Abstract
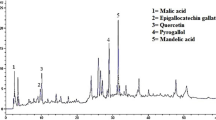
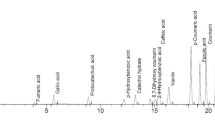
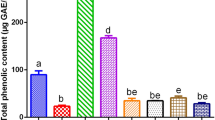
This study was aimed to investigate the phenolic profile of methanolic extract of Trifolium repens L. leaves using LC–HRMS and LC–DAD and its anti--cholinesterase and anti-oxidant activities. The n-Hexane (Tr.Hex), chloroform (Tr.Chf), ethanol (Tr.Et), methanol (Tr.Cme), and aqueous (Tr.Aq) extracts were tested for anti-cholinesterases and anti-oxidant potentials. Twenty-nine phenolic compounds were quantified and identified. The highest amount present were of tyrosol (11.1 mg/g), quercetin-3-glucuronide (5.36 mg/g), formononetin-7-glucoside (5.03 mg/g), quercetin-3-O-glucoside (4.71 mg/g), 3,4-di-O-caffeoylquinic acid (4.69 mg/g), formononetin-7-glucoside-acetate (4.29 mg/g), quercetin-3-O-glucoside (4.26 mg/g), and formononetin (3.64 mg/g). Tr.Chf and Tr.Et were most active against AChE, BChE, and free radicals. Tr.Chf exhibited IC50 of 15 and 21 µg/mL against AChE and BChE, respectively. In the anti-oxidant study, Tr.Chf showed IC50 of 42 and 25 µg/mL against ABTS and DPPH radicals, respectively. The current results of anti-cholinesterase and anti-radical studies on T. repens further signify its potential application in neurodegenerative disorders.
Graphic abstract




Similar content being viewed by others
References
Mattson MP (2004) Pathways towards and away from Alzheimer’s disease. Nature 430(7000):631
Selkoe DJ (1991) The molecular pathology of Alzheimer’s disease. Neuron 6(4):487–498
Barnes DE, Yaffe K (2011) The projected effect of risk factor reduction on Alzheimer’s disease prevalence. Lancet Neurol 10(9):819–828
Ayaz M, Sadiq A, Junaid M, Ullah F, Ovais M, Ullah I, Ahmed J, Shahid M (2019) Flavonoids as prospective neuroprotectants and their therapeutic propensity in aging associated neurological disorders. Front Aging Neurosci 11:155. https://doi.org/10.3389/fnagi.2019.00155
Ovais M, Zia N, Ahmad I, Khalil AT, Raza A, Ayaz M, Sadiq A, Ullah F, Shinwari ZK (2018) Phyto-therapeutic and nanomedicinal approach to cure Alzheimer disease: present status and future opportunities. Front Aging Neurosci 10:284
Ayaz M, Junaid M, Ullah F, Sadiq A, Khan MA, Ahmad W, Shah MR, Imran M, Ahmad S (2015) Comparative chemical profiling, cholinesterase inhibitions and anti-radicals properties of essential oils from Polygonum hydropiper L: a preliminary anti-Alzheimer’s study. Lipids Health Dis 14(1):141
Mimica N, Presečki P (2009) Side effects of approved antidementives. Psychiatria Danubina 21(1):108–113
Arias E, Gallego-Sandín S, Villarroya M, García AG, López MG (2005) Unequal neuroprotection afforded by the acetylcholinesterase inhibitors Galantamine, Donepezil, and Rivastigmine in SH-SY5Y neuroblastoma cells: role of nicotinic receptors. J Pharmacol Exp Ther 315(3):1346–1353. https://doi.org/10.1124/jpet.105.090365
Oh M, Houghton P, Whang W, Cho J (2004) Screening of Korean herbal medicines used to improve cognitive function for anti-cholinesterase activity. Phytomedicine 11(6):544–548
Schulz V (2003) Ginkgo extract or cholinesterase inhibitors in patients with dementia: what clinical trials and guidelines fail to consider. Phytomedicine 10:74–79
Ayaz M, Junaid M, Ullah F, Subhan F, Sadiq A, Ali G, Ovais M, Shahid M, Ahmad A, Wadood A (2017) Anti-Alzheimer’s studies on β-sitosterol isolated from Polygonum hydropiper L. Front Pharmacol 8:697
Atanasov AG, Waltenberger B, Pferschy-Wenzig E-M, Linder T, Wawrosch C, Uhrin P, Temml V, Wang L, Schwaiger S, Heiss EH (2015) Discovery and resupply of pharmacologically active plant-derived natural products: a review. Biotechnol Adv 33(8):1582–1614
Kunnumakkara AB, Bordoloi D, Padmavathi G, Monisha J, Roy NK, Prasad S, Aggarwal BB (2017) Curcumin, the golden nutraceutical: multitargeting for multiple chronic diseases. Br J Pharmacol 174(11):1325–1348
Zoric L, Merkulov L, Lukovic J, Boza P (2012) Comparative analysis of qualitative anatomical characters of Trifolium L. (Fabaceae) and their taxonomic implications: preliminary results. Plant Syst Evol 298(1):205–219
Sakeran MI, Zidan N, Rehman H, Aziz AT, Saggu S (2014) Abrogation by Trifolium alexandrinum root extract on hepatotoxicity induced by acetaminophen in rats. Redox Rep 19(1):26–33
Kolodziejczyk-Czepas J (2016) Trifolium species - the latest findings on chemical profile, ethnomedicinal use and pharmacological properties. J Pharm Pharmacol 68(7):845–861. https://doi.org/10.1111/jphp.12568
Ahmad S, Zeb A (2019) Effects of phenolic compounds from aqueous extract of Trifolium repens against acetaminophen‐induced hepatotoxicity in mice. J Food Biochem 43(9):e12963. https://doi.org/10.1111/jfbc.12963
Chen YH, Chen P, Wang Y, Yang CH, Wu X, Wu CJ, Luo L, Wang Q, Niu C, Yao JY (2019) Structural characterization and anti‐inflammatory activity evaluation of chemical constituents in the extract of Trifolium repens L. J Food Biochem 43(9):e12981. https://doi.org/10.1111/jfbc.12981
Rathee P, Chaudhary H, Rathee S, Rathee D, Kumar V, Kohli K (2009) Mechanism of action of flavonoids as anti-inflammatory agents: a review. Inflamm Allergy-drug Targ 8(3):229–235
Zeb A (2015) A reversed phase HPLC-DAD method for the determination of phenolic compounds in plant leaves. Anal Methods 7(18):7753–7757. https://doi.org/10.1039/C5AY01402F
Ellman GL, Courtney KD, Andres V Jr, Featherstone RM (1961) A new and rapid colorimetric determination of acetylcholinesterase activity. Biochem Pharmacol 7(2):88–95
Ayaz M, Junaid M, Ahmed J, Ullah F, Sadiq A, Ahmad S, Imran M (2014) Phenolic contents, antioxidant and anticholinesterase potentials of crude extract, subsequent fractions and crude saponins from Polygonum hydropiper L. BMC Complement Altern Med 14(1):145
Mukherjee PK, Kumar V, Mal M, Houghton PJ (2007) Acetylcholinesterase inhibitors from plants. Phytomedicine 14(4):289–300
Saklani A, Kutty SK (2008) Plant-derived compounds in clinical trials. Drug Discov Today 13(3–4):161–171
Williams P, Sorribas A, Howes M-JR (2011) Natural products as a source of Alzheimer’s drug leads. Nat Product Rep 28(1):48–77
Saunders D, Poppleton D, Struchkov A, Ireland R (2014) Analysis of five bioactive compounds from naturally occurring Rhodiola rosea in eastern Canada. Can J Plant Sci 94(4):741–748
Giovannini L, Migliori M, Filippi C, Origlia N, Panichi V, Falchi M, Bertelli A, Bertelli A (2002) Inhibitory activity of the white wine compounds, tyrosol and caffeic acid, on lipopolysaccharide-induced tumor necrosis factor-alpha release in human peripheral blood mononuclear cells. Int J Tissue React 24(2):53–56
Bu Y, Rho S, Kim J, Kim MY, Lee DH, Kim SY, Choi H, Kim H (2007) Neuroprotective effect of tyrosol on transient focal cerebral ischemia in rats. Neurosci Lett 414(3):218–221
An L, Guan S, Shi G, Bao Y, Duan Y, Jiang B (2006) Protocatechuic acid from Alpinia oxyphylla against MPP+ -induced neurotoxicity in PC12 cells. Food Chem Toxicol 44(3):436–443
Zhang Z, Li G, Szeto SS, Chong CM, Quan Q, Huang C, Cui W, Guo B, Wang Y, Han Y (2015) Examining the neuroprotective effects of protocatechuic acid and chrysin on in vitro and in vivo models of Parkinson disease. Free Radical Biol Med 84:331–343
Ojha S, Javed H, Azimullah S, Khair SBA, Haque ME (2015) Neuroprotective potential of ferulic acid in the rotenone model of Parkinson’s disease. Drug Des Dev Ther 9:5499
Cheng C-Y, Su S-Y, Tang N-Y, Ho T-Y, Chiang S-Y, Hsieh C-L (2008) Ferulic acid provides neuroprotection against oxidative stress-related apoptosis after cerebral ischemia/reperfusion injury by inhibiting ICAM-1 mRNA expression in rats. Brain Res 1209:136–150
Booth NL, Overk CR, Yao P, Burdette JE, Nikolic D, Chen S-N, Bolton JL, Breemen RB, Pauli GF, Farnsworth NR (2006) The chemical and biologic profile of a red clover (Trifolium pratense L.) phase II clinical extract. J Altern Complement Med 12(2):133–139
Aras AB, Guven M, Akman T, Ozkan A, Sen HM, Duz U, Kalkan Y, Silan C, Cosar M (2015) Neuroprotective effects of daidzein on focal cerebral ischemia injury in rats. Neural Regen Res 10(1):146
Hurtado O, Ballesteros I, Cuartero M, Moraga A, Pradillo J, Ramírez-Franco J, Bartolomé-Martín D, Pascual D, Torres M, Sánchez-Prieto J (2012) Daidzein has neuroprotective effects through ligand-binding-independent PPARγ activation. Neurochem Int 61(1):119–127
Subedi L, Ji E, Shin D, Jin J, Yeo J, Kim S (2017) Equol, a dietary daidzein gut metabolite attenuates microglial activation and potentiates neuroprotection in vitro. Nutrients 9(3):207
Liang K, Ye Y, Wang Y, Zhang J, Li C (2014) Formononetin mediates neuroprotection against cerebral ischemia/reperfusion in rats via downregulation of the Bax/Bcl-2 ratio and upregulation PI3K/Akt signaling pathway. J Neurol Sci 344(1–2):100–104
Fei H-X, Zhang Y-B, Liu T, Zhang X-J, Wu S-L (2018) Neuroprotective effect of formononetin in ameliorating learning and memory impairment in mouse model of Alzheimer’s disease. Biosci Biotechnol Biochem 82(1):57–64
Shahwar D, Rehman SU, Raza MA (2010) Acetyl cholinesterase inhibition potential and antioxidant activities of ferulic acid isolated from Impatiens bicolor Linn. J Med Plants Res 4(3):260–266
Szwajgier D (2013) Anticholinesterase activity of phenolic acids and their derivatives. Zeitschrift für Naturforschung C 68(3–4):125–132
Szwajgier D, Borowiec K (2012) Phenolic acids from malt are efficient acetylcholinesterase and butyrylcholinesterase inhibitors. J Inst Brew 118(1):40–48
Gülçin İ, Scozzafava A, Supuran CT, Koksal Z, Turkan F, Çetinkaya S, Bingöl Z, Huyut Z, Alwasel SH (2016) Rosmarinic acid inhibits some metabolic enzymes including glutathione S-transferase, lactoperoxidase, acetylcholinesterase, butyrylcholinesterase and carbonic anhydrase isoenzymes. J Enzyme Inhib Med Chem 31(6):1698–1702
Kwon S-H, Lee H-K, Kim J-A, Hong S-I, Kim H-C, Jo T-H, Park Y-I, Lee C-K, Kim Y-B, Lee S-Y (2010) Neuroprotective effects of chlorogenic acid on scopolamine-induced amnesia via anti-acetylcholinesterase and anti-oxidative activities in mice. Eur J Pharmacol 649(1–3):210–217
Senorans F, Ibanez E, Cavero S, Tabera J, Reglero G (2000) Liquid chromatographic–mass spectrometric analysis of supercritical-fluid extracts of rosemary plants. J Chromatogr A 870(1–2):491–499
Santos J, Oliveira M, Ibáñez E, Herrero M (2014) Phenolic profile evolution of different ready-to-eat baby-leaf vegetables during storage. J Chromatogr A 1327:118–131
He X-g, Lin L-z, Lian L-z (1996) Analysis of flavonoids from red clover by liquid chromatography—electrospray mass spectrometry. J Chromatogr A 755(1):127–132
Tsao R, Papadopoulos Y, Yang R, Young JC, McRae K (2006) Isoflavone profiles of red clovers and their distribution in different parts harvested at different growing stages. J Agric Food Chem 54(16):5797–5805
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Compliance with ethics requirements
This article does not contain any studies with human participants or animals.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ahmad, S., Zeb, A., Ayaz, M. et al. Characterization of phenolic compounds using UPLC–HRMS and HPLC–DAD and anti-cholinesterase and anti-oxidant activities of Trifolium repens L. leaves. Eur Food Res Technol 246, 485–496 (2020). https://doi.org/10.1007/s00217-019-03416-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00217-019-03416-8