Abstract
Whether or not treatment with antibiotics or probiotics for bacterial vaginosis (BV) is associated with a change in the diversity of vaginal microbiota in women was investigated. One hundred fifteen women, consisting of 30 healthy subjects, 30 BV-positive control subjects, 30 subjects with BV treated with a 7-day metronidazole regimen, and 25 subjects with BV treated with a 10-day probiotics regimen, were analyzed to determine the efficacy and disparity of diversity and richness of vaginal microbiota using 454 pyrosequencing. Follow-up visits at days 5 and 30 showed a greater BV cure rate in the probiotics-treated subjects (88.0 and 96 %, respectively) compared to the metronidazole-treated subjects (83.3 and 70 %, respectively [p = 0.625 at day 5 and p = 0.013 at day 30]). Treatment with metronidazole reduced the taxa diversity and eradicated most of the BV-associated phylotypes, while probiotics only suppressed the overgrowth and re-established vaginal homeostasis gradually and steadily. Despite significant interindividual variation, the microbiota of the actively treated groups or participants constituted a unique profile. Along with the decrease in pathogenic bacteria, such as Gardnerella, Atopobium, Prevotella, Megasphaera, Coriobacteriaceae, Lachnospiraceae, Mycoplasma, and Sneathia, a Lactobacillus-dominated vaginal microbiota was recovered. Acting as vaginal sentinels and biomarkers, the relative abundance of Lactobacillus and pathogenic bacteria determined the consistency of the BV clinical and microbiologic cure rates, as well as recurrent BV. Both 7-day intravaginal metronidazole and 10-day intravaginal probiotics have good efficacy against BV, while probiotics maintained normal vaginal microbiota longer due to effective and steady vaginal microbiota restoration, which provide new insights into BV treatment.




Similar content being viewed by others
References
Ling Z, Kong J, Liu F, Zhu H, Chen X, Wang Y, Li L, Nelson KE, Xia Y, Xiang C (2010) Molecular analysis of the diversity of vaginal microbiota associated with bacterial vaginosis. BMC Genomics 11:488
Fredricks DN, Fiedler TL, Marrazzo JM (2005) Molecular identification of bacteria associated with bacterial vaginosis. N Engl J Med 353:1899–1911
Hillier SL, Krohn MA, Rabe LK, Klebanoff SJ, Eschenbach DA (1993) The normal vaginal flora, H2O2-producing lactobacilli, and bacterial vaginosis in pregnant women. Clin Infect Dis 16(Suppl 4):S273–281
Ravel J, Gajer P, Abdo Z, Schneider GM, Koenig SS, McCulle SL, Karlebach S, Gorle R, Russell J, Tacket CO, Brotman RM, Davis CC, Ault K, Peralta L, Forney LJ (2011) Vaginal microbiome of reproductive-age women. Proc Natl Acad Sci U S A 108(Suppl 1):4680–4687
Hummelen R, Fernandes AD, Macklaim JM, Dickson RJ, Changalucha J, Gloor GB, Reid G (2010) Deep sequencing of the vaginal microbiota of women with HIV. PLoS One 5:e12078, LID - e12078 [pii]
Carey JC, Klebanoff MA, Hauth JC, Hillier SL, Thom EA, Ernest JM, Heine RP, Nugent RP, Fischer ML, Leveno KJ, Wapner R, Varner M (2000) Metronidazole to prevent preterm delivery in pregnant women with asymptomatic bacterial vaginosis. National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med 342:534–540
Workowski KA, Berman S (2010) Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep 59:1–110
Bradshaw CS, Morton AN, Hocking J, Garland SM, Morris MB, Moss LM, Horvath LB, Kuzevska I, Fairley CK (2006) High recurrence rates of bacterial vaginosis over the course of 12 months after oral metronidazole therapy and factors associated with recurrence. J Infect Dis 193:1478–1486
Sobel JD, Schmitt C, Meriwether C (1993) Long-term follow-up of patients with bacterial vaginosis treated with oral metronidazole and topical clindamycin. J Infect Dis 167:783–784
Sobel JD, Ferris D, Schwebke J, Nyirjesy P, Wiesenfeld HC, Peipert J, Soper D, Ohmit SE, Hillier SL (2006) Suppressive antibacterial therapy with 0.75% metronidazole vaginal gel to prevent recurrent bacterial vaginosis. Am J Obstet Gynecol 194:1283–1289
Anukam K, Osazuwa E, Ahonkhai I, Ngwu M, Osemene G, Bruce AW, Reid G (2006) Augmentation of antimicrobial metronidazole therapy of bacterial vaginosis with oral probiotic Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14: randomized, double-blind, placebo controlled trial. Microbes Infect 8:1450–1454
Uehara S, Monden K, Nomoto K, Seno Y, Kariyama R, Kumon H (2006) A pilot study evaluating the safety and effectiveness of Lactobacillus vaginal suppositories in patients with recurrent urinary tract infection. Int J Antimicrob Agents 28(Suppl 1):S30–34
Mastromarino P, Macchia S, Meggiorini L, Trinchieri V, Mosca L, Perluigi M, Midulla C (2009) Effectiveness of Lactobacillus-containing vaginal tablets in the treatment of symptomatic bacterial vaginosis. Clin Microbiol Infect 15:67–74
Petricevic L, Witt A (2008) The role of Lactobacillus casei rhamnosus Lcr35 in restoring the normal vaginal flora after antibiotic treatment of bacterial vaginosis. BJOG 115:1369–1374
Fredricks DN, Fiedler TL, Thomas KK, Mitchell CM, Marrazzo JM (2009) Changes in vaginal bacterial concentrations with intravaginal metronidazole therapy for bacterial vaginosis as assessed by quantitative PCR. J Clin Microbiol 47:721–726
Amsel R, Totten PA, Spiegel CA, Chen KC, Eschenbach D, Holmes KK (1983) Nonspecific vaginitis. Diagnostic criteria and microbial and epidemiologic associations. Am J Med 74:14–22
Nugent RP, Krohn MA, Hillier SL (1991) Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol 29:297–301
Ling Z, Liu X, Chen X, Zhu H, Li L, Nelson KE, Xia Y, Xiang C (2011) Diversity of cervicovaginal microbiota associated with female lower genital tract infections. Microb Ecol 61:704–714
Ling Z, Kong J, Jia P, Wei C, Wang Y, Pan Z, Huang W, Li L, Chen H, Xiang C (2010) Analysis of oral microbiota in children with dental caries by PCR-DGGE and barcoded pyrosequencing. Microb Ecol 60:677–690
Ferris MJ, Masztal A, Aldridge KE, Fortenberry JD, Fidel PL Jr, Martin DH (2004) Association of Atopobium vaginae, a recently described metronidazole resistant anaerobe, with bacterial vaginosis. BMC Infect Dis 4:5
Martinez RC, Franceschini SA, Patta MC, Quintana SM, Gomes BC, De Martinis EC, Reid G (2009) Improved cure of bacterial vaginosis with single dose of tinidazole (2 g), Lactobacillus rhamnosus GR-1, and Lactobacillus reuteri RC-14: a randomized, double-blind, placebo-controlled trial. Can J Microbiol 55:133–138
Reid G, Bruce AW, Fraser N, Heinemann C, Owen J, Henning B (2001) Oral probiotics can resolve urogenital infections. FEMS Immunol Med Microbiol 30:49–52
Reid G, Younes JA, Van der Mei HC, Gloor GB, Knight R, Busscher HJ (2011) Microbiota restoration: natural and supplemented recovery of human microbial communities. Nat Rev Microbiol 9:27–38
Aroutcheva A, Gariti D, Simon M, Shott S, Faro J, Simoes JA, Gurguis A, Faro S (2001) Defense factors of vaginal lactobacilli. Am J Obstet Gynecol 185:375–379
Hawes SE, Hillier SL, Benedetti J, Stevens CE, Koutsky LA, Wolner-Hanssen P, Holmes KK (1996) Hydrogen peroxide-producing lactobacilli and acquisition of vaginal infections. J Infect Dis 174:1058–1063
Anukam K, Osazuwa E, Ahonkhai I, Ngwu M, Osemene G, Bruce AW, Reid G (2006) Augmentation of antimicrobial metronidazole therapy of bacterial vaginosis with oral probiotic Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14: randomized, double-blind, placebo controlled trial. Microbes Infect 8:1450–1454
Stapleton AE, Au-Yeung M, Hooton TM, Fredricks DN, Roberts PL, Czaja CA, Yarova-Yarovaya Y, Fiedler T, Cox M, Stamm WE (2011) Randomized, placebo-controlled phase 2 trial of a Lactobacillus crispatus probiotic given intravaginally for prevention of recurrent urinary tract infection. Clin Infect Dis 52:1212–1217
Antonio MA, Meyn LA, Murray PJ, Busse B, Hillier SL (2009) Vaginal colonization by probiotic Lactobacillus crispatus CTV-05 is decreased by sexual activity and endogenous Lactobacilli. J Infect Dis 199:1506–1513
Acknowledgments
This work was supported by the National Basic Research Program of China (973 program) Grant 2013CB531404 and a Qiu-Shi Scholarship from Zhejiang University. We would like to thank all the participants recruited in this study.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Zongxin Ling, Xia Liu, and Weiguang Chen contributed equally to this work.
Clinical Trial Registration: ChiCTR-TRC-11001484 (www.chictr.org)
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 139 kb)
Table S1
The clinical data for each participant in our study (XLS 48 kb)
Table S2
Comparison of phylotype coverage and diversity estimation of the 16S rRNA gene libraries at the 3 % dissimilarity from the pyrosequencing analysis (DOC 39 kb)
Table S3
All genera assigned using the RDP classifier with at least 50 % as bootstrap support (XLS 299 kb)
Table S4
The abundance of vaginal bacteria relative to total Bacteria gene copy number by species-specific qPCR for clinical cured participants in the 5-day follow-up after treatment (DOC 47 kb)
Table S5
List of the 112 8-bp barcodes used to tag each PCR product analyzed as part of the study (DOC 42 kb)
Table S6
Species-specific primer sets for detection of vaginal bacteria by qPCR (DOC 84 kb)
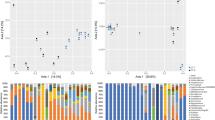
Fig. S1
Differences of phylum (A) and predominant genera (B) detected in vagina from CN, BV, and BV treated with metronidazole and Lactobacillus individuals (*p < 0.05, **p < 0.01) (JPEG 42 kb)
Fig. S2
Interindividual variations in the proportion of major phyla (A) and genera (B) in 115 vaginal samples from four groups. Only the seven largest phyla and 23 largest genera are shown in the figure. These data illustrate the dramatic interindividual variation (JPEG 120 kb)
Rights and permissions
About this article
Cite this article
Ling, Z., Liu, X., Chen, W. et al. The Restoration of the Vaginal Microbiota After Treatment for Bacterial Vaginosis with Metronidazole or Probiotics. Microb Ecol 65, 773–780 (2013). https://doi.org/10.1007/s00248-012-0154-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00248-012-0154-3