Abstract
Background
Leg length discrepancy (LLD) is a common problem that can cause long-term musculoskeletal problems. However, measuring LLD on radiography is time-consuming and labor intensive, despite being a simple task.
Objective
To develop and evaluate a deep-learning algorithm for measurement of LLD on radiographs.
Materials and methods
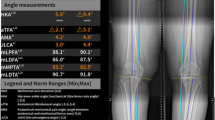
In this Health Insurance Portability and Accountability Act (HIPAA)-compliant retrospective study, radiographs were obtained to develop a deep-learning algorithm. The algorithm developed with two U-Net models measures LLD using the difference between the bilateral iliac crest heights. For performance evaluation of the algorithm, 300 different radiographs were collected and LLD was measured by two radiologists, the algorithm alone and the model-assisting method. Statistical analysis was performed to compare the measurement differences with the measurement results of an experienced radiologist considered as the ground truth. The time spent on each measurement was then compared.
Results
Of the 300 cases, the deep-learning model successfully delineated both iliac crests in 284. All human measurements, the deep-learning model and the model-assisting method, showed a significant correlation with ground truth measurements, while Pearson correlation coefficients and interclass correlations (ICCs) decreased in the order listed. (Pearson correlation coefficients ranged from 0.880 to 0.996 and ICCs ranged from 0.914 to 0.997.) The mean absolute errors of the human measurement, deep-learning-assisting model and deep-learning-alone model were 0.7 ± 0.6 mm, 1.1 ± 1.1 mm and 2.3 ± 5.2 mm, respectively. The reading time was 7 h and 12 min on average for human reading, while the deep-learning measurement took 7 min and 26 s. The radiologist took 74 min to complete measurements in the deep-learning mode.
Conclusion
A deep-learning U-Net model measuring the iliac crest height difference was possible on teleroentgenograms in children. LLD measurements assisted by the deep-learning algorithm saved time and labor while producing comparable results with human measurements.




Similar content being viewed by others
References
Subotnick SI (1981) Limb length discrepancies of the lower extremity (the short leg syndrome). J Orthop Sports Phys Ther 3:11–16
Woerman AL, Binder-Macleod SA (1984) Leg length discrepancy assessment: accuracv and precision in five clinical methods of evaluation*. J Orthop Sports Phys Ther 5:230–239
Giles LG, Taylor JR (1981) Low-back pain associated with leg length inequality. Spine (Phila Pa 1976) 6:510–521
Gofton JP, Trueman GE (1971) Studies in osteoarthritis of the hip. II. Osteoarthritis of the hip and leg-length disparity. Can Med Assoc J 104:791–799
Brunet ME, Cook SD, Dickinson BMR, JA, (1990) A survey of running injuries in 1505 competitive and recreational runners. J Sports Med Phys Fitness 30:307–315
Murrell P, Cornwall MW, Doucet SK (1991) Leg-length discrepancy: effect on the amplitude of postural sway. Arch Phys Med Rehabil 72:646–648
Sabharwal S, Kumar A (2008) Methods for assessing leg length discrepancy. Clin Orthop Relat Res 466:2910–2922
Moseley CF (1986) Leg-length discrepancy. Pediatr Clin North Am 33:1385–1394
Cleveland RH, Kushner DC, Ogden MC et al (1988) Determination of leg length discrepancy. A comparison of weight-bearing and supine imaging. Invest Radiol 23:301–304
Lampe HI, Swierstra BA, Diepstraten AF (1996) Measurement of limb length inequality. Comparison of clinical methods with orthoradiography in 190 children. Acta Orthop Scand 67:242–244
Guichet JM, Spivak JM, Trouilloud P, Grammont PM (1991) Lower limb-length discrepancy. An epidemiologic study. Clin Orthop Relat Res 272:235–241
Weinstein SL, Flynn JM (eds) (2014) Lovell and Winter's Pediatric orthopaedics, 7th edn. Lippincott Williams & Wilkins, Philadelphi, pp 618, 1360–1361
Gross RH (1978) Leg length discrepancy: how much is too much? Orthopedics 1:307–310
Reid DC, Smith B (1984) Leg length inequality: a review of etiology and management. Physiother Can 36:177–182
Kaufman KR, Miller LS, Sutherland DH (1996) Gait asymmetry in patients with limb-length inequality. J Pediatr Orthop 16:144–150
Bhave A, Paley D, Herzenberg JE (1999) Improvement in gait parameters after lengthening for the treatment of limb-length discrepancy. J Bone Joint Surg Am 81:529–534
Shin CH, Lee DJ, Choi IH et al (2018) Clinical and radiological outcomes of arthroscopically assisted cannulated screw fixation for tibial eminence fracture in children and adolescents. BMC Musculoskelet Disord 19:41
Yoon C, Shin CH, Kim DO et al (2020) Overgrowth of the lower limb after treatment of developmental dysplasia of the hip: incidence and risk factors in 101 children with a mean follow-up of 15 years. Acta Orthop 91:197–202
Shin CH, Lim C, Kim HY et al (2021) Prospective study of epigenetic alterations responsible for isolated hemihyperplasia/hemihypoplasia and their association with leg length discrepancy. Orphanet J Rare Dis 16:418
Horng S, Liao R, Wang X et al (2021) Deep learning to quantify pulmonary edema in chest radiographs. Radiol Artif Intell 3:e190228
Larson DB, Chen MC, Lungren MP et al (2018) Performance of a deep-learning neural network model in assessing skeletal maturity on pediatric hand radiographs. Radiology 287:313–322
Krogue JD, Cheng KV, Hwang KM et al (2020) Automatic hip fracture identification and functional subclassification with deep learning. Radiol Artif Intell 2:e190023
Choi JW, Cho YJ, Lee S et al (2020) Using a dual-input convolutional neural network for automated detection of pediatric supracondylar fracture on conventional radiography. Invest Radiol 55:101–110
Choi JW, Cho YJ, Ha JY et al (2022) Deep learning-assisted diagnosis of pediatric skull fractures on plain radiographs. Korean J Radiol 23:343–354
Zheng Q, Shellikeri S, Huang H et al (2020) Deep learning measurement of leg length discrepancy in children based on radiographs. Radiology 296:152–158
Rouzrokh P, Wyles CC, Philbrick KA et al (2021) A deep learning tool for automated radiographic measurement of acetabular component inclination and version after total hip arthroplasty. J Arthroplasty 36(2510–2517):e2516
Cho BH, Kaji D, Cheung ZB et al (2020) Automated measurement of lumbar lordosis on radiographs using machine learning and computer vision. Global Spine J 10:611–618
Gorelik N, Gyftopoulos S (2021) Applications of artificial intelligence in musculoskeletal imaging: from the request to the report. Can Assoc Radiol J 72:45–59
Mutasa S, Yi PH (2021) Clinical artificial intelligence applications: musculoskeletal. Radiol Clin North Am 59:1013–1026
Fleiss JL, Shrout PE (1978) Approximate interval estimation for a certain intraclass correlation coefficient. Psychometrika 43:259–262
Sabharwal S, Zhao C, McKeon J et al (2007) Reliability analysis for radiographic measurement of limb length discrepancy: full-length standing anteroposterior radiograph versus scanogram. J Pediatr Orthop 27:46–50
Funding
This work was supported by a grant from Withhealthcare Co. (Seoul, South Korea).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
247_2022_5499_MOESM1_ESM.png
Supplementary file1 Online Supplementary Material 1 Classification of the failure cases and examples of each. Among the 300 cases, there were a total 16 failure cases (5%). Bowel gas (five cases), skin fold (four cases) and artifact (three cases) were mistakenly taken to represent the iliac crests. The iliac crest was not recognized in 4 cases. a A telegoentgenogram in a 12-year-old boy demonstrates bowel gas as iliac crest. b A Telegoentgenogram in a 14-year-old girl shows a skin fold erroneously identified as the iliac crest. c A teleroentgenogram in a 15-year-old girl demonstrates artifact erroneously identified as iliac crest. d A teleroentgenogram in a 14-year-old boy demonstrates an unrecognized iliac crest (PNG 515 KB)
247_2022_5499_MOESM5_ESM.png
Supplementary file5 Online Supplementary Material 2 Success and failure in the deep-learning measurement. Teleroentgenograms in (a) a 15-year-old boy and (b) a 13-year-old boy. In a successful case (a), the deep-learning algorithm recognized the bilateral iliac crests and measured leg length discrepancy by calculating height difference (black arrow) between the highest points of the recognized bilateral iliac crests (white dotted line). On the other hand, in (b), the deep-learning algorithm failed to recognize correct iliac crest contour and measured height difference (white arrow) between the highest points of the recognized contour (white dotted line). The correct leg length discrepancy is the height difference between the upper white dotted line and the black dotted line (black arrow) (PNG 943 KB)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, M.J., Choi, Y.H., Lee, S.B. et al. Development and evaluation of deep-learning measurement of leg length discrepancy: bilateral iliac crest height difference measurement. Pediatr Radiol 52, 2197–2205 (2022). https://doi.org/10.1007/s00247-022-05499-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-022-05499-0