Abstract
Background
Endovascular stent reconstruction is the standard of care for chronic venous occlusive disease in adults, but it has not been reported in pediatric patients.
Objective
This study reports the technical success, complications, clinical outcomes, and stent patency of iliocaval stent reconstruction for chronic iliocaval thrombosis in pediatric patients.
Materials and methods
Fourteen patients, 13 (93%) male with a mean age of 16.4 years (range: 8–20 years), underwent iliocaval stent reconstruction for chronic iliocaval thrombosis. The mean number of prothrombotic risk factors was 2.5 (range: 0–4), including 7 (50%) patients with inferior vena cava atresia. At initial presentation, the Clinical, Etiology, Anatomy, and Pathophysiology classification (CEAP) score was C3 in 2 (14%) patients, C4 in 11 (79%) patients, and C6 in 1 (7.1%) patient. Time course of presenting symptoms included chronic (>4 weeks) (n=7; 50%) and acute worsening of chronic symptoms (2–4 weeks) (n=7; 50%). Aspects of recanalization and reconstruction, stenting technical success, complications, clinical outcomes and stent patency were recorded. Clinical success was defined as a 1-point decrease in the CEAP. Primary, primary-assisted, and secondary patency were defined by Cardiovascular and Interventional Radiological Society of Europe guidelines.
Results
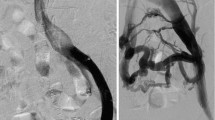
Most procedures employed three access sites (range: 2–4). Intravascular ultrasound was employed in 11 (79%) procedures. Blunt and sharp recanalization techniques were used in 12 (86%) and 2 (14%) patients, respectively. Stenting technical success was 100%. Two (14%) minor adverse events occurred and mean post-procedure hospitalization was 2.8 days (range: 1–8 days). Clinical success rates at 2 weeks, 6 months and 12 months were 85%, 82%, and 83%, respectively. At a mean final clinical follow-up of 88 months (range: 16–231 months), clinical success was 93%. Estimated 6- and 12-month primary stent patencies were 86% and 64%, respectively. Six- and 12-month primary-assisted and secondary stent patency rates were both 100%.
Conclusion
Iliocaval stent reconstruction is an effective treatment for symptomatic chronic iliocaval thrombosis in pediatric patients with high rates of technical success, 6- and 12-month clinical success, and 6- and 12-month primary-assisted and secondary patency rates.





Similar content being viewed by others
References
Eifert S, Villavicencio JL, Kao TC et al (2000) Prevalence of deep venous anomalies in congenital vascular malformations of venous predominance. J Vasc Surg 31:462–471
Koc Z, Oguzkurt L (2007) Interruption or congenital stenosis of the inferior vena cava: prevalence, imaging, and clinical findings. Eur J Radiol 62:257–266
Broholm R, Jørgensen M, Just S et al (2011) Acute iliofemoral venous thrombosis in patients with atresia of the inferior vena cava can be treated successfully with catheter-directed thrombolysis. J Vasc Interv Radiol 22:801–805
Chick JFB, Jo A, Meadows JM et al (2017) Endovascular iliocaval stent reconstruction for inferior vena cava filter-associated iliocaval thrombosis: approach, technical success, safety, and two-year outcomes in 120 patients. J Vasc Interv Radiol 28:933–939
Neglén P, Darcey R, Olivier J, Raju S (2010) Bilateral stenting at the iliocaval confluence. J Vasc Surg 51:1457–1466
Neglén P, Hollis KC, Olivier J, Raju S (2007) Stenting of the venous outflow in chronic venous disease: long-term stent-related outcome, clinical, and hemodynamic result. J Vasc Surg 46:979–990
Ganguli S, Kalva S, Oklu R et al (2012) Efficacy of lower-extremity venous thrombolysis in the setting of congenital absence or atresia of the inferior vena cava. Cardiovasc Intervent Radiol 35:1053–1058
Rogers A, Moloney MA, O'Donnell DH et al (2010) Deep venous thrombosis in a patient with atresia of the infrarenal inferior vena cava. J Vasc Interv Radiol 21:754–756
Oguzkurt L, Ozkan U, Tercan F, Koc Z (2007) Catheter-directed thrombolysis of acute deep vein thrombosis in the lower extremity of a child with interrupted inferior vena cava. Cardiovasc Intervent Radiol 30:332–334
Goldman RE, Arendt VA, Kothary N et al (2017) Endovascular management of May-Thurner syndrome in adolescents: a single-center experience. J Vasc Interv Radiol 28:71–77
Gaballah M, Shi J, Kukreja K et al (2016) Endovascular thrombolysis in the management of iliofemoral thrombosis in children: a multi-institutional experience. J Vasc Interv Radiol 27:524–530
Goldenberg NA, Branchford B, Wang M et al (2011) Percutaneous mechanical and pharmacomechanical thrombolysis for occlusive deep vein thrombosis of the proximal limb in adolescent subjects: findings from an institution-based prospective inception cohort study of pediatric venous thromboembolism. J Vasc Interv Radiol 22:121–132
Dougherty MJ, Calligaro KD, DeLaurentis DA (1996) Congenitally absent inferior vena cava presenting in adulthood with venous stasis and ulceration: a surgically treated case. J Vasc Surg 23:141–146
Tofigh AM, Coscas R, Koskas F, Kieffer E (2008) Surgical management of deep venous insufficiency caused by congenital absence of the infrarenal inferior vena cava. Vasc Endovasc Surg 42:58–61
Dean SM, Tytle TL (2006) Acute right lower extremity iliofemoral deep venous thrombosis secondary to an anomalous inferior vena cava: a report of two cases. Vasc Med 11:165–169
Hanauer DA, Mei Q, Law J et al (2015) Supporting information retrieval from electronic health records: a report of University of Michigan’s nine-year experience in developing and using the electronic medical record search engine (EMERSE). J Biomed Inform 55:290–300
Williams DM (2014) Iliocaval reconstruction in chronic deep vein thrombosis. Tech Vasc Interv Radiol 17:109–113
Bjarnason H, Kruse JR, Asinger DA et al (1997) Iliofemoral deep venous thrombosis: safety and efficacy outcome during 5 years of catheter-directed thrombolytic therapy. J Vasc Interv Radiol 8:405–418
Hartung O, Loundou AD, Barthelemy P et al (2009) Endovascular management of chronic disabling Ilio-caval obstructive lesions: long-term results. Eur J Vasc Endovasc Surg 38:118–124
Vedantham S, Sista AK, Klein SJ et al (2014) Quality improvement guidelines for the treatment of lower-extremity deep vein thrombosis with use of endovascular thrombus removal. J Vasc Interv Radiol 25:1317–1325
Hage AN, Srinivasa RN, Abramowitz SD et al (2018) Endovascular iliocaval reconstruction for the treatment of iliocaval thrombosis: from imaging to intervention. Vasc Med 23:267–275
Chick JFB, Srinivasa RN, Cooper KJ et al (2018) Endovascular iliocaval reconstruction for chronic iliocaval thrombosis: the data, where we are, and how it is done. Tech Vasc Interv Radiol 21:92–104
Raju S, Hollis K, Neglen P (2006) Obstructive lesions of the inferior vena cava: clinical features and endovenous treatment. J Vasc Surg 44:820–827
Monagle P, Chan AKC, Goldenberg NA et al (2012) Antithrombotic therapy in neonates and children: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 Suppl):e737S–e801S
Vedantham S, Thorpe PE, Cardella JF et al (2009) Quality improvement guidelines for the treatment of lower extremity deep vein thrombosis with use of endovascular thrombus removal. J Vasc Interv Radiol 20:S227–S239
Mahnken AH, Thomson K, de Haan M, O’Sullivan GJ (2014) CIRSE standards of practice guidelines on iliocaval stenting. Cardiovasc Intervent Radiol 37:889–897
Khalilzadeh O, Baerlocher MO, Shyn PB et al (2017) Proposal of a new adverse event classification by the Society of Interventional Radiology Standards of practice committee. J Vasc Interv Radiol 28 e1433:1432–1437
Eklöf B, Rutherford RB, Bergan JJ et al (2004) Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg 40:1248–1252
Bakken AM, Protack CD, Saad WE et al (2007) Long-term outcomes of primary angioplasty and primary stenting of central venous stenosis in hemodialysis patients. J Vasc Surg 45:776–783
Chee YL, Culligan DJ, Watson HG (2001) Inferior vena cava malformation as a risk factor for deep venous thrombosis in the young. Br J Haematol 114:878–880
Ramanathan T, Hughes TM, Richardson AJ (2001) Perinatal inferior vena cava thrombosis and absence of the infrarenal inferior vena cava. J Vasc Surg 33:1097–1099
Lambert M, Marboeuf P, Midulla M et al (2010) Inferior vena cava agenesis and deep vein thrombosis: 10 patients and review of the literature. Vasc Med 15:451–459
Malaki M, Willis AP, Jones RG (2012) Congenital anomalies of the inferior vena cava. Clin Radiol 67:165–171
Sandoval JA, Sheehan MP, Stonerock CE et al (2008) Incidence, risk factors, and treatment patterns for deep venous thrombosis in hospitalized children: an increasing population at risk. J Vasc Surg 47:837–843
Vedantham S, Vesely TM, Parti N et al (2003) Endovascular recanalization of the thrombosed filter-bearing inferior vena cava. J Vasc Interv Radiol 14:893–903
Neglén P, Oglesbee M, Olivier J, Raju S (2011) Stenting of chronically obstructed inferior vena cava filters. J Vasc Surg 54:153–161
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
McDevitt, J.L., Srinivasa, R.N., Hage, A.N. et al. Lower extremity endovenous reconstruction for symptomatic occlusive disease in pediatric patients: techniques, clinical outcomes, and long-term stent patencies. Pediatr Radiol 49, 808–818 (2019). https://doi.org/10.1007/s00247-019-04357-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-019-04357-w