Abstract
Rationale
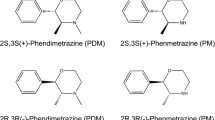
3,4-Methylenedioxymethamphetamine (MDMA, designated as “Ecstasy” if illicitly marketed in tablet form) induces significant decrements in neuronal serotonin (5-HT) markers in humans, nonhuman primates, and rats as a function of dosing and dosing regimen. In rats, MDMA-mediated effects are attributed, in part, to selective high-affinity transport of MDMA into 5-HT neurons by the 5-HT transporter (SERT), followed by extensive 5-HT release.
Objectives
To clarify whether SERT-selective effects of MDMA at human monoamine transporters can account for the reported MDMA-induced selective toxicity of serotonin neurons in primate brain.
Methods
We investigated the interaction of [3H](±, RS)- (+, S)- and (−, R)-MDMA with the human SERT, dopamine (DA) transporter (DAT), and norepinephrine (NE) transporter (NET) in stably transfected human embryo kidney (HEK)-293 cells.
Results
The human DAT, NET, and SERT actively transported [3H]RS(±)-MDMA saturably, stereoselectively, and in a temperature-, concentration-, and transporter-dependent manner. MDMA exhibited the highest affinity for the NET≫SERT≥DAT, the same rank order for MDMA inhibition of [3H]DA, [3H]NE, and [3H]5-HT transport and stimulated release of the [3H]monoamines, which differed from reports derived from rodent monoamine transporters. The extent of MDMA-induced release of 5-HT was higher compared with release of DA or NE.
Conclusions
The affinity of MDMA for the human SERT in transfected cells does not clarify the apparent selective toxicity of MDMA for serotonin neurons, although conceivably, its higher efficacy for stimulating 5-HT release may be a distinguishing factor. The findings highlight the need to investigate MDMA effects in DAT-, SERT-, and NET-expressing neurons in the primate brain and the therapeutic potential of NET or DAT inhibitors, in addition to SERT-selective inhibitors, for alleviating the pharmacological effects of MDMA.
Similar content being viewed by others
Introduction
In the mammalian brain, 3,4-methylenedioxymethamphetamine (MDMA) induces selective decrements in markers of monoamine neurons as a function of dose, dosing regimen, and species (Ricaurte et al. 1988a). These changes can persist for years after the last exposure (Bowyer et al. 2003; Taffe et al. 2002, 2003; Reneman et al. 2002; Hatzidimitriou et al. 1999; Scheffel et al. 1998; Nash and Yamamoto 1992; Slikker et al. 1989). The most consistent and prominent findings in the primate brain are reductions in brain serotonin (5-HT), its major metabolite 5-hydroxyindoleacetic acid (5-HIAA), the 5-HT transporter (SERT), and tryptophan hydroxylase (Ricaurte et al. 1988a,b, 1992). In humans, the 5-HT system is also most notably affected, with reduced cerebrospinal fluid levels of 5-HT and 5-HIAA and reduced SERT binding potential in the brain (Steele et al. 1994; Buchert et al. 2004; McCann et al. 2005). These findings are postulated to reflect MDMA-induced neurotoxicity and to account for the neuropsychological effects of prolonged exposure to MDMA (Parrott 2001). Nevertheless, extrapolation from biochemical markers to neuronal damage or death in humans remains equivocal (Turner and Parrott 2000; Kish 2002; Check 2004). Although MDMA-induced release of serotonin via the SERT is frequently cited as the significant mechanism in MDMA-induced neurotoxicity, this postulate remains controversial. Other underlying causes have been proposed, including carrier-dependent transport of MDMA, metabolic toxic products, oxidative stress, hyperthermia, apoptosis, and increased extracellular concentrations of dopamine (DA) and 5-HT (Simantov and Tauber 1997; Shankaran et al. 1999; Sanchez et al. 2001; Green et al. 2003).
The selective effects of MDMA on 5-HT neurons are species-dependent. Serotonin neurons of the primate brain are more susceptible to MDMA-induced changes when compared to rats (Ricaurte and McCann 1992; Slikker et al. 1988, 1989), whereas in mice, MDMA selectively modifies DA neurons while sparing 5-HT neurons (Logan et al. 1988; O'Callaghan and Miller 1994; Xie et al. 2004). Dose and dosing regimen are another contributing factor to MDMA-induced neurotoxicity, as high doses of MDMA promotes dopaminergic and noradrenergic neurotoxicity in rats (Commins et al. 1987; Mayerhofer et al. 2001). However, the susceptibility of catecholamine neurons to MDMA-induced neurotoxicity is unresolved in primates (Turner and Parrott 2000).
The divergent neurotoxic properties of substituted amphetamines are postulated, among others, to be due to differences in potencies at monoamine transporters (Rudnick and Wall 1992). The serotonin neuron-selective toxicity of MDMA has been attributed to its higher affinity, uptake, or releasing capacity at the SERT, compared with the dopamine transporter (DAT) or norepinephrine (NE) transporter (NET, Rudnick and Wall 1992). This view is supported by data derived from the rodent brain, in which MDMA displays a tenfold higher affinity for blocking SERT-mediated 5-HT transport compared with its affinity for the DAT (Steele et al. 1987; Battaglia et al. 1988). In contrast, amphetamine selectively affects DA neurons, and methamphetamine apparently affects both neuronal subtypes, coinciding with their relative potencies at the three monoamine transporters (see McCann and Ricaurte 2004 for a review).
The conventional hypothesis that MDMA is toxic to serotonin neurons in the human brain because of selective effects at the human SERT has been liberally extrapolated from MDMA inhibition potencies at rodent brain monoamine transporters. Potential species differences, a possible mismatch between inhibition (K i values) and affinity data (K m values), and incomplete evidence that MDMA is a substrate for human monoamine transporters may compromise this extrapolation. To fill this void, we interrogated the influence of MDMA at human monoamine transporters. Foremost, we determined whether the relative potencies of MDMA for inhibiting rodent monoamine transporters extended to human monoamine transporters. Second, we determined directly whether [3H]MDMA is sequestered by cells expressing human monoamine transporters and compared substrate affinities with MDMA potencies for inhibiting human DAT, NET, and SERT. This represents the first direct evidence of DAT-, NET-, and SERT-mediated [3H]MDMA transport into cells and supports the view of MDMA as a substrate based on MDMA-induced ion conductances (Sonders et al. 1997). To further explore the substrate properties of MDMA, we compared MDMA affinities for inhibiting radiolabeled inhibitor binding to the DAT, NET, and SERT with affinities for blocking monoamine transport, as substrates display relatively weak affinities at radioligand binding sites, whereas transport inhibitor potencies at radiolabeled sites usually correspond to their affinities for blocking the transport of monoamines (Madras et al. 1989a,b; Goulet et al. 2001; Eshleman et al. 1995, 1999). Our third objective was to monitor the capacity of MDMA to release sequestered monoamines from transporter-expressing cultured cells, as MDMA promotes monoamine release in vivo (except NE) and in vitro (Yamamoto and Spanos 1988; Johnson et al. 1986; Fitzgerald and Reid 1990; Gough et al. 1991; Gudelsky and Nash 1996; Rothman et al. 2001; Zaczek et al. 1990; O'Shea et al. 2001; Mechan et al. 2002; Nash and Brodkin 1991; Koch and Galloway 1997).
Conceivably, data derived from cell lines expressing the cloned human transporters may not fully reflect transporter pharmacology in human neurons. This is unlikely, as the pharmacological specificities of drugs at biogenic amine transporters expressed in various regions of a macaque monkey's primate brain corresponded closely (r 2=0.93 for NET, 0.98 for DAT, and 0.99 for SERT) to affinities derived from cell lines expressing cloned macaque monkey transporters (Miller et al. 2001).
For the first time, we demonstrate the transport of [3H]MDMA by human monoamine transporters in a stereospecific-, concentration-, time-, and temperature-dependent manner. Contrary to conclusions drawn from rat transporters, MDMA did not display selective effects at the human SERT compared with the DAT or the NET. Indeed, MDMA affinity for the human NET was higher than for DAT or SERT, warranting further investigation of the functional and therapeutic significance of NET–MDMA interactions.
Methods
Stable expression of DAT, NET, and SERT in HEK-293 cells
Human embryo kidney (HEK)-293 cells were stably transfected with the human DAT, NET, or SERT as previously described (Miller et al. 2001; Goulet et al. 2001). Cells were grown in 145-mm untreated tissue culture dishes (Greiner America, Inc., Lake Mary, FL) in Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% fetal bovine serum, 100 U ml−1 penicillin, 100 μg streptomycin, and 0.1 mM nonessential amino acids (all from Life Technologies, Rockville, MD), at 5% CO2 in a 37°C water-jacketed incubator.
Transporter assays: [3H]S(+), [3H]R(−), and [3H]RS(±)MDMA kinetics
For [3H]MDMA experiments, 200 μl of native HEK whole-cell suspensions and whole-cell suspensions of HEK cells stably transfected with DAT, NET, or SERT were preincubated with 200 μl of assay buffer for 10 min on an orbital shaker. Nonspecific transport was determined by preincubating 200 μl of DAT, NET, or SERT whole-cell suspensions with 200 μl of selective uptake inhibitors [10 μM mazindol (DAT assays), 10 μM desipramine (NET assays), and 10 μM fluoxetine (SERT assays)] for 10 min on an orbital shaker. Transport was initiated by the addition of 200 μl of [3H](±)MDMA (final volume 600 μl) at a final concentration of 328 nM per tube and allowed to proceed for various times (0–60 min) at 37 or 0°C (n=2). Following incubation, experiments were terminated by placing the test tubes in ice. The cells were harvested by centrifuging test tubes at 16,600×g for 15 min (∼0°C) and aspirating the supernatant. Cells were lysed with 100 μl sodium dodecyl sulfate (SDS, 0.1% for ∼24 h at room temperature) and counted in 4 ml Readysafe scintillation fluid for 5 min on an LS6000IC Beckman (Fullerton, CA) scintillation spectrophotometer. Nonspecific transport was subtracted from the total disintegrations per minute (dpm) to yield specific accumulation of [3H](±)MDMA.
Affinities of [3H]DA, [3H]NE, [3H]5-HT, and [3H](±)MDMA for DAT, NET, and SERT
The affinities of [3H]DA, [3H]NE, [3H]5-HT, [3H](+), [3H](−), and [3H](±)MDMA for the DAT, NET, and SERT were determined by incubating DAT, NET, and SERT cells with various concentrations of each MDMA enantiomer and their respective endogenous substrate. Whole-cell suspensions were preincubated with 200 μl of assay buffer or 200 μl of their respective transport uptake inhibitors (100 μM) for 15 min. Transport of the monoamines was initiated by adding 200 μl of 10 nM [3H]DA (DAT), [3H]NE (NET), or [3H]5-HT (SERT) with various concentrations of the unlabeled monoamine (66–30,000 nM). Transport of [3H]MDMA was initiated by adding 200 μl of [3H](+), [3H](−), or [3H](±)MDMA at various concentrations (10–9,000 nM). For [3H]MDMA assays, initial experiments were conducted with seven to ten concentrations, using a maximum of 9,000 nM (n≥2). Subsequent studies used ten concentrations with a maximum of 2,000 nM (n≥3). All data points up to 2,000 nM were included for analysis. Following a 10-min incubation for [3H]DA, [3H]NE, and [3H]5-HT, or a 6-min incubation for [3H]MDMA, cells were harvested by the same procedures described above to determine specific dpm. Data were fitted to the Michaelis–Menten equation by nonlinear curve fitting.
Inhibition of [3H]DA, [3H]NE, and [3H]5-HT transport
Test tubes containing 200 μl of the cell suspension and 200 μl of various concentrations of test drugs were preincubated for 15 min at 37°C. Next, 200 μl of [3H]DA, [3H]NE, or [3H]5-HT (10 nM) were added to initiate transport and incubated for another 10 min. Following incubation, cells were harvested by centrifugation at approximately 0°C, and radioactive counts were determined as described above. Nonspecific binding was determined in the presence of 10 μM of transport uptake inhibitors and subtracted from total counts to yield specific accumulation.
MDMA affinity for [3H]citalopram, [3H]nisoxetine, and [3H]CFT binding sites
Whole-cell suspensions (200 μl) were incubated with various drug dilutions (200 μl) and 1 nM of the labeled ligand [200 μl; [3H]citalopram (SERT), [3H]nisoxetine (NET), or [3H]CFT (DAT)] for 2 h on ice as described (Madras et al. 1989b, 1996; Goulet et al. 2001). Experiments were terminated by centrifugation and aspiration of the supernatant as described above. Nonspecific binding, measured with fluoxetine (10 μM, SERT), (−)-cocaine (30 μM, DAT), and desipramine (30 μM, NET) was subtracted from total dpm to calculate specific binding.
MDMA-induced release of [3H]DA, [3H]NE, and [3H]5-HT
Procedures for release assays were adapted (Rothman et al. 2001). Spontaneous release of [3H]DA, [3H]NE, and [3H]5-HT was determined to be less than 10% of the maximal uptake achieved. DAT, NET, or SERT cells (200 μl) were incubated to steady state with 10 nM of the appropriate radioligand (200 μl; 30 min for [3H]5-HT and [3H]NE and 40 min for [3H]DA) in an uptake buffer at 37°C. After steady-state incubation, cells were exposed to various concentrations of test drugs in an uptake buffer (200 μl). After 15 min, the release reaction was terminated by placing the test tubes in ice. Cells were harvested by centrifugation at 0°C followed by rapid aspiration. Nonspecific binding was determined in the presence of 10 μM of transport uptake inhibitors, which was a 15-min pretreatment before incubation with radioligands, and subtracted from total counts to yield specific accumulation.
Data analysis
All points were assayed in triplicate, and each experiment was independently repeated at least three times (except where noted) with different cell preparations. Data analyses were performed as previously described (Miller et al. 2001; Goulet et al. 2001) using GraphPad Prism software (San Diego, CA). In uptake experiments, K i values were calculated according to the formula K i=IC50/(1+L/K m) (Cheng and Prusoff 1973), where L is the concentration of the radioligand ([3H]DA, [3H]NE, [3H]5-HT, or [3H]MDMA).
Materials
(−) and (+)-[6′-3H(n)]-3′,4′-MDMA hydrochloride (specific activity [3H](−)-MDMA 0.22 and 0.44 Ci mmol−1; [3H](+)-MDMA 0.24 and 0.853 Ci mmol−1) was kindly provided by the National Institute on Drug Abuse (NIDA, Bethesda, MD). A racemic mixture of [3H]MDMA was constituted by mixing equal concentrations of [3H](−)-MDMA and [3H](+)-MDMA. MDMA (±), (−), and (+) was also provided by NIDA. [3H]DA, (specific activity 23.5 Ci mmol−1) [3H]NE (specific activity 52 Ci mmol−1), [3H]CFT, or WIN 35,428—2β-carbomethoxy-3β-(4-fluorophenyl)tropane (specific activity 87 Ci mmol−1), [3H]nisoxetine (specific activity 86 Ci mmol−1), and [3H]citalopram (specific activity 72 Ci mmol−1)—were all purchased from PerkinElmer Life Sciences (Boston, MA). [3H]5-HT (specific activity 133 Ci mmol−1) was purchased from Amersham Biosciences (Buckinghamshire, UK). All others drugs were obtained from Sigma (St. Louis, MO). Cell lines were a kind gift from Dr. B. Hoffman.
Results
Affinities of [3H]DA, [3H]NE, and [3H]5-HT for the DAT, NET, and SERT
To compare MDMA effects at monoamine transporters with endogenous neurotransmitters, we conducted assays with [3H]DA, [3H]NE, and [3H]5-HT and the human DAT, NET, and SERT. The time course of transport of 5-HT (Goulet et al. 2001), DA (Yatin et al. 2002), and NE had been previously determined and verified (data not shown). [3H]Monoamine transport assays were conducted for 10 min, and affinities (K m) and velocities (V max) of [3H]DA for the DAT, [3H]NE for the NET, and [3H]5HT for the SERT were measured. For all three transporters, transport was saturable with increasing neurotransmitter concentration (Fig. 1).
Transport velocity of [3H]DA, [3H]NE, and [3H]5-HT as a function of concentration. Each [3H]monoamine (66–30,000 nM) was incubated with HEK-293 cells stably transfected with the human DAT (▪), n=3; NET (▴), n=3; or SERT (•), n=4. The K m and V max values are provided in Table 1
The affinity of [3H]DA for DAT was 932±186 nM (K m), and carrier capacity (V max) was 65.4±12 fmol min−1 106 cells−1. [3H]NE transport affinity for the NET was K m 789±126 nM, although transport capacity was lower (V max 30.3±1.88 fmol min −1 106 cells−1). The affinity of [3H]5-HT for the SERT transporter was higher than for the other transporters (K m 398±64 nM), while transport capacity was similar to the NET (V max 39.4±3.6 fmol min−1 106 cells−1, Table 1).
Kinetics of [3H](±)-MDMA transport
We next conducted a series of experiments with MDMA at the human DAT, NET, and SERT to establish affinities of [3H]MDMA as a substrate for the monoamine transporters and to determine whether these values corresponded to MDMA affinities for blocking monoamine transport, inhibiting radiolabeled transport inhibitor binding, and/or promoting release of monoamines.
The association of [3H](±)-MDMA (328 nM) with the DAT, NET, and SERT was time-, temperature-, and transporter-dependent. Transport of [3H](±)-MDMA by the DAT, NET, and SERT was rapid and achieved steady state within 10 min (Fig. 2a–c). Subsequent [3H](±)-MDMA assays were conducted for a 6-min time period. Incubations conducted at 37°C were sevenfold higher than those at 0°C, supporting the view that [3H](±)-MDMA was actively transported by the DAT, NET, and SERT. [3H](±)-MDMA accumulation by untransfected HEK-293 cells was higher than accumulation at 0°C in cells transfected with monoamine transporters and remained stable throughout the course of the assay. The more than 3:1 ratio of DAT-dependent (DAT-transfected HEK-293 cells) vs DAT-independent (untransfected HEK-293 cells) accumulation of [3H]MDMA accumulation (Fig. 2a) was higher than corresponding values for NET or SERT (Fig. 2b,c). Under the present conditions, approximately 67, 52, and 60% of [3H](±)-MDMA transport were DAT-, NET-, or SERT-mediated, and the remainder of [3H](±)-MDMA cell-associated radioactivity was not carrier-mediated. The accumulation of radioactivity in the absence of a transporter is attributable to the conditions of the centrifugation assay, which does not tolerate extensive washing procedures.
[3H](±)-MDMA (328 nM) transport as a function of time, temperature, and cell line. a [3H](±)-MDMA was incubated with HEK-293 cells transfected with the human DAT for 0–25 min at 0° (▾), at 37° (▴), or in untransfected HEK-293 cells at 37°C (▪). Transport achieved maximum velocity in less than 10 min. At 0°C and 10 min, transport was less than 20% of [3H](±)MDMA transport at 37°C. b [3H](±)-MDMA was incubated with HEK-293 cells transfected with the human NET for 0–25 min at 0° (▾), at 37° (▴), or in untransfected HEK-293 cells at 37°C (▪). Transport achieved maximum velocity in less than 10 min, and at 0°C, was less than 20% of transport at 37°C. c [3H](±)-MDMA was incubated with HEK-293 cells transfected with the human SERT 0–25 min at 0 (▾), at 37 (▴), or in untransfected HEK-293 cells at 37°C (▪). Transport achieved maximum velocity in less than 10 min; at 0°C, transport was lower than 20% of [3H](±)-MDMA transport at 37°C. dpm refers to disintegrations per minute of radioactivity monitored by liquid scintillation spectrometry
MDMA and the DAT
The transport of [3H](±)-MDMA by the DAT was saturable (Fig. 3a, top left), and the affinity K m 1,490±393 nM was similar to that of [3H]DA (Table 1). [3H](+)-MDMA affinity for the DAT was approximately 3 times higher than racemic MDMA and 20 times higher than [3H](−)-MDMA, indicative of stereoselective transport (Table 1 and Fig. 3a, top left). Interestingly, DAT transport capacity for [3H](±)-MDMA (V max 14.0±2.5 fmol min−1 106 cells−1) was 20% of transport capacity for [3H]DA (Table 1). In comparing the velocity of transport for racemic MDMA and its stereoisomers, the highest transport capacity was exhibited by [3H](−)-MDMA. To compare these values with the potency of MDMA to block [3H]DA transport by the human DAT, we coincubated various concentrations of (±)-MDMA, (+)-MDMA, or (−)-MDMA with [3H]DA in HEK-293 cells transfected with the human DAT and compared the effects with unlabeled DA and mazindol (Table 2). (±)-MDMA inhibited [3H]DA transport in a concentration-dependent manner (Fig. 3b, top right), with relatively low affinity (IC50 1,020±291 nM), but comparable to the K m value for [3H](±)-MDMA transport by the DAT (Tables 1 and 2). The affinities for the (+) and (−) enantiomers of MDMA were similar in both assays, as (+)-MDMA inhibited [3H]DA transport with approximately twice the potency of the racemic mixture, whereas (−)-MDMA was 50 times less potent. Overall, DAT affinities for the three radiolabeled forms of MDMA corresponded to their affinities for blocking [3H]DA transport (Fig. 3b and Tables 1 and 2, left column).
MDMA and the human DAT. a (top left) Velocity and transport capacity of the human DAT as a function of (±)-MDMA and (+)MDMA concentrations. Various concentrations of [3H](±)-MDMA (▴) or (+)-MDMA (▪) (10–1,300 nM) were incubated with HEK-293 cells stably transfected with the DAT at 37°C. The data represent the means±SEM of at least six independent experiments. b (top right) Inhibition of [3H]DA transport (10 nM) by various concentrations of (±)-MDMA (▴), DA (•), and mazindol (▪). c (bottom left) Inhibition of [3H]CFT binding (1 nM) to DAT. Various concentrations of (±)-MDMA (▴), DA (•), and mazindol (▪) were incubated with [3H]CFT (1 nM), and the affinities of the drugs measured after equilibrium was achieved. Note the reduced potencies of DA and MDMA compared with potencies displayed in b. d (bottom right) [3H]DA release assays. Various concentrations of (±)-MDMA (▴), DA (•), and mazindol (▪) were incubated with DAT cells after preloading with [3H]DA (10 nM). Affinities of the drugs were measured after equilibrium was achieved (40 min). All values are provided in Tables 2, 3, and 4
To further resolve whether MDMA is a DAT substrate or inhibitor, we postulated that, as with other substrates, MDMA potency at [3H]CFT binding sites on the DAT would be lower than its potency for blocking [3H]DA transport, possibly reflecting different substrate and inhibitor domains on transporters. In contrast, inhibitor potencies for both parameters at the DAT are similar (Madras et al. 1989a; Goulet et al. 2001; Eshleman et al. 1999). (±)-MDMA was tenfold weaker as an inhibitor of [3H]CFT binding than as a substrate for the DAT (Fig. 3c and Table 3, left column). The [3H]MDMA results paralleled those of the substrate dopamine but contrasted with the DAT inhibitor mazindol, which displayed similar affinities for inhibiting [3H]DA transport and for competing with [3H]CFT binding.
Another parameter to help clarify the substrate properties of (±)-MDMA at the DAT is to compare its potency for releasing [3H]DA from human (h)DAT cells with MDMA affinity for transport. Initially, we determined the effect of incubation time on drug-induced [3H]DA release, generated dose–response curves with mazindol, DA, and MDMA, and terminated the incubations after 5, 15, or 30 min. With 30-min incubations, even high concentrations of the uptake inhibitor mazindol released no more than 10% of accumulated radioligands. In contrast, DA- and MDMA-induced release was almost identical at all incubation times. Based on these results, release assays were terminated after 15 min. The uptake inhibitor mazindol was inactive in the release assays. In contrast to mazindol, the substrates DA and MDMA were active in both uptake and release assays. Cells were preloaded with [3H]DA and then incubated with (±)-MDMA or DA. (±)-MDMA released DA from the cells, in a concentration-dependent manner, with an apparent affinity (1,290±198 nM) that corresponded to its affinity as a substrate (Fig. 3d and Tables 1, 2, and 4). Dopamine also promoted [3H]DA release from hDAT cells preloaded with [3H]DA, with both DA and (±)-MDMA releasing approximately 60% of intracellular [3H]DA (Fig. 3d). Taken together, these experiments support the view that MDMA is a DAT substrate.
MDMA and the NET
Under these assay conditions, the affinity of [3H](±)-MDMA (K m 377±235 nM) for the NET was four times higher than its affinity for the DAT and higher than that of [3H]NE for the NET (K m 789±126 nM) (Table 1 and Fig. 4a). Stereoselective transport was again evident, as the affinity of [3H](+)-MDMA for the NET was approximately twice as high as racemic MDMA and 32 times higher than [3H](−)-MDMA (Table 1). Compared with [3H]NE transport capacity, NET transport capacity was approximately 12 times lower for racemic MDMA and 27 times higher for [3H](−)-MDMA (Table 1 and Fig. 4a, top left). The affinity of [3H](±)-MDMA as a NET substrate (K m 377±235 nM) paralleled its potency for blocking [3H]NE transport (IC50 375±60 nM) (Fig. 4a,b, Tables 1 and 2). Based on these data, we concluded that MDMA is a relatively potent substrate for the NET and a competitive inhibitor of [3H]NE transport.
MDMA and the human NET. a (top left) Velocity and transport capacity of the human NET as a function of (±)-MDMA and (+)-MDMA concentrations. Various concentrations of [3H](±)-MDMA (▴) or (+)-MDMA (▪) (10–1,000 nM) were incubated with HEK-293 cells stably transfected with the NET at 37°C. The data represent the means±SEM of three to nine independent experiments. b (top right) Inhibition of [3H]NE transport (10 nM) by various concentrations of (±)-MDMA (▴), NE (•), and desipramine (▪). c (bottom left) Inhibition of [3H]nisoxetine binding (1 nM) to NET. Various concentrations of (±)-MDMA (▴), NE (•), and desipramine (▪) were incubated with [3H]nisoxetine (1 nM), and the affinities of the drugs measured after equilibrium was achieved. Note the reduced potencies of NE and MDMA compared with potencies displayed in b. d (bottom right) [3H]NE release assays. Various concentrations of (±)-MDMA (▴), NE (•), and desipramine (▪) were incubated with NET cells after preloading with [3H]NE (10 nM). Affinities of the drugs were measured after equilibrium was achieved (30 min). All values are provided in Tables 2, 3, and 4
In parallel to results with the DAT, stereoselective inhibition of [3H]NE transport was observed. Overall, the affinities of the racemic and enantiomeric radiolabeled forms of MDMA corresponded closely to their affinities for blocking [3H]NE transport (Fig. 4b and Tables 1 and 2, middle column). The affinity of unlabeled (+)-MDMA for inhibiting [3H]NE transport was approximately 2.5-fold higher than the racemic mixture, whereas (−)-MDMA was considerably less potent.
(±)-MDMA blocked [3H]NE transport 73 times more potently than [3H]nisoxetine binding to the NET, suggesting that the binding domain of (±)-MDMA differs from that of the transport inhibitor (Fig. 4c and Table 3, middle column). Similarly, the substrate NE was 46 times weaker as an inhibitor of [3H]nisoxetine binding on the NET than as a competitive inhibitor of [3H]NE transport by the NET. In contrast, the NET inhibitor desipramine displayed similar affinities (IC50 2.10±0.35 vs 3.4±0.8 nM) for blocking [3H]NE transport and inhibiting [3H]nisoxetine binding.
Incubation time on drug-induced [3H]NE release was also determined in preparation for release assays with the NET. Similar to results obtained from DAT cells, release assays were terminated after 15-min incubations. The uptake inhibitor desipramine was inactive in the release assays. (±)-MDMA released [3H]NE from hNET cells preloaded with [3H]NE in a dose-dependent manner (Fig. 4d and Table 4). The apparent affinity for [3H]NE release, 267±25, corresponded to its affinity as a NET substrate (Fig. 4d and Tables 1, 2, and 4), but again, release was partial (approximately 55% of intracellular [3H]NE, Fig. 4d). NE also promoted [3H]NE release from hNET cells, with release achieving approximately 65% of control values. Taken together, these experiments support the view that MDMA is a NET substrate.
MDMA and the SERT
Saturation isotherms for the SERT revealed high affinity sites for [3H]5-HT (K m 398±64 nM; V max 39.4±3.6 fmol min−1 106 cell−1, Fig. 1). In comparison with [3H]5-HT, [3H](±)MDMA affinity was approximately 50% lower (K m 910±496 nM), with (+)-MDMA and 5-HT having similar affinity and (−)-MDMA being tenfold weaker. In parallel with the other transporters, the capacity of SERT to transport [3H](±)MDMA was tenfold lower (V max 3.87±1.29 fmol min−1 106 cells−1) than [3H]5-HT, whereas [3H](−)MDMA and [3H]5-HT transport capacities were similar (Table 1 and Fig. 5a, top left). Unlabeled (±)-MDMA was a relatively weak inhibitor of [3H]5-HT transport by the human SERT, with potencies falling in the same range as transport affinities (K m 910±496 vs 1,340±280 nM, Tables 1, 2 and Fig. 5b, top right). [3H]5-HT transport was stereoselectively inhibited by (+)-MDMA, which was approximately nine times more potent than (−)MDMA (Table 2, right column). The affinities of racemic [3H]MDMA and its enantiomers for the SERT corresponded closely to the affinities of their unlabeled forms for blocking [3H]5-HT transport (Fig. 5b and Tables 1 and 2, right column).
MDMA and the human SERT. a (top left) Velocity and transport capacity of the human SERT as a function of (±)-MDMA and (+)-MDMA concentrations. Various concentrations of [3H](±)-MDMA (▴) or (+)-MDMA (▪) (10–1,400 nM) were incubated with HEK-293 cells stably transfected with the SERT at 37°C. The data represent the means±SEM of five to seven independent experiments. b (top right) Inhibition of [3H]5-HT transport (10 nM) by various concentrations of (±)-MDMA (▴), 5-HT (•), and fluoxetine (▪). c (bottom left) Inhibition of [3H]citalopram binding (1 nM) to SERT. Various concentrations of (±)-MDMA (▴), 5-HT (•), and fluoxetine (▪) were incubated with [3H]citalopram (1 nM), and the affinities of the drugs measured after equilibrium was achieved. d (bottom right) [3H]5-HT release assays. Various concentrations of (±)-MDMA (▴), 5-HT (•), and fluoxetine (▪) were incubated with SERT cells after preloading with [3H]5-HT (10 nM). Affinities of the drugs were measured after equilibrium was achieved (30 min). All data are provided in Tables 2, 3, and 4
(±)-MDMA inhibition of [3H]5-HT transport was 12 times more potent than its potency for inhibiting [3H]citalopram binding to the SERT (Tables 2 and 3, right column, and Fig. 5c), indicative of a different binding domain for MDMA and 5-HT compared with a SERT transport inhibitor. [3H]5-HT displayed a modest twofold lower affinity for inhibiting [3H]citalopram binding than for competing with itself as a substrate (Fig. 5c and Table 3, right column).
(±)-MDMA effectively released [3H]5-HT from hSERT cells preloaded with [3H]5-HT (Table 4). The apparent affinity for [3H]5-HT release, 874±35, corresponded to its affinity as a SERT substrate (Fig. 5d and Tables 1, 2 and 4). In contrast to (±)-MDMA-stimulated release in hDAT and hNET cells, (±)-MDMA release of [3H]5-HT was approximately 80% of the total and exceeded the release of [3H]5-HT mediated by 5-HT, which achieved maximum effect at 65% (Fig. 5d and Table 4). Fluoxetine did not produce release of [3H]5-HT.
The relative potencies of [3H](±)-MDMA, [3H](+)-MDMA, and [3H](−)-MDMA as substrates for the DAT, NET, and SERT were highly correlated with their potencies for inhibiting the transport of [3H]DA, [3H]NE, or [3H]5-HT (Fig. 6).
Relationship between substrate affinities of various forms of [3H]MDMA for monoamine transporters and affinities of unlabeled MDMA forms for inhibiting monoamine transport. K m values for [3H](±)-MDMA, [3H](+)-MDMA, and [3H](−)-MDMA as a substrate for the DAT, NET, and SERT (x-axis) were compared with IC50 values of (±)-MDMA, (+)-MDMA, and (−)-MDMA for blocking [3H]DA, [3H]NE, and [3H]5-HT transport by the DAT, NET, and SERT, respectively (y-axis; Tables 1 and 2)
Discussion
It is well established that MDMA is selectively neurotoxic to the brain 5-HT neurons in rats, guinea pigs, and primates as a function of dose and dosing regimen. The mechanisms by which MDMA induces neurotoxic effects remain controversial. Carrier-dependent transport of MDMA metabolic toxic products, oxidative stress, hyperthermia, apoptosis, and increased extracellular concentrations of DA and 5-HT are postulated as underlying causes (Simantov and Tauber 1997; Shankaran et al. 1999; Sanchez et al. 2001; Green et al. 2003). The selective neurotoxic effects of MDMA on serotonin neurons are nonetheless frequently attributed to the relatively higher affinity of MDMA for the rodent SERT compared with the DAT (Rudnick and Wall 1992; Johnson et al. 1991; Steele et al. 1987). This premise has been extrapolated to the human brain (Colado et al. 2004) in the absence of supportive evidence with human transporters. The present report reexamines whether the relative affinities of MDMA for human monoamine transporters, a conduit of entry of MDMA into monoaminergic neurons, can account for its selective neurotoxic effects of 5-HT neurons in primates.
Based on three independent measures of relative potencies of MDMA at the human monoamine transporters, we now conclude that the selective toxicity of MDMA on 5-HT neurons in the primate brain cannot be attributed to higher MDMA affinity for the SERT compared with the DAT or NET. The only distinctive property displayed by MDMA, with possible implications for the selective neurotoxic effects of MDMA, was its greater capacity to deplete preloaded intracellular [3H]5-HT via the SERT than [3H]DA or [3H]NE. Collectively, these data suggest that MDMA is sequestered from the extracellular to the intracellular milieu by monoamine transporters, leading to reverse transport of monoamines.
Our strategy was to directly characterize the properties of [3H]MDMA at human DAT, NET, and SERT. Previous studies failed to identify specific binding sites for, or transport of, [3H]MDMA, but the use of membrane preparations and low assay temperatures (0–4°C) predictably precluded detection of active transport of [3H]MDMA by monoamine transporters. A filtration assay that yielded saturable [3H]MDMA binding sites on brain membranes (Gehlert et al. 1985) was subsequently discovered to be an artifact of binding to glass fiber filters (Wang et al. 1987). A centrifugation assay at 4°C detected saturable [3H]MDMA binding to whole brain homogenates (Zaczek et al. 1989), but no further characterization studies were conducted to identify the nature of the binding sites. Nonetheless, membrane preparations would have failed to detect active MDMA transport at 4°C.
We introduce an effective assay for measuring [3H]MDMA transport by using cell lines transfected with human monoamine transporters and a centrifugation assay that prevents dissociation of accumulated [3H]MDMA. Based on the following considerations, we conclude that [3H]MDMA is a substrate for the DAT, NET, and SERT:
-
1.
[3H]MDMA sequestration was temperature-dependent;
-
2.
[3H]MDMA sequestration was dependent on the presence of transfected DAT, NET, and SERT (Untransfected HEK-293 cells yielded results similar to experiments conducted in the presence of transport inhibitors, and carrier-mediated transport exceeded 50% of nonspecific cell-associated radioactivity.);
-
3.
[3H]MDMA sequestration was saturable, indicative of a finite transport capacity;
-
4.
[3H]MDMA sequestration was stereoselective, with the (+) enantiomer more potent than the (−) enantiomer at the three transporters, a finding consistent with the higher potency of the (+) isomer in humans (Anderson et al. 1978; but see Steele et al. (1987), who reported no stereoselectivity at the NET);
-
5.
the affinities of racemic and enantiomeric forms of [3H]MDMA as a substrate for transport corresponded closely to the affinities of their unlabeled counterparts for blocking the transport of [3H]DA, [3H]NE, and [3H]5-HT, again suggestive of MDMA as a substrate and competitor of monoamine substrates for transport;
-
6.
[3H]MDMA accumulation by DAT, NET, and SERT was blocked by the potent uptake inhibitors mazindol, desipramine, and fluoxetine (respectively), again reflecting carrier-mediated transport;
-
7.
MDMA affinities at DAT, NET, and SERT radioligand binding sites were lower than their corresponding affinities in transport assays or their affinities to block monoamine transport, findings paralleling those for DA, NE, and 5-HT.
These data imply that the binding domain of MDMA and endogenous monoamine substrates are different from that of inhibitors, a finding highlighted by others (Madras et al. 1989a; Eshleman et al. 1999).
Contrary to data derived from rat transporters, MDMA displayed higher affinity for the human NET and lower affinities for the SERT and DAT, which were similar. However, the apparently low affinity of [3H]MDMA for the human SERT (K m 910 nM) and for inhibiting [3H]5-HT transport (IC50 1,340 nM) was anticipated, as Mortensen et al. (1999), in a side-by-side comparison, reported that MDMA potency for blocking the human SERT (IC50 819 nM) was fourfold lower than corresponding values for the rat SERT (IC50 196 nM). An overall comparison with rat transporters is instructive, as the affinity of MDMA for inhibiting 5-HT transport into rat synaptosomes was tenfold higher than for rat DAT or NET (Battaglia et al. 1988). In a reexamination of these values, MDMA affinities for rat transporters confirmed this rank order of potencies (SERT>NET≫DAT), although the differences between SERT and NET were less robust than in later reports (Rothman and Baumann 2003). The apparent species difference may be attributable to differences in assays conducted with cloned transporters (present study) compared with rat brain synaptosomes, but several reports contradict this postulate (Eshleman et al. 1999). In HeLa cells transiently expressing the SERT, the potency of MDMA to inhibit [3H]5-HT uptake was similar to reports derived from brain tissue (Mortensen et al. 1999), and the pharmacological specificities of drugs at biogenic amine transporters expressed in various regions of the macaque monkey primate brain corresponded closely (0.93 NET, 0.98 DAT, and 0.99 SERT) to their affinities derived from cell lines expressing cloned macaque monkey transporters (Miller et al. 2001).
The selective effects of MDMA on 5-HT neurons may be attributable to the greater effectiveness of MDMA in releasing a higher proportion of intracellular 5-HT from preloaded SERT-expressing cells compared with DA or NE release from DAT- and NET-expressing cells, respectively. Furthermore, MDMA-induced 5-HT release was more extensive than 5-HT-mediated release, while DA and NE were marginally more effective than MDMA in promoting autorelease. Accordingly, MDMA may trigger distinct biochemical sequelae in neurons expressing the SERT compared with DAT or NET. There are several consequences of enhanced 5-HT release that can potentially underlie the selective neurotoxic effects of MDMA. For example, N-terminal phosphorylation of the DAT is required for release of amphetamine but not for amphetamine transport (Khoshbouei et al. 2004). If this process generalizes across all three transporters, the robust 5-HT releasing capacity of MDMA at the SERT may reflect a unique capacity of MDMA to promote phosphorylation at the SERT compared with the DAT or NET, enhancing carrier-mediated release. Conceivably, if transport, release, and transporter trafficking induced by MDMA are linked, then MDMA may regulate SERT differently than DAT or NET. The SERT can be internalized (Ramamoorthy et al. 1998), but 5-HT inhibits this process and maintains cell-surface expression to permit further accumulation of exogenous (e.g., MDMA) and endogenous substrates (Ramamoorthy and Blakely 1999). Thus, the magnified MDMA-induced release of 5-HT can lock SERT on the surface, prevent SERT internalization, and enhance intracellular accumulation of MDMA, neurotransmitters, and toxic metabolites, leading to neuron terminal adaptation or toxicity. In contrast to the SERT, DAT internalization is promoted by amphetamine and DA, thereby reducing transport capacity and diminishing DAT cell-surface availability (Saunders et al. 2000; Sandoval et al. 2001; Hansen et al. 2002). NET is also susceptible to internalization and downregulation, but the effects of NE or MDMA on NET trafficking are not known (Jayanthi et al. 2004). Conceivably, MDMA prevents SERT internalization but promotes DAT and NET internalization, either directly or consequent to MDMA-induced 5-HT, DA, and NE release, thereby potentiating further sequestration of MDMA or putative toxic metabolites to enter 5-HT neurons. Our approach provides a simple model system to investigate whether the transport and release of MDMA differs from that of endogenous substrates and whether it triggers regulatory processes unique to each monoamine transporter.
The capacity of MDMA to promote 5-HT, NE, and DA release from slices, synaptosomes, or in vivo is amply documented (Nichols et al. 1982; Johnson et al. 1986; Fitzgerald and Reid 1990; Berger et al. 1992; Rothman et al. 2001; see White et al. 1996; Green et al. 2003 for a review). However, it should be noted that MDMA interactions in vitro will not necessarily be conserved in vivo (Rothman and Baumann 2003), as other neuronal factors may influence MDMA effects on transporter function. In fact, MDMA-induced monoamine release in vivo can occur through transporter-mediated release, which is presumably the mechanism observed in the present studies, or via exocytotic release (i.e., impulse-dependent). This may be particularly relevant to MDMA-induced DA release, as both impulse- and transporter-mediated release has been reported (Yamamoto et al. 1995). A carrier-mediated mechanism of MDMA-induced 5-HT release has been amply documented (Gudelsky and Nash 1996; Mechan et al. 2002), while the contribution of impulse-dependent mechanisms has not been explored.
Interactions of MDMA with multiple transporters, autoreceptors, and/or postsynaptic receptors may also affect in vivo physiology. MDMA-induced release of DA, but not 5-HT, is inhibited by pretreatment with the NET inhibitor, desipramine, or by depleting brain NE (Shankaran and Gudelsky 1998), which suggests that the MDMA-induced DA increase in vivo may also result from NET transport of MDMA (Shankaran and Gudelsky 1998). Receptors may also contribute to MDMA effects, as MDMA-induced DA release is markedly attenuated by 5-HT2A receptor blockade (Yamamoto et al. 1995; Gudelsky and Nash 1996). α2-Adrenergic receptors are also implicated in MDMA-induced 5-HT release (Battaglia et al. 1988), as MDMA has a relatively high affinity for these receptors, and they are present on 5-HT terminals (Green et al. 2003). Finally, a novel candidate receptor, the trace amine receptor1 (TA1), may also mediate some of the pharmacological effects of MDMA (Bunzow et al. 2001) by four or more mechanisms. First, MDMA and amphetamine activate TA1 (Borowsky et al. 2001; Miller et al. 2005). Second, MDMA potentiates TA1 activity if cotransfected with the DAT (Miller et al. 2005) and, therefore, may influence TA1 activity by modulating DAT, NET, or SERT. Third, the trace amine phenylethylamine (PEA) is an effective substrate for DAT and NET (Madras et al. 2004) and a potent agonist at TA1. Conceivably, MDMA blocks PEA transport and promotes PEA release to modulate TA1 activity. Finally, it has been postulated that the trace amines function as endogenous neuromodulators of classical monoamine neurotransmitters, and MDMA-induced modulation of trace amines may affect monoamines (Berry 2004; Sotnikova et al. 2004). Our findings clearly demonstrate the capacity of MDMA to release NE via the human NET. MDMA reportedly stimulates NE release in rodent brain preparations, a process blocked by the NET-selective inhibitor desipramine (Steele et al. 1989; Lavelle et al. 1999; Rothman et al. 2001; Fitzgerald and Reid 1993), but not confirmed by microdialysis in vivo. MDMA reportedly also promotes tachycardia in rats and humans (Gordon et al. 1991; Hayner and McKinney 1986), desipramine-sensitive vasoconstriction in vitro (Fitzgerald and Reid 1994), and cardiovascular mortality in humans (Dowling et al. 1987). Additionally, MDMA has been linked to intracerebral hemorrhage (Harries and De Silva 1992), with cerebral hyperperfusion demonstrated in rat (Kelly et al. 1994). All of these effects may be related to the high affinity of MDMA for the NET, capacity of MDMA to release NE, and agonist effects at α2-adrenoceptor receptors (Lavelle et al. 1999). Notably, high doses of MDMA can deplete DA and NE in rat and guinea pig brains (Commins et al. 1987; Mayerhofer et al. 2001). Thus, the high affinity of MDMA as a substrate for the human NET warrants further consideration, particularly in devising medications to treat the consequences of acute or repeated exposure to MDMA.
At a practical level, our findings highlight the need to systematically investigate the therapeutic potential of DAT, NET, and SERT inhibitors to alleviate the acute and long-term pharmacological consequences of MDMA. In rodents, a serotonin-selective drug inhibits MDMA-induced effects on the immune system and partly attenuates anxiety and depressive-like behaviors (Pacifici et al. 2004; Thompson et al. 2004). In human users, the serotonin-selective transport inhibitor citalopram reportedly attenuates the acute psychological (heightened mood, increased self-confidence, and enhanced sensory perception) effects of MDMA (Liechti et al. 2000). Whether a SERT inhibitor will also curtail MDMA-induced transformation of serotonin neurons in the human brain after repeated use is unknown. Equally intriguing is whether high-affinity NET-selective inhibitors or nonselective monoamine transport inhibitors will be as, or more, effective than SERT inhibitors in diminishing the acute and long-term consequences of MDMA.
References
Anderson GM III, Braun G, Braun U, Nichols DE, Shulgin AT (1978) Absolute configuration and psychotomimetic activity. NIDA Res Monogr (22):8–15
Battaglia G, Brooks BP, Kulsakdinun C, De Souza EB (1988) Pharmacologic profile of MDMA (3,4-methylenedioxymethamphetamine) at various brain recognition sites. Eur J Pharmacol 149:159–163
Berger UV, Gu XF, Azmitia EC (1992) The substituted amphetamines 3,4-methylenedioxymethamphetamine, methamphetamine, p-chloroamphetamine and fenfluramine induce 5-hydroxytryptamine release via a common mechanism blocked by fluoxetine and cocaine. Eur J Pharmacol 215:153–160
Berry MD (2004) Mammalian central nervous system trace amines. Pharmacologic amphetamines, physiologic neuromodulators. J Neurochem 90(2):257–271
Borowsky B, Adham N, Jones KA, Raddatz R, Artymyshyn R, Ogozalek KL, Durkin MM, Lakhlani PP, Bonini JA, Pathirana S, Boyle N, Pu X, Kouranova E, Lichtblau H, Ochoa FY, Branchek TA, Gerald C (2001) Trace amines: identification of a family of mammalian G protein-coupled receptors. Proc Natl Acad Sci U S A 98:8966–8971
Bowyer JF, Young JF, Slikker W, Itzak Y, Mayorga AJ, Newport GD, Ali SF, Frederick DL, Paule MG (2003) Plasma levels of parent compound and metabolites after doses of either d-fenfluramine or d-3,4-methylenedioxymethamphetamine (MDMA) that produce long-term serotonergic alterations. Neurotoxicology 24:379–390
Buchert R, Thomasius R, Wilke F, Petersen K, Nebeling B, Obrocki J, Schulze O, Schmidt U, Clausen M (2004) A voxel-based PET investigation of the long-term effects of “Ecstasy” consumption on brain serotonin transporters. Am J Psychiatry 161:1181–1189
Bunzow JR, Sonders MS, Arttamangkul S, Harrison LM, Zhang G, Quigley DI, Darland T, Suchland KL, Pasumamula S, Kennedy JL, Olson SB, Magenis RE, Amara SG, Grandy DK (2001) Amphetamine, 3,4-methylenedioxymethamphetamine, lysergic acid diethylamide, and metabolites of the catecholamine neurotransmitters are agonists of a rat trace amine receptor. Mol Pharmacol 60:1181–1188
Check E (2004) Psychedelic drugs: the ups and downs of ecstasy. Nature 429:126–128
Cheng Y, Prusoff WH (1973) Relationship between the inhibition constant (K1) and the concentration of inhibitor which causes 50 per cent inhibition (I50) of an enzymatic reaction. Biochem Pharmacol 22:3099–3108
Colado MI, O'Shea E, Green AR (2004) Acute and long-term effects of MDMA on cerebral dopamine biochemistry and function. Psychopharmacology (Berl) 173:249–263
Commins DL, Vosmer G, Virus RM, Woolverton WL, Schuster CR, Seiden LS (1987) Biochemical and histological evidence that methylenedioxymethylamphetamine (MDMA) is toxic to neurons in the rat brain. J Pharmacol Exp Ther 241:338–345
Dowling GP, McDonough ET III, Bost RO (1987) ‘Eve’ and ‘Ecstasy’. A report of five deaths associated with the use of MDEA and MDMA. JAMA 257:1615–1617
Eshleman AJ, Neve RL, Janowsky A, Neve KA (1995) Characterization of a recombinant human dopamine transporter in multiple cell lines. J Pharmacol Exp Ther 274:276–283
Eshleman AJ, Carmolli M, Cumbay M, Martens CR, Neve KA, Janowsky A (1999) Characteristics of drug interactions with recombinant biogenic amine transporters expressed in the same cell type. J Pharmacol Exp Ther 289:877–885
Fitzgerald JL, Reid JJ (1990) Effects of methylenedioxymethamphetamine on the release of monoamines from rat brain slices. Eur J Pharmacol 191:217–220
Fitzgerald JL, Reid JJ (1993) Interactions of methylenedioxymethamphetamine with monoamine transmitter release mechanisms in rat brain slices. Naunyn Schmiedebergs Arch Pharmacol 347:313–323
Fitzgerald JL, Reid JJ (1994) Sympathomimetic actions of methylenedioxymethamphetamine in rat and rabbit isolated cardiovascular tissues. J Pharm Pharmacol 46:826–832
Gehlert DR, Schmidt CJ, Wu L, Lovenberg W (1985) Evidence for specific methylenedioxymethamphetamine (Ecstasy) binding sites in the rat brain. Eur J Pharmacol 119:135–136
Gordon CJ, Watkinson WP, O'Callaghan JP, Miller DB (1991) Effects of 3,4-methylenedioxymethamphetamine on autonomic thermoregulatory responses of the rat. Pharmacol Biochem Behav 38:339–344
Gough B, Ali SF, Slikker W Jr, Holson RR (1991) Acute effects of 3,4-methylenedioxymethamphetamine (MDMA) on monoamines in rat caudate. Pharmacol Biochem Behav 39:619–623
Goulet M, Miller GM, Bendor J, Liu S, Meltzer PC, Madras BK (2001) Non-amines, drugs without an amine nitrogen, potently block serotonin transport: novel antidepressant candidates? Synapse 42:129–140
Green AR, Mechan AO, Elliott JM, O'Shea E, Colado MI (2003) The pharmacology and clinical pharmacology of 3,4-methylenedioxymethamphetamine (MDMA, “Ecstasy”). Pharmacol Rev 55:463–508
Gudelsky GA, Nash JF (1996) Carrier-mediated release of serotonin by 3,4-methylenedioxymethamphetamine: implications for serotonin–dopamine interactions. J Neurochem 66:243–249
Hansen JP, Riddle EL, Sandoval V, Brown JM, Gibb JW, Hanson GR, Fleckenstein AE (2002) Methylenedioxymethamphetamine decreases plasmalemmal and vesicular dopamine transport: mechanisms and implications for neurotoxicity. J Pharmacol Exp Ther 300:1093–1100
Harries DP, De Silva R (1992) ‘Ecstasy’ and intracerebral haemorrhage. Scott Med J 37:150–152
Hatzidimitriou G, McCann UD, Ricaurte GA (1999) Altered serotonin innervation patterns in the forebrain of monkeys treated with (±)3,4-methylenedioxymethamphetamine seven years previously: factors influencing abnormal recovery. J Neurosci 19:5096–5107
Hayner GN, McKinney H (1986) MDMA. The dark side of ecstasy. J Psychoactive Drugs 18:341–347
Jayanthi LD, Samuvel DJ, Ramamoorthy S (2004) Regulated internalization and phosphorylation of the native norepinephrine transporter in response to phorbol esters. Evidence for localization in lipid rafts and lipid raft-mediated internalization. J Biol Chem 279:19315–19326
Johnson MP, Hoffman AJ, Nichols DE (1986) Effects of the enantiomers of MDA, MDMA and related analogues on [3H]serotonin and [3H]dopamine release from superfused rat brain slices. Eur J Pharmacol 132:269–276
Johnson MP, Conarty PF, Nichols DE (1991) [3H]Monoamine releasing and uptake inhibition properties of 3,4-methylenedioxymethamphetamine and p-chloroamphetamine analogues. Eur J Pharmacol 200:9–16
Kelly PA, Ritchie IM, Sangra M, Cursham MJ, Dickson EM, Kelly B, Neilson FP, Reidy MJ, Stevens MC (1994) Hyperaemia in rat neocortex produced by acute exposure to methylenedioxymethamphetamine. Brain Res 665:315–318
Khoshbouei H, Sen N, Guptaroy B, Johnson L, Lund D, Gnegy ME, Galli A, Javitch JA (2004) N-terminal phosphorylation of the dopamine transporter is required for amphetamine-induced efflux. PLoS Biol 2:E78
Kish SJ (2002) How strong is the evidence that brain serotonin neurons are damaged in human users of ecstasy? Pharmacol Biochem Behav 71:845–855
Koch S, Galloway MP (1997) MDMA induced dopamine release in vivo: role of endogenous serotonin. J Neural Transm 104:135–46
Lavelle A, Honner V, Docherty JR (1999) Investigation of the prejunctional alpha2-adrenoceptor mediated actions of MDMA in rat atrium and vas deferens. Br J Pharmacol 128:975–980
Liechti ME, Baumann C, Gamma A, Vollenweider FX (2000) Acute psychological effects of 3,4-methylenedioxymethamphetamine (MDMA, “Ecstasy”) are attenuated by the serotonin uptake inhibitor citalopram. Neuropsychopharmacology 22:513–521
Logan BJ, Laverty R, Sanderson WD, Yee YB (1988) Differences between rats and mice in MDMA (methylenedioxymethylamphetamine) neurotoxicity. Eur J Pharmacol 152:227–234
Madras BK, Fahey MA, Bergman J, Canfield DR, Spealman RD (1989a) Effects of cocaine and related drugs in nonhuman primates. I. [3H]Cocaine binding sites in caudate–putamen. J Pharmacol Exp Ther 251:131–141
Madras BK, Spealman RD, Fahey MA, Neumeyer JL, Saha JK, Milius RA (1989b) Cocaine receptors labeled by [3H]2β-cabomethoxy-3β-(4-fluorophenyl)tropane. Mol Pharmacol 36:518–524
Madras BK, Jones AG, Mahmod A, Zimmerman RE, Garada B, Holman LB, Davison A, Blundell P, Meltzer PC (1996) Technepine: a high affinity 99mtechnetium probe to label the dopamine transporter in brain by SPECT imaging. Synapse 22:239–246
Madras BK, Verrico C, Jassen A, Miller GM (2004) Attention Deficit Hyperactivity Disorder (ADHD): new roles for old trace amines and monoamine transporters. Neuropsychopharmacology 29(Suppl. 1):S 137
Mayerhofer A, Kovar KA, Schmidt WJ (2001) Changes in serotonin, dopamine and noradrenaline levels in striatum and nucleus accumbens after repeated administration of the abused drug MDMA in rats. Neurosci Lett 308:99–102
McCann UD, Ricaurte GA (2004) Amphetamine neurotoxicity: accomplishments and remaining challenges. Neurosci Biobehav Rev 27:821–826
McCann UD, Szabo Z, Seckin E, Rosenblatt P, Mathews WB, Ravert HT, Dannals RF, Ricaurte GA (2005) Quantitative PET Studies of the Serotonin Transporter in MDMA Users and Controls Using [(11)C]McN5652 and [(11)C]DASB. Neuropsychopharmacology 30(9):1741–1750. DOI 10.1038/sj.npp.1300736
Mechan AO, Esteban B, O'Shea E, Elliott JM, Colado MI, Green AR (2002) The pharmacology of the acute hyperthermic response that follows administration of 3,4-methylenedioxymethamphetamine (MDMA, ‘ecstasy’) to rats. Br J Pharmacol 135:170–180
Miller GM, Yatin SM, De La Garza R II, Goulet M, Madras BK (2001) Cloning of dopamine, norepinephrine and serotonin transporters from monkey brain: relevance to cocaine sensitivity. Brain Res Mol Brain Res 87:124–143
Miller GM, Verrico CD, Jassen AK, Konar M, Yang H, Panas HN, Bahn M, Johnson RS, Madras BK (2005) Primate trace amine receptor 1 modulation by the dopamine transporter. J Pharmacol Exp Ther 313(3):983–994. DOI 10.1124/jpet.105.084459
Mortensen OV, Kristensen AS, Rudnick G, Wiborg O (1999) Molecular cloning, expression and characterization of a bovine serotonin transporter. Brain Res Mol Brain Res 71:120–126
Nash JF, Brodkin J (1991) Microdialysis studies on 3,4-methylenedioxymethamphetamine-induced dopamine release: effect of dopamine uptake inhibitors. J Pharmacol Exp Ther 259:820–825
Nash JF, Yamamoto BK (1992) Methamphetamine neurotoxicity and striatal glutamate release: comparison to 3,4-methylenedioxymethamphetamine. Brain Res 581:237–243
Nichols DE, Lloyd DH, Hoffman AJ, Nichols MB, Yim GK (1982) Effects of certain hallucinogenic amphetamine analogues on the release of [3H]serotonin from rat brain synaptosomes. J Med Chem 25:530–535
O'Callaghan JP, Miller DB (1994) Neurotoxicity profiles of substituted amphetamines in the C57BL/6J mouse. J Pharmacol Exp Ther 270:741–751
O'Shea E, Esteban B, Camarero J, Green AR, Colado MI (2001) Effect of GBR 12909 and fluoxetine on the acute and long term changes induced by MDMA (‘ecstasy’) on the 5-HT and dopamine concentrations in mouse brain. Neuropharmacology 40:65–74
Pacifici R, Pichini S, Zuccaro P, Farre M, Segura M, Ortuno J, Di Carlo S, Bacosi A, Roset PN, Segura J, de la Torre R (2004) Paroxetine inhibits acute effects of 3,4-methylenedioxymethamphetamine on the immune system in humans. J Pharmacol Exp Ther 309:285–292
Parrott AC (2001) Human psychopharmacology of Ecstasy (MDMA): a review of 15 years of empirical research. Hum Psychopharmacol 16:557–577
Ramamoorthy S, Blakely RD (1999) Phosphorylation and sequestration of serotonin transporters differentially modulated by psychostimulants. Science 285:763–766
Ramamoorthy S, Giovanetti E, Qian Y, Blakely RD (1998) Phosphorylation and regulation of antidepressant-sensitive serotonin transporters. J Biol Chem 273:2458–2466
Reneman L, Booij J, Habraken JB, De Bruin K, Hatzidimitriou G, Den Heeten GJ, Ricaurte GA (2002) Validity of [123I]beta-CIT SPECT in detecting MDMA-induced serotonergic neurotoxicity. Synapse 46:199–205
Ricaurte GA, McCann UD (1992) Neurotoxic amphetamine analogues: effects in monkeys and implications for humans. Ann N Y Acad Sci 648:371–382
Ricaurte GA, DeLanney LE, Irwin I, Langston JW (1988a) Toxic effects of MDMA on central serotonergic neurons in the primate: importance of route and frequency of drug administration. Brain Res 446:165–168
Ricaurte GA, Forno LS, Wilson MA, DeLanney LE, Irwin I, Molliver ME, Langston JW (1988b) (±)3,4-Methylenedioxymethamphetamine selectively damages central serotonergic neurons in nonhuman primates. JAMA 260:51–55
Ricaurte GA, Martello AL, Katz JL, Martello MB (1992) Lasting effects of (±)-3,4-methylenedioxymethamphetamine (MDMA) on central serotonergic neurons in nonhuman primates: neurochemical observations. J Pharmacol Exp Ther 261:616–622
Rothman RB, Baumann MH (2003) Monoamine transporters and psychostimulant drugs. Eur J Pharmacol 479:23–40
Rothman RB, Baumann MH, Dersch CM, Romero DV, Rice KC, Carroll FI, Partilla JS (2001) Amphetamine-type central nervous system stimulants release norepinephrine more potently than they release dopamine and serotonin. Synapse 39:32–41
Rudnick G, Wall SC (1992) The molecular mechanism of ‘ecstasy’ [3,4-methylenedioxymethamphetamine (MDMA)]: serotonin transporters are targets for MDMA-induced serotonin release. Proc Natl Acad Sci U S A 89:1817–1821
Sanchez V, Camarero J, Esteban B, Peter MJ, Green AR, Colado MI (2001) The mechanisms involved in the long-lasting neuroprotective effect of fluoxetine against MDMA (‘ecstasy’)-induced degeneration of 5-HT nerve endings in rat brain. Br J Pharmacol 134:46–57
Sandoval V, Riddle EL, Ugarte YV, Hanson GR, Fleckenstein AE (2001) Methamphetamine-induced rapid and reversible changes in dopamine transporter function: an in vitro model. J Neurosci 21:1413–1419
Saunders C, Ferrer JV, Shi L, Chen J, Merrill G, Lamb ME, Leeb-Lundberg LM, Carvelli L, Javitch JA, Galli A (2000) Amphetamine-induced loss of human dopamine transporter activity: an internalization-dependent and cocaine-sensitive mechanism. Proc Natl Acad Sci U S A 97:6850–6855
Scheffel U, Szabo Z, Mathews WB, Finley PA, Dannals RF, Ravert HT, Szabo K, Yuan J, Ricaurte GA (1998) In vivo detection of short- and long-term MDMA neurotoxicity—a positron emission tomography study in the living baboon brain. Synapse 29:183–192
Shankaran M, Gudelsky GA (1998) Effect of 3,4-methylenedioxymethamphetamine (MDMA) on hippocampal dopamine and serotonin. Pharmacol Biochem Behav 61:361–366
Shankaran M, Yamamoto BK, Gudelsky GA (1999) Involvement of the serotonin transporter in the formation of hydroxyl radicals induced by 3,4-methylenedioxymethamphetamine. Eur J Pharmacol 385:103–110
Simantov R, Tauber M (1997) The abused drug MDMA (Ecstasy) induces programmed death of human serotonergic cells. FASEB J 11:141–146
Slikker W Jr, Ali SF, Scallet AC, Frith CH, Newport GD, Bailey JR (1988) Neurochemical and neurohistological alterations in the rat and monkey produced by orally administered methylenedioxymethamphetamine (MDMA). Toxicol Appl Pharmacol 94:448–457
Slikker W Jr, Holson RR, Ali SF, Kolta MG, Paule MG, Scallet AC, McMillan DE, Bailey JR, Hong JS, Scalzo FM (1989) Behavioral and neurochemical effects of orally administered MDMA in the rodent and nonhuman primate. Neurotoxicology 10:529–542
Sonders MS, Zhu SJ, Zahniser NR, Kavanaugh MP, Amara SG (1997) Multiple ionic conductances of the human dopamine transporter: the actions of dopamine and psychostimulants. J Neurosci 17:960–974
Sotnikova TD, Budygin EA, Jones SR, Dykstra LA, Caron MG, Gainetdinov RR (2004) Dopamine transporter-dependent and -independent actions of trace amine beta-phenylethylamine. J Neurochem 91(2):362–373
Steele TD, Nichols DE, Yim GK (1987) Stereochemical effects of 3,4-methylenedioxymethamphetamine (MDMA) and related amphetamine derivatives on inhibition of uptake of [3H]monoamines into synaptosomes from different regions of rat brain. Biochem Pharmacol 36:2297–2303
Steele TD, Nichols DE, Yim GK (1989) MDMA transiently alters biogenic amines and metabolites in mouse brain and heart. Pharmacol Biochem Behav 34:223–227
Steele TD, McCann UD, Ricaurte GA (1994) 3,4-Methylenedioxymethamphetamine (MDMA, “Ecstasy”): pharmacology and toxicology in animals and humans. Addiction 89:539–551
Taffe MA, Davis SA, Yuan J, Schroeder R, Hatzidimitriou G, Parsons LH, Ricaurte GA, Gold LH (2002) Cognitive performance of MDMA-treated rhesus monkeys: sensitivity to serotonergic challenge. Neuropsychopharmacology 27:993–1005
Taffe MA, Huitron-Resendiz S, Schroeder R, Parsons LH, Henriksen SJ, Gold LH (2003) MDMA exposure alters cognitive and electrophysiological sensitivity to rapid tryptophan depletion in rhesus monkeys. Pharmacol Biochem Behav 76:141–152
Thompson MR, Li KM, Clemens KJ, Gurtman CG, Hunt GE, Cornish JL, McGregor IS (2004) Chronic fluoxetine treatment partly attenuates the long-term anxiety and depressive symptoms induced by MDMA (‘Ecstasy’) in rats. Neuropsychopharmacology 29:694–704
Turner JJ, Parrott AC (2000) ‘Is MDMA a human neurotoxin?’: diverse views from the discussants. Neuropsychobiology 42:42–48
Wang SS, Ricaurte GA, Peroutka SJ (1987) [3H]3,4-Methylenedioxymethamphetamine (MDMA) interactions with brain membranes and glass fiber filter paper. Eur J Pharmacol 138:439–443
White SR, Obradovic T, Imel KM, Wheaton MJ (1996) The effects of methylenedioxymethamphetamine (MDMA, “Ecstasy”) on monoaminergic neurotransmission in the central nervous system. Prog Neurobiol 49:455–479
Xie T, Tong L, McCann UD, Yuan J, Becker KG, Mechan AO, Cheadle C, Donovan DM, Ricaurte GA (2004) Identification and characterization of metallothionein-1 and -2 gene expression in the context of (±)3,4-methylenedioxymethamphetamine-induced toxicity to brain dopaminergic neurons. J Neurosci 24:7043–7050
Yamamoto BK, Spanos LJ (1988) The acute effects of methylenedioxymethamphetamine on dopamine release in the awake-behaving rat. Eur J Pharmacol 148:195–203
Yamamoto BK, Nash JF, Gudelsky GA (1995) Modulation of methylenedioxymethamphetamine-induced striatal dopamine release by the interaction between serotonin and gamma-aminobutyric acid in the substantia nigra. J Pharmacol Exp Ther 273:1063–1070
Yatin SM, Miller GM, Norton C, Madras BK (2002) Dopamine transporter-dependent induction of C-Fos in HEK cells. Synapse 45:52–65
Zaczek R, Hurt S, Culp S, De Souza EB (1989) Characterization of brain interactions with methylenedioxyamphetamine and methylenedioxymethamphetamine. NIDA Res Monogr 94:223–239
Zaczek R, Culp S, De Souza EB (1990) Intrasynaptosomal sequestration of [3H]amphetamine and [3H]methylenedioxyamphetamine: characterization suggests the presence of a factor responsible for maintaining sequestration. J Neurochem 54:195–204
Acknowledgements
Supported by NIDA grants DA11558, DA06303, DA15305, and by NCRR 00168 to B.K.M. We thank Helen Panas, Dina Yang, and Sophia Schippers for excellent technical assistance and Jennifer Carter for manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Klaus A. Miczek as Principal Editor—the special issue “A Contemporary View of MDMA.”
Rights and permissions
About this article
Cite this article
Verrico, C.D., Miller, G.M. & Madras, B.K. MDMA (Ecstasy) and human dopamine, norepinephrine, and serotonin transporters: implications for MDMA-induced neurotoxicity and treatment. Psychopharmacology 189, 489–503 (2007). https://doi.org/10.1007/s00213-005-0174-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-005-0174-5