Abstract
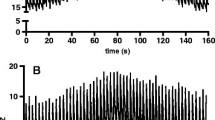
Electrical impedance tomography (EIT) is a noninvasive method to monitor regional lung ventilation in infants and children without using radiation. The objective of this prospective study was to determine the value of EIT as an additional monitoring tool to assess regional lung ventilation after pediatric cardiac surgery for congenital heart disease in infants and children. EIT monitoring was performed in a prospective study comprising 30 pediatric patients who were mechanically ventilated after cardiac surgery. Data were analyzed off-line with respect to regional lung ventilation in different clinical situations. EIT data were correlated with respirator settings and arterial carbon dioxide (CO2) partial pressure in the blood. In 29 of 30 patients, regional ventilation of the lung could sufficiently and reliably be monitored by means of EIT. The effects of the transition from mechanical ventilation to spontaneous breathing after extubation on regional lung ventilation were studied. After extubation, a significant decrease of relative impedance changes was evident. In addition, a negative correlation of arterial CO2 partial pressure and relative impedance changes could be shown. EIT was sufficient to discriminate differences of regional lung ventilation in children and adolescents after cardiac surgery. EIT reliably provided additional information on regional lung ventilation in children after cardiac surgery. Neither chest tubes nor pacemaker wires nor the intensive care unit environment interfered with the application of EIT. EIT therefore may be used as an additional real-time monitoring tool in pediatric cardiac intensive care because it is noninvasive.




Similar content being viewed by others
References
Barber DC (1989) A review of image reconstruction techniques for electrical impedance tomography. Med Phys 16:162–169
Bellani G, Mauri T, Pesenti A (2012) Imaging in acute lung injury and acute respiratory distress syndrome. Curr Opin Crit Care 18:29–34
Bikker IG, Leonhardt S, Bakker J, Gommers D (2009) Lung volume calculated from electrical impedance tomography in ICU patients at different PEEP levels. Intensive Care Med 35:1362–1367
Bikker IG, Leonhardt S, Reis Miranda D, Bakker J, Gommers D (2010) Bedside measurement of changes in lung impedance to monitor alveolar ventilation in dependent and non-dependent parts by electrical impedance tomography during a positive end-expiratory pressure trial in mechanically ventilated intensive care unit patients. Crit Care 14:R100
Bikker IG, Preis C, Egal M, Bakker J, Gommers D (2011) Electrical impedance tomography measured at two thoracic levels can visualize the ventilation distribution changes at the bedside during a decremental positive end-expiratory lung pressure trial. Crit Care 15:R193
Brown BH (2003) Electrical impedance tomography (EIT): a review. J Med Eng Technol 27:97–108
Corley A, Caruana LR, Barnett AG, Tronstad O, Fraser JF (2011) Oxygen delivery through high-flow nasal cannulae increase end-expiratory lung volume and reduce respiratory rate in post-cardiac surgical patients. Br J Anaesth 107:998–1004
Frerichs I (2000) Electrical impedance tomography (EIT) in applications related to lung and ventilation: a review of experimental and clinical activities. Physiol Meas 21:R1–R21
Frerichs I, Schiffmann H, Hahn G, Hellige G (2001) Non-invasive radiation-free monitoring of regional lung ventilation in critically ill infants. Intensive Care Med 27:1385–1394
Frerichs I, Schiffmann H, Oehler R, Dudykevych T, Hahn G, Hinz J et al (2003) Distribution of lung ventilation in spontaneously breathing neonates lying in different body positions. Intensive Care Med 29:787–794
Frerichs I, Braun P, Dudykevych T, Hahn G, Genee D, Hellige G (2004) Distribution of ventilation in young and elderly adults determined by electrical impedance tomography. Respir Physiol Neurobiol 143:63–75
Hahn G DT, Frerichs I, Thiel F, Hellige G (2002) A high performance electrical impedance tomography (EIT) system for clinical evaluation studies and space application. Paper presented at the 2nd European Medical and Biological Engineering Conference EMBEC’02, Vienna, Austria
Hahn G, Sipinkova I, Baisch F, Hellige G (1995) Changes in the thoracic impedance distribution under different ventilatory conditions. Physiol Meas 16:A161–A173
Hahn G, Thiel F, Dudykevych T, Frerichs I, Gersing E, Schroder T et al (2001) Quantitative evaluation of the performance of different electrical tomography devices. Biomed Tech (Berl) 46:91–95
Heinrich S, Schiffmann H, Frerichs A, Klockgether-Radke A, Frerichs I (2006) Body and head position effects on regional lung ventilation in infants: an electrical impedance tomography study. Intensive Care Med 32:1392–1398
Heinze H, Eichler W, Karsten J, Sedemund-Adib B, Heringlake M, Meier T (2011) Functional residual capacity-guided alveolar recruitment strategy after endotracheal suctioning in cardiac surgery patients. Crit Care Med 39:1042–1049
Hinz J, Neumann P, Dudykevych T, Andersson LG, Wrigge H, Burchardi H et al (2003) Regional ventilation by electrical impedance tomography: a comparison with ventilation scintigraphy in pigs. Chest 124:314–322
Hough JL, Johnston L, Brauer SG, Woodgate PG, Pham TM, Schibler A (2011) Effect of body position on ventilation distribution in preterm infants on continuous positive airway pressure. Pediatr Crit Care Med 13(4):446–451
Humphreys S, Pham TM, Stocker C, Schibler A (2011) The effect of induction of anesthesia and intubation on end-expiratory lung level and regional ventilation distribution in cardiac children. Paediatr Anaesth 21:887–893
Kristjansdottir A, Ragnarsdottir M, Hannesson P, Beck HJ, Torfason B (2004) Respiratory movements are altered 3 months and 1 year following cardiac surgery. Scand Cardiovasc J 38:98–103
Muller NL, Bryan AC (1979) Chest wall mechanics and respiratory muscles in infants. Pediatr Clin North Am 26:503–516
Riedel T, Kyburz M, Latzin P, Thamrin C, Frey U (2009) Regional and overall ventilation inhomogeneities in preterm and term-born infants. Intensive Care Med 35:144–151
Schibler A, Yuill M, Parsley C, Pham T, Gilshenan K, Dakin C (2009) Regional ventilation distribution in non-sedated spontaneously breathing newborns and adults is not different. Pediatr Pulmonol 44:851–858
Serrano RE, Riu PJ, de Lema B, Casan P (2004) Assessment of the unilateral pulmonary function by means of electrical impedance tomography using a reduced electrode set. Physiol Meas 25:803–813
Sharp JT, Druz WS, Balagot RC, Bandelin VR, Danon J (1970) Total respiratory compliance in infants and children. J Appl Physiol 29:775–779
Wolf GK, Arnold JH (2006) Electrical impedance tomography: ready for prime time? Intensive Care Med 32:1290–1292
Wolf GK, Grychtol B, Frerichs I, van Genderingen HR, Zurakowski D, Thompson JE et al (2007) Regional lung volume changes in children with acute respiratory distress syndrome during a derecruitment maneuver. Crit Care Med 35:1972–1978
Zhao Z, Steinmann D, Frerichs I, Guttmann J, Moller K (2010) PEEP titration guided by ventilation homogeneity: a feasibility study using electrical impedance tomography. Crit Care 14:R8
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krause, U., Becker, K., Hahn, G. et al. Monitoring of Regional Lung Ventilation Using Electrical Impedance Tomography After Cardiac Surgery in Infants and Children. Pediatr Cardiol 35, 990–997 (2014). https://doi.org/10.1007/s00246-014-0886-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-014-0886-6