ann Ital Chir 75 (4):483–486
Matsuki M (2005) Adenocarcinoma arising from aberrant pancreas in stomach. J Gastroenterol 40(6):652–656
Surowski S (2004) Ectopic pancreas localized in the stomach. Przegl Lek 61(12):1459–1460
Mulholland KC, Wallace WD, Epanomeritakis E, Hall SR (2004) Pseudocyst formation in gastric ectopic pancreas. J Pancreas 5(6):498–501
Basili E (2003) Cystic dystrophy in heterotopic pancreas of the duodenal wall. Gastroenterol Clin Biol 27(12):1110–1115
Bessoud B (2005) Cystic dystrophy of the duodenal wall and heterotopic pancreas. Presse Med 34(11):825
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Soledad Fernandez Lopez-Pelaez, M., Bergaz Hoyos, F., Garcia Isidro, M. et al. Cystic dystrophy of heterotopic pancreas in stomach: radiologic and pathologic correlation. Abdom Imaging 33, 391–394 (2008). https://doi.org/10.1007/s00261-007-9275-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-007-9275-4