Abstract
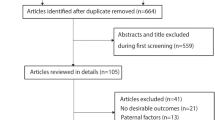
Epidemiological studies have reported conflicting results on the association of congenital heart defect (CHD) risk in offspring with a maternal history of prior pregnancies and abortions, but no meta-analysis has been reported. We searched MEDLINE and EMBASE from their inception to April 14, 2014, for relevant studies that assessed the association between maternal reproductive history and CHD risk. Two authors independently assessed eligibility and extracted data. Fixed-effects or random-effects models were used to calculate the pooled odds ratios (ORs). Among 1,599 references, 17 case–control studies and one nested case–control study were included in this meta-analysis. The summary OR for the ever versus nulligravidity was 1.18 (95 % CI 1.03–1.34). A dose–response analysis also indicated a positive effect of maternal gravidity on CHD risk, and the summary OR for each increment in number of pregnancies was 1.13 (95 % CI 1.08–1.18). A history of abortion was associated with a 24 % higher risk of CHD, OR = 1.24 (95 % CI 1.11–1.38). When stratified by abortion category, CHD risk increased by 18 and 58 % with a history of spontaneous abortion and induced abortion, respectively. The summary OR for each increment of one abortion was 1.28 (95 % CI 1.18–1.40). In summary, this study provides evidence that increased maternal gravidity was positively associated with a risk of CHDs in offspring. Meanwhile, our results demonstrate a positive association of any history of abortion with an increased risk of CHDs.





Similar content being viewed by others
References
Baardman ME, Kerstjens-Frederikse WS, Corpeleijn E, de Walle HE, Hofstra RM, Berger RM, Bakker MK (2012) Combined adverse effects of maternal smoking and high body mass index on heart development in offspring: evidence for interaction? Heart 98:474–479
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Bernstein L, Depue RH, Ross RK, Judd HL, Pike MC, Henderson BE (1986) Higher maternal levels of free estradiol in first compared to second pregnancy: early gestational differences. J Natl Cancer Inst 76:1035–1039
Bhattacharya S, Townend J, Shetty A, Campbell D, Bhattacharya S (2008) Does miscarriage in an initial pregnancy lead to adverse obstetric and perinatal outcomes in the next continuing pregnancy? BJOG 115:1623–1629
Bianca S, Ettore G (2002) Maternal reproductive history and isolated hypoplastic left heart syndrome. Acta Cardiol 57:407–408
Bianca S, Bianca M, Bonaffini F, Ettore G (2002) The role of maternal reproductive history in the aetiology of neural tube defects. Med Hypotheses 58:113–114
Boneva RS, Moore CA, Botto L, Wong LY, Erickson JD (1999) Nausea during pregnancy and congenital heart defects: a population-based case-control study. Am J Epidemiol 149:717–725
Brentlinger PE (2001) Folic acid antagonists during pregnancy and risk of birth defects. N Engl J Med 344:933–934 author reply 934–935
Cai GJ, Sun XX, Zhang L, Hong Q (2014) Association between maternal body mass index and congenital heart defects in offspring: a systematic review. Am J Obstet Gynecol 211:91–117
Cedergren MI, Selbing AJ, Kallen BA (2002) Risk factors for cardiovascular malformation—a study based on prospectively collected data. Scand J Work Environ Health 28:12–17
Celik N, Evsen MS, Sak ME, Soydinc E, Gul T (2011) Evaluation of the relationship between insulin resistance and recurrent pregnancy loss. Ginekol Pol 82:272–275
Chubak J, Tworoger SS, Yasui Y, Ulrich CM, Stanczyk FZ, McTiernan A (2004) Associations between reproductive and menstrual factors and postmenopausal sex hormone concentrations. Cancer Epidemiol Biomarkers Prev 13:1296–1301
Czeizel AE, Dudas I, Vereczkey A, Banhidy F (2013) Folate deficiency and folic acid supplementation: the prevention of neural-tube defects and congenital heart defects. Nutrients 5:4760–4775
Doria-Rose VP, Kim HS, Augustine ET, Edwards KL (2003) Parity and the risk of Down’s syndrome. Am J Epidemiol 158:503–508
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Everett C (1997) Incidence and outcome of bleeding before the 20th week of pregnancy: prospective study from general practice. BMJ 315:32–34
Gibson S, Lewis KC (1952) Congenital heart disease following maternal rubella during pregnancy. AMA J Dis Child 83:317–319
Greenland S, Longnecker MP (1992) Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol 135:1301–1309
Grewal J, Carmichael SL, Ma C, Lammer EJ, Shaw GM (2008) Maternal periconceptional smoking and alcohol consumption and risk for select congenital anomalies. Birth Defects Res A 82:519–526
Grisaru-Granovsky S, Gordon ES, Haklai Z, Samueloff A, Schimmel MM (2009) Effect of interpregnancy interval on adverse perinatal outcomes—a national study. Contraception 80:512–518
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Hoffman JI, Kaplan S (2002) The incidence of congenital heart disease. J Am Coll Cardiol 39:1890–1900
Jenkins KJ, Correa A, Feinstein JA, Botto L, Britt AE, Daniels SR, Elixson M, Warnes CA, Webb CL, American Heart Association Council on Cardiovascular Disease in the Young (2007) Noninherited risk factors and congenital cardiovascular defects: current knowledge: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young: endorsed by the American Academy of Pediatrics. Circulation 115:2995–3014
Jovanovic L, Knopp RH, Kim H, Cefalu WT, Zhu XD, Lee YJ, Simpson JL, Mills JL (2005) Elevated pregnancy losses at high and low extremes of maternal glucose in early normal and diabetic pregnancy: evidence for a protective adaptation in diabetes. Diabetes Care 28:1113–1117
Liu S, Liu J, Tang J, Ji J, Chen J, Liu C (2009) Environmental risk factors for congenital heart disease in the Shandong Peninsula, China: a hospital-based case-control study. J Epidemiol 19:122–130
Loffredo CA, Wilson PD, Ferencz C (2001) Maternal diabetes: an independent risk factor for major cardiovascular malformations with increased mortality of affected infants. Teratology 64:98–106
Long J, Ramadhani T, Mitchell LE (2010) Epidemiology of nonsyndromic conotruncal heart defects in Texas, 1999-2004. Birth Defects Res A 88:971–979
Materna-Kiryluk A, Wieckowska B, Wisniewska K, Borszews-Kakornacka MK, Godula-Stuglik U, Limon J, Rusin J, Sawulicka-Oleszczuk H, Szwalkiewicz-Warowicka E, Walczak M, Members of PWG (2011) Maternal reproductive history and the risk of isolated congenital malformations. Paediatr Perinat Epidemiol 25:135–143
Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D (2012) Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol 175:66–73
Padula AM, Tager IB, Carmichael SL, Hammond SK, Yang W, Lurmann F, Shaw GM (2013) Ambient air pollution and traffic exposures and congenital heart defects in the San Joaquin Valley of California. Paediatr Perinat Epidemiol 27:329–339
Petrescu A, Berdan G, Hulea I, Gaitanidis R, Ambert V, Jinga V, Damian D, Codreanu O, Andrei F, Niculescu L (2007) Small cell carcinoma of the urinary bladder—a new case report. Rom J Morphol Embryol 48:309–314
Pierpont ME, Basson CT, Benson DW Jr, Gelb BD, Giglia TM, Goldmuntz E, McGee G, Sable CA, Srivastava D, Webb CL, American Heart Association Congenital Cardiac Defects Committee CoCDitY (2007) Genetic basis for congenital heart defects: current knowledge: a scientific statement from the American Heart Association Congenital Cardiac Defects Committee, Council on Cardiovascular Disease in the Young: endorsed by the American Academy of Pediatrics. Circulation 115:3015–3038
Pradat P (1992) A case-control study of major congenital heart defects in Sweden—1981-1986. Eur J Epidemiol 8:789–796
Rivas F, Davalos IP, Olivares N, Davalos NO, Perez-Medina R, Gomez-Partida G, Chakraborty R (2000) Reproductive history in mothers of children with neural tube defects. Gynecol Obstet Invest 49:255–260
Rosenquist TH, Ratashak SA, Selhub J (1996) Homocysteine induces congenital defects of the heart and neural tube: effect of folic acid. Proc Natl Acad Sci USA 93:15227–15232
Rovas L, Sladkevicius P, Strobel E, Valentin L (2006) Reference data representative of normal findings at three-dimensional power Doppler ultrasound examination of the cervix from 17 to 41 gestational weeks. Ultrasound Obstet Gynecol 28:761–767
Rushton DI (1978) Simplified classification of spontaneous abortions. J Med Genet 15:1–9
Sheiner E, Katz M, Fraser D, Gohar J, Carmi R (1998) The relationship between congenital cardiovascular malformations and spontaneous abortion in preceding pregnancy. Paediatr Perinat Epidemiol 12:128–135
Steinberger EK, Ferencz C, Loffredo CA (2002) Infants with single ventricle: a population-based epidemiological study. Teratology 65:106–115
Stoll C, Alembik Y, Roth MP, Dott B, De Geeter B (1989) Risk factors in congenital heart disease. Eur J Epidemiol 5:382–391
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283:2008–2012
Stuckey D (1956) Congenital heart defects following maternal rubella during pregnancy. Br Heart J 18:519–522
Tian L, Shen H, Lu Q, Norman RJ, Wang J (2007) Insulin resistance increases the risk of spontaneous abortion after assisted reproduction technology treatment. J Clin Transl Endocrinol Metab 92:1430–1433
Tikkanen J, Heinonen OP (1992) Congenital heart disease in the offspring and maternal habits and home exposures during pregnancy. Teratology 46:447–454
van der Bom T, Zomer AC, Zwinderman AH, Meijboom FJ, Bouma BJ, Mulder BJ (2011) The changing epidemiology of congenital heart disease. Nat Rev Cardiol 8:50–60
Vereczkey A, Kosa Z, Csaky-Szunyogh M, Urban R, Czeizel AE (2012) Birth outcomes of cases with left-sided obstructive defects of the heart in the function of maternal socio-demographic factors: a population-based case-control study. J Matern Fetal Neonatal Med 25:2536–2541
Vereczkey A, Kosa Z, Csaky-Szunyogh M, Czeizel AE (2013) Isolated atrioventricular canal defects: birth outcomes and risk factors: a population-based Hungarian case-control study, 1980-1996. Birth Defects Res A 97:217–224
Wang X, Chen C, Wang L, Chen D, Guang W, French J (2003) Conception, early pregnancy loss, and time to clinical pregnancy: a population-based prospective study. Fertil Steril 79:577–584
Wasserman CR, Shaw GM, O’Malley CD, Tolarova MM, Lammer EJ (1996) Parental cigarette smoking and risk for congenital anomalies of the heart, neural tube, or limb. Teratology 53:261–267
Wells GA, Shea B, OConnell D, Welch V (2013) The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses.comparison. Available from: http://www.ohrica/programs/clinical_epidemiology/oxfordasp. Accessed 3 May 2013:
Williams LJ, Correa A, Rasmussen S (2004) Maternal lifestyle factors and risk for ventricular septal defects. Birth Defects Res A 70:59–64
Woolf B (1955) On estimating the relation between blood group and disease. Ann Hum Genet 19:251–253
Zhu JL, Olsen J, Sorensen HT, Li J, Nohr EA, Obel C, Vestergaard M, Olsen MS (2013) Prenatal maternal bereavement and congenital heart defects in offspring: a registry-based study. Pediatrics 131:e1225–e1230
Author information
Authors and Affiliations
Corresponding author
Additional information
Yu Feng and Song Wang have contributed equally to this work and should be considered co-first authors.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Feng, Y., Wang, S., Zhao, L. et al. Maternal Reproductive History and the Risk of Congenital Heart Defects in Offspring: A Systematic Review and Meta-analysis. Pediatr Cardiol 36, 253–263 (2015). https://doi.org/10.1007/s00246-014-1079-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-014-1079-z