Abstract
Background
Prior studies have suggested that maternal corticosteroids exposure during the first trimester may be associated with an increased risk of congenital heart defects (CHDs) in offspring. However, the findings are discrepant. Moreover, a complete overview of the existing data in the literature is lacking. Our objective was to identify whether such an association exists.
Methods and results
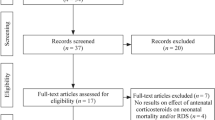
Relevant studies were identified via searching PubMed, Web of Science, Embase, Chinese databases, and the Cochrane Library databases (search date July 15, 2021) and through checking the reference lists of retrieved articles. The overall pooled risk estimate was calculated using random-effect models. We used the GRADE approach to assess the overall strength of the evidence and the Newcastle–Ottawa Scale to assess study quality. Subgroup analyses were performed to evaluate the association within studies or samples with different characteristics. Sensitivity analyses were performed to assess the robustness of the results. Nine studies involving 1,901,599 participants were included in the final analysis. All studies were evaluated as high quality. In the meta-analysis, no statistically significant association was found between maternal corticosteroids exposure during the first trimester and increased risk of CHDs in offspring (OR = 1.06, 95% CI: 1.00–1.13, P = 0.06, low certainty of evidence). Additionally, we also did not find significant differences in subgroup analyses of corticosteroids exposure patterns, including oral corticosteroids exposure (OR = 1.23, 95% CI: 1.00–1.52), ointment corticosteroids exposure (OR = 1.03, 95% CI: 0.90–1.19), inhalation corticosteroids exposure (OR = 1.06, 95% CI: 0.96–1.17), topical corticosteroids or systemic corticosteroids exposure (OR = 0.95, 95% CI: 0.79–1.15), and nasal corticosteroids exposure (OR = 1.12, 95% CI: 0.80–1.57).
Conclusions
Our study does not find an association between maternal corticosteroids exposure during the first trimester and offspring CHDs. However, the existing evidence is of low quality; thus, long-term prospective cohort studies are warranted to verify the safety of corticosteroids in this population, with adequate adjustments for confounding variables.



Similar content being viewed by others
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Change history
22 November 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00228-022-03429-5
Abbreviations
- CHDs:
-
Congenital heart defects
- CI:
-
Confidence interval
- GRADE:
-
The Grading of Recommendations, Assessment, Development, and Evaluations recommendations
- HR:
-
Hazard ratio
- OR:
-
Odds ratio
- PR:
-
Prevalence ratio
- NOS:
-
Newcastle-Ottawa Scale
- RR:
-
Risk ratio
- SLE:
-
Systemic lupus erythematosus
References
Mitchell S, Korones S, Berendes H (1971) Congenital heart disease in 56,109 births. Incidence and natural history Circulation 43(3):323–332
Khoshnood B, Lelong N, Houyel L et al (2012) Prevalence, timing of diagnosis and mortality of newborns with congenital heart defects: a population-based study. Heart (British Cardiac Society) 98(22):1667–1673
van der Linde D, Konings E, Slager M et al (2011) Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol 58(21):2241–2247
Liu Y, Chen S, Zühlke L et al (2019) Global birth prevalence of congenital heart defects 1970–2017: updated systematic review and meta-analysis of 260 studies. Int J Epidemiol 48(2):455–463
Zhao L, Chen L, Yang T et al (2020) Birth prevalence of congenital heart disease in China, 1980–2019: a systematic review and meta-analysis of 617 studies. Eur J Epidemiol 35(7):631–642
Jenkins K, Correa A, Feinstein J et al (2007) Noninherited risk factors and congenital cardiovascular defects: current knowledge: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young: endorsed by the American Academy of Pediatrics. Circulation 115(23):2995–3014
Wilson P, Loffredo C, Correa-Villaseñor A, Ferencz C (1998) Attributable fraction for cardiac malformations. Am J Epidemiol 148(5):414–423
McGee D (2002) Steroid use during pregnancy. J Perinat Neonatal Nurs 16(2):26–39
Bjørn A, Ehrenstein V, Nohr E, Nørgaard M (2015) Use of inhaled and oral corticosteroids in pregnancy and the risk of malformations or miscarriage. Basic Clin Pharmacol Toxicol 116(4):308–314
Irvine L, Flynn R, Libby G, Crombie I, Evans J (2010) Drugs dispensed in primary care during pregnancy: a record-linkage analysis in Tayside. Scotland Drug safety 33(7):593–604
Lacroix I, Damase-Michel C, Lapeyre-Mestre M, Montastruc J (2000) Prescription of drugs during pregnancy in France. Lancet (London, England) 356(9243):1735–1736
Fraser F, Fainstat T (1951) Production of congenital defects in the off-spring of pregnant mice treated with cortisone; progress report. Pediatrics 8(4):527–533
Sahin L, Nallani S, Tassinari M (2016) Medication use in pregnancy and the pregnancy and lactation labeling rule. Clin Pharmacol Ther 100(1):23–25
Liberati A, Altman D, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100
Stroup D, Berlin J, Morton S et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283(15):2008–2012
Guyatt G, Oxman A, Vist G et al (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ (Clinical research ed) 336(7650):924–926
Balshem H, Helfand M, Schünemann H et al (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidem 64(4):401–406
Viera A (2008) Odds ratios and risk ratios: what’s the difference and why does it matter? South Med J 101(7):730–734
Borenstein M, Hedges L, Higgins J, Rothstein H (2010) A basic introduction to fixed-effect and random-effects models for meta-analysis. Research synthesis methods 1(2):97–111
Higgins J, Thompson S (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558
Higgins J, Thompson S, Deeks J, Altman D (2003) Measuring inconsistency in meta-analyses. BMJ (Clinical research ed) 327(7414):557–560
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ (Clinical research ed) 315(7109):629–634
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4):1088–1101
Schmidt AB, Lund M, Corn G, Øyen N, Wohlfahrt J, Melbye M (2019) Oral corticosteroids during pregnancy and offspring risk of congenital heart defects - a nationwide cohort study. Pharmacoepidemiol Drug Saf 28:367
Kallen B, Olausson PO (2007) Use of anti-asthmatic drugs during pregnancy. 3. Congenital malformations in the infants. Europ J Clin Pharma 63(4):383–388
Van Zutphen AR, Bell EM, Browne ML, Lin S, Lin AE, Druschel CM (2015) Maternal asthma medication use during pregnancy and risk of congenital heart defects. Birth Defects Research Part A - Clinical and Molecular Teratology 103(11):951–961
Lin S, Herdt-Losavio M, Gensburg L, Marshall E, Druschel C (2009) Maternal asthma, asthma medication use, and the risk of congenital heart defects. Birth Defects Research Part A - Clinical and Molecular Teratology 85(2):161–168
Garne E, Hansen AV, Morris J et al (2015) Use of asthma medication during pregnancy and risk of specific congenital anomalies: a European case-malformed control study. J Allerg Clin Immun 136(6):1496–1502e1497
Gur C, Diav-Citrin O, Shechtman S, Arnon J, Ornoy A (2004) Pregnancy outcome after first trimester exposure to corticosteroids: a prospective controlled study. Reprod Toxicol Jan-Feb 18(1):93–101
Vasilakis‐Scaramozza C (2013) Asthma drugs and the risk of congenital anomalies. Pharmacotherapy 33(4):363–368
Kallen B (2003) Maternal drug use in early pregnancy and infant cardiovascular defect. Reprod Toxicol 17(3):255–261
Czeizel AE (1997) Population-based case-control study of teratogenic potential of corticosteroids
Queisser-Luft A, Eggers I, Stolz G, Kieninger-Baum D, Schlaefer K (1996) Serial examination of 20,248 newborn fetuses and infants: correlations between drug exposure and major malformations. Am J Med Genet 63(1):268–276
Howley MM, Papadopoulos EA, Van Bennekom CM et al (2020) Asthma medication use and risk of birth defects: National Birth Defects Prevention Study, 1997–2011. J Allerg Clin Immun Prac Nov-Dec 8(10):3490-+
Wollins D, Ferencz C, Boughman J, Loffredo C (2001) A population-based study of coarctation of the aorta: comparisons of infants with and without associated ventricular septal defect. Teratology 64(5):229–236
Zambelli-Weiner A, Via C, Yuen M, Weiner D (2018) Evaluating the relationship between in-utero methylprednisolone exposure and birth defects. Value in Health 21:S142
Vinet É (2015) Increased congenital heart defects in children born to women with systemic lupus erythematosus: results from the offspring of Systemic Lupus Erythematosus Mothers Registry Study. Circulation 131(2):149–156
Tata LJ, Lewis SA, McKeever TM et al (2008) Effect of maternal asthma, exacerbations and asthma medication use on congenital malformations in offspring: a UK population-based study. Thorax 63(11):981–987
Tamasi L, Somoskovi A, Muller V et al (2006) A population-based case-control study on the effect of bronchial asthma during pregnancy for congenital abnormalities of the offspring. J Asthma Jan-Feb 43(1):81–86
Bosco J, Silliman R, Thwin S et al (2010) A most stubborn bias: no adjustment method fully resolves confounding by indication in observational studies. J Clin Epidemiol 63(1):64–74
Ehrenstein V, Sørensen H, Bakketeig L, Pedersen L (2010) Medical databases in studies of drug teratogenicity: methodological issues. Clin Epidemiol 2:37–43
Gao S, Wu Q, Sun C et al (2018) Selective serotonin reuptake inhibitor use during early pregnancy and congenital malformations: a systematic review and meta-analysis of cohort studies of more than 9 million births. BMC Med 16(1):205
Acknowledgements
We thank everyone who has provided advice and help with this article.
Funding
This study was funded by the National Natural Science Foundation Program of China (no. 81973137 and 82173608 to Lizhang Chen) and the Project of Hunan Provincial Maternal and Child Health Care Hospital (2021RX26). The funding bodies had no role in the design of this study, the collection, analysis, and interpretation of the data, or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
Lizhang Chen and Tingting Wang contributed to the conception and study design. Jiehua Wei performed a search strategy and searched the literature. Jiehua Wei, Fang Xia, and Junxiang Miao selected the studies, extracted the data, and analyzed and interpreted the data. Jiehua Wei drafted the manuscript. Lizhang Chen, Xuemei Yan, and Jiehua Wei revised the article critically for important intellectual content and interpreted the results. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Figure 1 in the published proof does not show the complete image.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wei, J., Xia, F., Miao, J. et al. The risk of congenital heart defects associated with corticosteroids use during the first trimester of pregnancy: a systematic review and meta-analysis. Eur J Clin Pharmacol 79, 1–11 (2023). https://doi.org/10.1007/s00228-022-03416-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-022-03416-w