Abstract
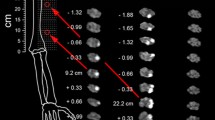
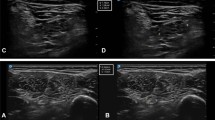
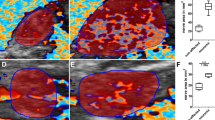
Hourglass-like constriction neuropathy is a neurological condition caused by non-traumatic, non-compressive fascicular constrictions of one or more individual peripheral nerves. Based on clinical manifestations, it is very difficult to differentiate hourglass-like constriction neuropathy from idiopathic neuralgic amyotrophy. Focal hourglass-like constriction neuropathy may be erroneously diagnosed as idiopathic neuralgic amyotrophy. Previous studies demonstrated hourglass-like constrictions of peripheral nerves in the surgical exploration of patients diagnosed with idiopathic neuralgic amyotrophy. Recently, high-resolution ultrasound or magnetic resonance neurography (MRN) have been introduced to detect focal hourglass-like constrictions of peripheral nerves in spontaneous nerve palsy. We present a series of three cases in which the suprascapular nerve was affected by hourglass-like constrictions, which were visualized by high-solution MRN, including a nerve-selective morphological MR pulse sequence with strong fat- and water-signal suppression.



Similar content being viewed by others
References
Van Alfen N, van Eijk JJ, Ennik T, et al. Incidence of neuralgic amyotrophy (parsonage turner syndrome) in a primary care setting—a prospective cohort study. PLoS One. 2015;10:e0128361.
Vigasio A, Marcoccio I. Hourglass-like constriction of the suprascapular nerve: a contraindication for minimally invasive surgery. J Shoulder Elbow Surg. 2018;27:e29–37.
Pan Y, Wang S, Zheng D, et al. Hourglass-like constrictions of peripheral nerve in the upper extremity: a clinical review and pathological study. Neurosurgery. 2014;75:10–22.
Aranyi Z, Csillik A, Devay K, et al. Ultrasonographic identification of nerve pathology in neuralgic amyotrophy: enlargement, constriction, fascicular entwinement, and torsion. Muscle Nerve. 2015;52:503–11.
ArAnyi Z, Csillik A, DeVay K, et al. Ultrasonography in neuralgic amyotrophy: sensitivity, spectrum of findings, and clinical correlations. Muscle Nerve. 2017;56:1054–62.
Sneag DB, Saltzman EB, Meister DW, Feinberg JH, Lee SK, Wolfe SW. MRI Bullseye sign: an indicator of peripheral nerve constriction in parsonage-turner syndrome. Muscle Nerve. 2017;56:99–106.
Kasper JM, Wadhwa V, Scott KM, Rozen S, Xi Y, Chhabra A. SHINKEI—a novel 3D isotropic MR neurography technique: technical advantages over 3DIRTSE-based imaging. Eur Radiol. 2015;25:1672–7.
Lieba-Samal D, Jengojan S, Kasprian G, Wober C, Bodner G. Neuroimaging of classic neuralgic amyotrophy. Muscle Nerve. 2016;54:1079–85.
Vigasio A, Marcoccio I. Homolateral hourglass-like constrictions of the axillary and suprascapular nerves: case report. J Hand Surg Am. 2009;34:1815–20.
Van Alfen N, van Engelen BG. The clinical spectrum of neuralgic amyotrophy in 246 cases. Brain. 2006;129:438–50.
Yamamoto S, Nagano A, Mikami Y, Tajiri Y. Multiple constrictions of the radial nerve without external compression. J Hand Surg Am. 2000;25:134–7.
Duman I, Guvenc I, Kalyon TA. Neuralgic amyotrophy, diagnosed with magnetic resonance neurography in acute stage: a case report and review of the literature. Neurologist. 2007;13:219–21.
Yoneyama M, Takahara T, Kwee TC, Nakamura M, Tabuchi T. Rapid high resolution MR neurography with a diffusion-weighted pre-pulse. Magn Reson Med Sci. 2013;12:111–9.
Sneag DB, Rancy SK, Wolfe SW, et al. Brachial plexitis or neuritis? MRI features of lesion distribution in Parsonage–Turner syndrome. Muscle Nerve. 2018;58:359–66.
Guerra WK, Schroeder HW. Peripheral nerve palsy by torsional nerve injury. Neurosurgery. 2011;68:1018–24; discussion 1024.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional review board.
Disclosure
We did not receive any financial support or other benefits from commercial sources for the work reported in this manuscript, nor did any of the authors have any financial interests with regard to the work that may create a potential conflict of interest or the appearance of one. This work has not been previously presented, submitted, or published in any form or any language.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, D.H., Kim, J. & Sung, D.H. Hourglass-like constriction neuropathy of the suprascapular nerve detected by high-resolution magnetic resonance neurography: report of three patients. Skeletal Radiol 48, 1451–1456 (2019). https://doi.org/10.1007/s00256-019-03174-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-019-03174-4