Abstract
Purpose
To evaluate lower-extremity rotational abnormalities in subjects with achondroplasia using computed tomography (CT) scans.
Materials and methods
CT scans were performed in 25 subjects with achondroplasia (13 skeletally immature, mean age 8.7 years; 12 skeletally mature, mean age 17.6 years). In a total of 50 bilateral limbs, CT images were used to measure the angles of acetabular anteversion, femoral anteversion, and tibial external torion. Measurement was performed by three examiners and then repeated by one examiner. Inter- and intraobserver agreements were analyzed, and results were compared with previously reported normal values.
Results
Mean values for skeletally immature and skeletally mature subjects were 13.6±7.5° and 21.5±6.4° respectively for acetabular anteversion, 27.1±20.8° and 30.5±20.1° for femoral torsion, and 21.6±10.6° and 22.5±10.8° for tibial torsion. Intra- and interobserver agreements were good to excellent. Acetabular anteversion and femoral anteversion in skeletally mature subjects were greater than normal values in previous studies. Both skeletally immature and mature subjects with achondroplasia had decreased tibial torsion compared to normal skeletally immature and mature subjects.
Conclusion
Lower-extremity rotational abnormalities in subjects with achondroplasia include decreased tibial external torsion in both skeletally immature and mature subjects, as well as increased femoral and acetabular anteversion in skeletally mature subjects.
Similar content being viewed by others
Introduction
Lower-extremity deformities in achondroplasia include coxa vara, genu varum, and heel varus, which result from abnormalities in longitudinal growth. Torsional deformity of the femur and the tibia are frequently associated, and lead to periarticular pain and eventual arthritis [1–3]. Usually this rotational malalignment becomes more apparent after the correction of severe angular deformity, thereby requiring a second operation later [3, 4]. Femoral anteversion greater than 50°, or medial hip rotation greater than 85°, or lateral rotation less than 10° in a child over 8 years of age are indications of corrective surgery. Tibial medial torsion beyond 15° and lateral torsion beyond 30° are considered as indications of surgery, and the goal of surgery is to achieve a thigh–foot angle of 20° [5–7]. Therefore, evaluation of combined rotational deformity is necessary when performing osteotomies for correction of these deformities. Clinical and radiographic measurements using biplane radiographs cannot give exact information of rotational deformity because of limited intra- and interobserver reliability [6, 8]. Computed tomography (CT) is a more accurate method for measuring rotational deformity in the lower extremity of the body. To the best of our knowledge, there is no report that describes measurement of lower-extremity rotation in subjects with achondroplasia using clinical methods and plain radiographs, as well as CT scan. We report the lower-extremity rotation profiles measured by CT in 25 subjects with achondroplasia.
Materials and methods
Our series included 25 subjects with achondroplasia. The diagnoses in all subjects was achieved using gene mutation analyses between December 2000 and January 2004. Informed consent for DNA analysis was obtained from the subjects and/or their parents, depending on the subject’s age. All exon 8 of FGFR3 gene was amplified by polymerase chain reaction (PCR) using primers located in the flanking introns. All subjects had glycine-to-arginine substation at residue 380 (G380R) of fibroblast growth factor receptor 3 (FGFR3).
Of the total 25 subjects, 12 were female and 13 were male. There were 13 subjects before skeletal growth, and 12 subjects after skeletal growth, who were over 14 years old and with closure of the physis. Mean age for total subject population was 15.6 years (range, 6-37 years). Mean age was 8.7 years for skeletally immature subjects and 17.6 years for skeletally mature subjects.
All subjects underwent lower-extremity CT for preoperative evaluation of lower-extremity rotational profile. Corrective and lengthening osteotomies of bilateral lower extremities were performed in all subjects. Informed consent for preoperative CT scan and operation was taken from all subjects.
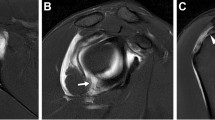
Bilateral torsion of the acetabulum, femur, and tibia in 50 limbs were measured using two multidetector-row CT scanners, LightSpeed Plus (General Electric Medical Systems, Milwaukee, WI, USA) and SOMATOM Sensation 16 (Siemens, Forchheim, Germany), with 5.5-mm slice thickness. During the CT examination each subject was in a supine position, with the patella in a forward position and the hip and knee in extension. Axial CT studies of the hip were taken from the superior acetabulum to the lower border of lesser trochanter. We measured the acetabular anteversion as the angle formed by a reference line perpendicular to a line connecting the posterior ischia and a line connecting the posterior and anterior margins of the acetabulum at the center of the hip joint (Fig. 1) [9, 10]. In the proximal femur, the section that showed the greater trochanter, femoral neck, and femoral head was selected (Fig. 2a). When all of them were not visible in one axial scan, we selected a section that showed femur neck and greater trochanter. In the distal femur and proximal tibia, CT scans were taken from the supracondylar region down to tibial tuberosity. In the distal femur, we selected the section that showed the largest medial and lateral femoral condyles (Fig. 2b). In the proximal tibia, we selected the section immediately below the joint line that showed the entire anterior and posterior border of the proximal tibial condyle (Fig. 3a). In the distal tibia, we selected the section immediately above the joint line that showed medial and lateral malleoli (Fig. 3b). The femoral torsion was measured by the tabletop method (Fig. 2) [11]. According to this method, the line joining the centers of the head and the neck was considered the proximal reference line. When it was impossible to draw this line due to dysplasia, we drew the line parallel to the femur neck (Fig. 2a). The line tangent to the most posterior points of the femoral condyle was considered the distal reference line (Fig. 2b). The angle between proximal and distal reference lines was defined as the femoral anteversion angle (Fig. 2). The tibial torsion was measured by the method advocated by Laasonen et al. (Fig. 3) [12]. According to this method, the proximal tibial condyle appears as an ellipse. The estimated long axis of this tibial condylar ellipse was selected as the proximal reference line (Fig. 3a). In the distal tibia, the axis through the centers of medial and lateral malleoli was taken as the distal reference line (Fig. 3b). The angle between the proximal and distal reference lines was defined as the tibial torsion angle (Fig. 3).
In the proximal femur, the CT scan shows the section that showed the greater trochanter, femoral neck, and femoral head (a). In the distal femur, the CT scans shows the section that showed the largest medial and lateral femoral condyles (b). The angle between the line parallel to the femoral neck and the line tangent to the most posterior points of femoral condyles was defined as the femoral anteversion angle
In the proximal tibia, the CT scan shows the section immediately below the joint line that showed the entire anterior and posterior border of proximal tibial condyle (a). In the distal tibia, the CT scan shows the section immediately above the joint line that showed medial and lateral malleoli (b). Tibial torsion angle was defined as the angle between the estimated long axis line of tibial condylar ellipse and the axis line through the centers of medial and lateral malleoli
All measurements were taken by three examiners, including two orthopaedic surgeons (observer 1, 2) and one radiologist (observer 3), for evaluation of interobserver variation. To determine the intraobserver variation, the measurement was repeated 1 month later by one of the same examiners (observer 1). Intraobserver agreements between two sets of measurements of observer 1 and interobserver agreements between three sets of measurements of observer 1, 2, 3 were analyzed using Pearson correlation coefficient and intraclass correlation coefficient (ICC). An ICC value greater than 0.75 is excellent, from 0.40 to 0.75 is fair to good, and less than 0.40 is poor. We compared the mean angles of acetabular verion, femoral torsion, and tibial torsion with the corresponding normal values that had been reported previously in the skeletally immature and mature achondroplasia groups separately, using the t-test.
Results
In total, 50 limbs were studied. The mean angle of acetabular anteversion was 13.6±7.5° in 26 limbs of skeletally immature subjects and 21.5±6.4° in 24 skeletally mature subjects (Table 1). The acetabular anteversion angle in the skeletally mature achondroplasia group was significantly increased compared to the normal values of Seber et al. (mean 15.6±4.8° in right, 15.8±5.8° in left; p<0.05) [13], but did not differ from the other normal value of Kim et al. (mean 20.7±2.9°) [9]. There was no statistically significant difference between the acetabular version angle of childhood achondroplasia and normal values reported (Table 1) [9, 10].
The mean angle of femoral torsion was 27.1±20.8° in skeletally immature subjects and 30.5±20.1° in skeletally mature subjects (Table 1). The mean angle of femoral torsion in the group of skeletally matured achondroplasia was significantly increased compared to the normal values previously reported by Seber et al. (6.5±7.7° in right, 5.8±8.4° in left) [13], Yagi et al. (15.6±6.7°) [14], and Moussa et al. (16.1±8.2°) [15]. The mean angle of femoral torsion in the skeletally immature achondroplasia group did not differ from the normal value reported by Fabry et al. (24.0±5°) [16].
The mean angle of tibial torsion was 21.6±10.6° in skeletally immature subjects and 22.5±10.8° in skeletally mature subjects (Table 1). The result of childhood achondroplasia was significantly decreased compared to the normal value reported by Kristinansen et al. (mean 33.6±6.5°) [17], and significantly increased compared to the result of Valmassy et al. (11.2±2.7°) [18]. The result of skeletally mature subjects with achondroplasia was significantly decreased compared to the normal values reported by Moussa et al. (mean 34±6.7°) [15], Jend et al. (mean 40±9°) [19], and Seber et al. (mean 30.9±7.1° in right, 29.1±6.9° in left) [13], but did not differ from the value of Yagi et al. (mean 23.5±5.1°) [14].
The intraobserver agreement was excellent (ICC value >0.9) in the measurement of acetabular anteversion, femoral torsion, and tibial torsion (Table 2). The interobserver agreements of the three examiners were excellent (ICC values >0.7) in all measurements except tibial torsion, which revealed fair to good agreement (ICC values between 0.4 and 0.7).
Discussion
The characteristics of achondroplasia are shortened long bone and wide metaphysis in the lower extremity due to endochondral ossification failure. The femoral neck is short due to decreased longitudinal growth, whereas the greater trochanter has normal growth affected by periosteal ossification. These findings lead to the appearance of coxa vara, even though the femoral neck-to-shaft angle is normal and there is no true coxa vara. Differential growth between the anterior part (or medial part) and the posterior part (or lateral part) of the physis may produce torsional deformity and deformed femoral head, with sagging rope sign which presents overlap of deformed femoral head and the metaphysis. In achondroplasia, the fibular growth exceeds the tibial growth, and so the fibula is longer at the knee and ankle. The suggested reason is that there are proportionately larger peripheral physis in smaller-calibered fibula than tibia, and hence proportionately more peripheral growth [20]. The longer fibula at the knee produces laxity of the lateral collateral ligament, which aggravates genu varum deformity. The longer fibula at the ankle causes increased pressure on the medial distal tibial physis, resulting in varus deformity of the distal tibia. The longer fibula also limits eversion of the subtalar joint and external rotation of the foot, which may contribute to torsional deformity of the tibia. Thus, a skeletally immature subject presents with the tibial medial torsion deformity along with varus deformity of the knee. This developmental deformity can correct itself as the subjects mature skeletally, due to the growth at both the upper and lower tibial epiphysis up to the age of 8 years. Therefore, corrective surgery should be undertaken after 8 years of age [7] and CT should only be performed for surgical preparation in order to accurately measure the medial torsion of the tibia.
It is impossible to measure the femoral torsion during clinical examination, whereas it is possible to measure the tibial torsion using the thigh-to-foot angle or the transmalleolar axis. Valmassy and Stanton reported that the mean tibial torsion in the normal population using the transmalleolar axis was 5–6° at 1–2 years, increased by 1.4° per year, and became 11.2° at the age of 6 years [18]. The tibial torsion results from the skeletally immature subjects in our study were higher than the results of Valmassy and Stanton [18], but the ages of the skeletally immature subjects in the study of Valmassy and Stanton were less than 6 years. Staheli et al. described that the mean thigh–foot angle in normal population was 10° (-5–30°) and the mean angle of transmalleolar axis was 20° (0–45°) at the age of 7–10 years [6]. Using CT methods, Kristiansen et al. found that the mean tibial torsion in a normal population was 28° (20–37°) at the age of 4 years, increased by 1° per year, became 32–33° at age of 7–10 years, and 38° (18–47°) at skeletal maturation [17]. Several investigators also found that the mean tibial torsion in a normal skeletally mature population ranged from 24° to 40° using CT methods [13–15, 19]. The present study dealt with achondroplasia subjects, and the mean tibial torsion was significantly decreased compared to the normal values in skeletally immature subjects and skeletally mature subjects, which were 21.6±10.6° and 22.5±10.8° respectively. These results mean that there was decreased tibial torsion at the middle of childhood, no increase of external torsion during growth, and residual decreased tibial torsion in skeletally mature subjects with achondroplasia. The interobserver agreement of the tibial torsion is relatively poorer than the other measurements. This could in part be due due to ankle varus in achondroplasia subjects, which results in difficulty for observers in choosing the CT section that showed both lateral and medial malleoli.
Regarding the femoral torsion, CT data of normal skeletally immature subjects has not been reported in previous studies. Fabry et al. reported that skeletally immature subjects with toe-in gait due to increased tibial torsion had normal femoral anteversion, with mean of 24±5.6° measured by CT [16]. Previous studies with CT found that the mean femoral anteversion ranged from 6° to 16° in skeletally matured subjects, and the variation of the data resulted from different methods of measurement [13–15, 19]. These results suggest that the femoral anteversion decreased during growth in the normal population. There was no difference between the mean femoral torsion angle of achondroplasia subjects and the normal value in skeletally immature subjects. However, the femoral torsional angle of achondroplasia subjects was significantly higher than the normal values in skeletally mature subjects. These results suggested that the normal decrease of femoral anteversion during growth may be deficient in subjects with achondroplasia.
The mean acetabular anteversion has been reported by several investigators to range from 13° to 18° in normal skeletally immature subjects, and from 16° to 20° in normal skeletally mature subjects [9, 10, 13]. In our study, the mean acetabular anteversion was not different from the normal values in the skeletally immature achondroplasia group, but it significantly increased in the skeletally mature achondroplasia group compared to the normal value reported by Seber et al. [13]. These results may suggest increased acetabular anteversion related to increased femoral anteversion in skeletally mature subjects with achondroplasia.
We can conclude that there was decreased tibial external torsion in skeletally immature subjects with achondroplasia. Also, there was increased acetabular anteversion, increased femoral anteversion, and decreased tibial external torsion in skeletally mature subjects with achondroplasia. We suggest that there was persistently decreased tibial external torsion, lack of normal decrease in femoral anteversion, and related increase of acetabular anteversion, during growth, in the subjects with achondroplasia. So the torsional deformity should be evaluated carefully before surgery, and treated during correction of angular deformities in achondroplasia.
References
Paley D, Tetsworth K. Mechanical axis deviation of lower limbs: Preoperative planning of multiapical frontal plane angular and bowing deformities of the femur and tibia. Clin Orthop 1992;280:65–71.
Turner MS. The association between tibial torsion and knee joint pathology. Clin Orthop 1994;302:47–51.
Herzenberg JE, Smith JD, Paley D. Correcting torsion deformities with Ilizarov’s apparatus. Clin Orthop 1991;302:36–41.
Herzenberg JE, Waanders NA. Calculating rate and duration of distraction for deformity correction with the Ilizarov technique. Orthop Clin North Am 1991;22:601–11.
Delgado WD, Schoenecker PL, Rich MM, Capelli RN. Treatment of severe malalignment syndrome. J Pediatr Orthop 1996;16:484–88.
Staheli LT, Corbett M, Wyss C, King H. Lower-extremity rotational problems in children. Normal values to guide management. J Bone Joint Surg Am 1985;67:39–47.
Staheli LT. Torsion-treatment indications. Clin Orthop 1989;247:61–6.
Stuberg W, Temme J, Kaplan P, Clarke A, Fuchs R. Measurement of tibial torsion and thigh-foot angle using goniometry and computed tomography. Clin Orthop 1991;272:208–12.
Kim SS, Frick SL, Wenger DR. Anteversion of the acetabulum in developmental dysplasia of the hip. analysis with computed tomography. J Pediatr Orthop 1999;19:438–42.
Jacquemier M, Jouve JL, Bolllini G, Panu M, Migliani R. Acetabular anteversion in children. J Pediatr Orthop 1992;12:373–75.
Murphy SB, Simon SR, Kijewski PK, Wilkinson RH, Griscom NT. Femoral anteversion. J Bone Joint Surg Am 1987;69:1169–76.
Laasonen EM, Jokio P, Lindholm TS. Tibial torsion measured by computed tomography. Acta Radiol 1984;25:325–29.
Seber S, Hazer B, Kose N, Gokturk E, Gunal I, Turgut A. Rotational profile of the lower extremity and foot progression angle. computerized tomographic examination of 50 male adults. Arch Orthop Trauma Surg 2000;120:255–58.
Yagi T, Sasaki T. Tibial torsion in patients with medial-type osteoarthritic knee. Clin Orthop 1986;213:177–82.
Moussa M. Rotational malalignment and femoral torsion in osteoarthritic knees with patellofemoral joint involvement. A CT scan study. Clin Orthop 1994;304:176–83.
Fabry G, Cheng LX, Molenaers G. Normal and abnormal torsional development in children. Clin Orthop 1994;302:22–6.
Kristiansen LP, Gunderson RB, Steen H, Reikeras O. The normal development of tibial torsion. Skeletal Radiol 2001;30:519–22.
Valmassy R, Stanton B. Tibial torsion. Normal values in children. J Am Podiatr Med Assoc 1989:79;432–35.
Jend HH, Heller M, Dallek M, Schoettle H. Measurement of tibial torsion by computer tomography. Acta Radiol 1981;22:271–76.
Ponseti IV. Skeletal growth in achondroplasia. J Bone Joint Surg Am 1970;52:701–16.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Song, HR., Choonia, AT., Hong, S.J. et al. Rotational profile of the lower extremity in achondroplasia: computed tomographic examination of 25 patients. Skeletal Radiol 35, 929–934 (2006). https://doi.org/10.1007/s00256-006-0180-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-006-0180-7