Abstract
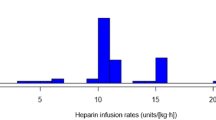
Heparin is used to decrease the risk of thromboembolic complications during electrophysiology studies (EPS); however, there is wide practice variation and minimal evidence to guide heparin dosing, particularly in pediatric patients. This study retrospectively analyzed heparin dosing and response, measured via activated clotting time (ACT), in patients undergoing EPS and used these data (pre-protocol cohort, n = 40), as well as guidance from available literature to implement a standardized heparin protocol (phase 1, n = 43). We utilized quality improvement methodology to refine this protocol (phase 2, n = 40) to improve therapeutic heparin response. Prior to the protocol, patients achieved therapeutic ACT levels (250–350 s) only 35% of the time which improved to 60% during phase 1 (p < 0.05) and to 73% during phase 2 (p < 0.001 compared to pre-protocol). There were no thromboses or significant adverse events in any group. These results demonstrate the effectiveness of a standardized heparin protocol in achieving effective antithrombotic therapy during left-sided pediatric EPS.


Similar content being viewed by others
References
Blanc JJ, Almendral J, Brignole M, Fatemi M, Gjesdal K, Gonzalez-Torrecilla E, Kulakowski P, Lip GYH, Shah D, Wolpert C (2008) Consensus document on antithrombotic therapy in the setting of electrophysiological procedures. Europace 10(5):513–527
Bae EJ, Ban JE, Lee JJ et al (2005) Pediatric radiofrequency catheter ablation: results of initial 100 consecutive cases including congenital heart anomalies. J Korean Med Sci 20(5):740
Miga DE, McKellar LF, Denslow S et al (1997) Incidence of femoral vein occlusion after catheter ablation in children: evaluation with magnetic resonance angiography. Pediatr Cardiol 18(3):204–207
Lee SJ, Schueller WC (2000) Tachycardias in infants, children and adolescents: safety and effectiveness of radiofrequency catheter ablation. Cardiology 94(1):44–51
Jiang H, Li X-M, Li Y-H et al (2016) Efficacy and safety of radiofrequency catheter ablation of tachyarrhythmias in 123 children under 3 years of age. PACE Pacing Clin Electrophysiol 39(8):792–796
Calkins H, Hindricks G et al (2017) 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm 14(10):e275–e444
Boris JRHM (2003) The use of anticoagulation in pediatric cardiac disease. Images Paediatr Cardiol 5(3):1–35
Grady RM, Eisenberg PR, Bridges ND (1995) Rational approach to use of heparin during cardiac catheterization in children. J Am Coll Cardiol 25(3):725–729
Freed MD, Keane JF, Rosenthal A (1974) The use of heparinization to prevent arterial thrombosis after percutaneous cardiac catheterization in children. Circulation 50(3):565–569
Saxena A, Gupta RK, Raman K et al (1997) Predictors of arterial thrombosis after diagnostic cardiac catheterization in infants and children randomized to two heparin dosages. Cathet Cardiovasc Diagn 41(4):400–403
Kim GG, El Rouby S, Thompson J et al (2010) Monitoring unfractionated heparin in pediatric patients with congenital heart disease having cardiac catheterization or cardiac surgery. J Thromb Thrombolysis 29(4):429–436
Dieks JK, Müller MJ, Schneider HE et al (2016) Catheter ablation of pediatric focal atrial tachycardia: ten-year experience using modern mapping systems. Pediatr Cardiol 37(3):459–464
Hafez M, Abu-Elkheir M, Shokier M et al (2012) Radiofrequency catheter ablation in children with supraventricular tachycardias: intermediate term follow up results. Clin Med Insights Cardiol 6:7–16
Woolf P, Sorbera C, Cohen M (2000) Pediatric radiofrequency ablation for tachyarrhythmias: the Westchester Medical Center experience. Heart Dis 2:336–339
Seslar S, Dubin A, Bradley D et al (2017) What have we learned in the last 20 years? A comparison of modern and early era pediatric and congenital catheter ablation registries [abstract] in: heart Rhythm scientific sessions. Chicago; abstract C-AB37-01.
Thakur RK, Klein GJ, Yee R, Zardini M (1994) Embolic complications after radiofrequency catheter ablation. Am J Cardiol 74(3):278–279
de Swart CA, Nijmeyer B, Roelofs JM, Sixma JJ (1982) Kinetics of intravenously administered heparin in normal humans. Blood 60(6):1251–1258
Garcia DA, Baglin TP, Weitz JI, Samama MM (2012) Parenteral anticoagulants: antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest 141(2):e24S–e43S
Monagle P, Chan AKC, Goldenberg NA et al (2012) Antithrombotic therapy in neonates and children: antithrombotic therapy and prevention of thrombosis, 9th ed: American college of CHEST physicians evidence-based clinical practice guidelines. Chest 141(2):e737S–e801S
Bjornsson TD, Wolfram KM, Kitchell BB (1982) Heparin kinetics determined by three assay methods. Clin Pharmacol Ther 31(1):104–113
Newall F, Ignjatovic V, Monagle P, Johnston L (2009) Unfractionated heparin therapy in infants and children. Pediatrics 123(3):e510–e518
Andrew M, Marzinotto V, Massicotte P et al (1994) Heparin therapy in pediatric patients: a prospective cohort study. Pediatr Res 35(1):78–83
Enriquez AD, Churchill T, Gautam S et al (2017) Determinants of heparin dosing and complications in patients undergoing left atrial ablation on uninterrupted rivaroxaban. PACE 40(2):183–190
Ren J-f, Marchlinski FE, Callans DJ et al (2005) Increased intensity of anticoagulation may reduce risk of thrombus during atrial fibrillation ablation procedures in patients with spontaneous ECHO contrast. J Cardiovasc Electrophysiol 16(5):474–477
Moffett BS, Teruya J, Petit C (2011) Heparin dosing in obese pediatric patients in the cardiac catheterization laboratory. Ann Pharmacother 45(7–8):7–8
Avila ML, Shah PS, Brandão LR (2014) Different unfractionated heparin doses for preventing arterial thrombosis in children undergoing cardiac catheterization. Cochrane Database Syst Rev 2014(3):CD010196
Kohn LT (2009) Institute of Medicine. Committee on Quality of Health Care in America. In: To err is human: building a safer health system. National Academy Press, Washington, DC
Hanslik A, Kitzmuller E, Thom K et al (2015) Monitoring unfractionated heparin in children: a parallel-cohort randomized controlled trial comparing 2 dose protocols. Blood 126(18):2091–2097
Ignjatovic V, Furmedge J, Newall F et al (2006) Age-related differences in heparin response. Thromb Res 118(6):741–745
Moore E, Armatage A, Keylon J et al (2017) Assessing use of pain medication after pediatric Cardiac catheterizations. Pediatr Nurs 43(4):163–168
Hanslik A, Kitzmüller E, Thom K et al (2011) Incidence of thrombotic and bleeding complications during cardiac catheterization in children: comparison of high-dose vs. low-dose heparin protocols. JTH 9(12):2353–2360
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have a conflict of interest or relevant relationship with industry.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Seattle Children’s Hospital IRB approved the human research conducted in this study. Formal consent was not required.
Rights and permissions
About this article
Cite this article
Moore, E.F., Pak, J., Jefferis-Kirk, C. et al. Development and Implementation of a Standardized Heparin Protocol for Left-Sided Pediatric Electrophysiology Procedures. Pediatr Cardiol 39, 941–947 (2018). https://doi.org/10.1007/s00246-018-1843-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-018-1843-6