Abstract
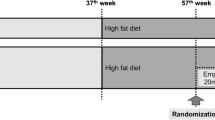
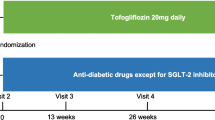
The study aimed to investigate the effects of the sodium-glucose co-transporter 2 (SGLT2) inhibitor empagliflozin on chronic heart failure (HF) in normoglycemic rats. The effects of empagliflozin were compared with the standard medications for HF, e.g., angiotensin-converting enzyme (ACE) inhibitor fosinopril, beta-blocker bisoprolol, and aldosterone antagonist spironolactone. Myocardial infarction (MI) was induced in male Wistar rats via permanent ligation of the left descending coronary artery. One-month post MI, 50 animals were randomized into 5 groups (n = 10): vehicle-treated, empagliflozin (1.0 mg/kg), fosinopril (10 mg/kg), bisoprolol (10 mg/kg), and spironolactone (20 mg/kg). All medications except empagliflozin were titrated within a month and administered per os daily for 3 months. Echocardiography, 24-hour urine volume test, and treadmill exercise tests were performed at the beginning and at the end of the study. Treatment with empagliflozin slowed the progression of left ventricular dysfunction: LV sizes and ejection fraction were not changed and the minute volume was significantly increased (from 52.0 ± 15.5 to 61.2 ± 21.2 ml/min) as compared with baseline. No deaths occurred in empagliflozin group. The 24-hour urine volume tends to be higher in empagliflozin and spironolactone groups than in vehicle and fosinopril group. Moreover, empagliflozin exhibited maximal physical exercise tolerance in comparison with all investigated groups (289 ± 27 s versus 183 ± 61 s in fosinopril group, 197 ± 95 s in bisoprolol group, and 47 ± 46 s in spironolactone group, p = 0.0035 for multiple comparisons). Sodium-glucose co-transporter 2 inhibitor empagliflozin reduced progression of left ventricular dysfunction and improved tolerance of physical exercise in normoglycemic rats with HF. Empagliflozin treatment was superior with respect to physical tolerance compared with fosinopril, bisoprolol, and spironolactone.






Similar content being viewed by others
Abbreviations
- ACE:
-
Angiotensin-converting enzyme
- CV:
-
Cardiovascular
- EF:
-
Ejection fraction
- FS:
-
Left ventricular fraction shortening
- HF:
-
Heart failure
- HR:
-
Heart rate
- IVST:
-
Interventricular septum thickness
- LA_ap:
-
Left atrial antero-posterior dimension
- LA_l:
-
Left atrial long axis dimension
- LA_s:
-
Left atrial short axis dimension
- LV:
-
Left ventricular
- LV EDV:
-
Left ventricular end-diastolic
- LV EDD:
-
Left ventricle end-diastolic diameter
- LV ESD:
-
Left ventricle end-systolic diameters
- LV ESV:
-
Left ventricular end-systolic volumes
- LVM:
-
Left ventricular myocardium mass
- MAPSE:
-
Mitral annular plane systolic excursion
- MI:
-
Myocardial infarction
- MV:
-
Left ventricular minute volume
- PWT:
-
Left ventricular posterior wall thickness in diastole
- RA_l:
-
Long axis dimensions
- RA_s:
-
Right atrium short axis
- RAAS:
-
Angiotensin aldosterone system
- RV:
-
Right ventricle antero-posterior dimension
- RWT:
-
Left ventricular relative wall thickness
- SGLT2:
-
Sodium-glucose co-transporter 2
- SV:
-
Stroke volume
- T2D:
-
Type 2 diabetes
- TAPSE:
-
Tricuspid annular plane systolic excursion
References
Anker SD, Chua TP, Ponikowski P, Harrington D, Swan JW, Kox WJ, Poole-Wilson PA, Coats AJ (1997) Hormonal changes and catabolic/anabolic imbalance in chronic heart failure and their importance for cardiac cachexia. Circulation 96(2):526–534
Baartscheer A, Schumacher CA, Wüst RC, Fiolet JW, Stienen GJ, Coronel R, Zuurbier CJ (2017) Empagliflozin decreases myocardial cytoplasmic Na+ through inhibition of the cardiac Na+/H+ exchanger in rats and rabbits. Diabetologia 60(3):568–573
Beresneva ON, Kulikov AN, Parastaeva MM, Okovityi SV, Ivkin DY, Zaraiskii M (2017) The influence of empagliflozin on microRNA-21 urinary expression in Wistar rats with left coronary ligation. Nephrol Dial Transplant 32(Suppl 3):iii613–iii614. https://doi.org/10.1093/ndt/gfx174.MP504
Cavaiola TS, Pettus J (2018) Cardiovascular effects of sodium glucose cotransporter 2 inhibitors. Diabetes Metab Syndr Obes 11:133–148
Boehringer Ingelheim Pharmaceuticals Inc. (2013) Pharmacology/toxicology NDA review and evaluation. NDA 204629
Cezar MD, Damatto RL, Pagan LU, Lima AR, Martinez PF, Bonomo C, Rosa CM, Campos DH, Cicogna AC, Gomes MJ, Oliveira SA Jr, Blotta DA, Okoshi MP, Okoshi K (2015) Early spironolactone treatment attenuates heart failure development by improving myocardial function and reducing fibrosis in spontaneously hypertensive rats. Cell Physiol Biochem 36(4):1453–1466
Connelly KA, Zhang Y, Visram A, Advani A, Batchu SN, Desjardins JF, Thai K, Gilbert RE (2019) Empagliflozin improves diastolic function in a nondiabetic rodent model of heart failure with preserved ejection fraction. JACC Basic Transl Sci 4(1):27–37
Empagliflozin outcome trial in patients with chronic heart failure with preserved ejection fraction (EMPEROR-Preserved). Clinicaltrials.gov. https://clinicaltrials.gov/ct2/show/NCT03057951?term=emperor&rank=2. Accessed 20 Feb 2017
Empagliflozin outcome trial in patients with chronic heart failure with reduced ejection fraction (EMPEROR-Reduced). Clinicaltrials.gov. https://clinicaltrials.gov/ct2/show/NCT03057977?term=emperor&rank=1. Accessed 20 Feb 2017
Gohlke P, Unger T (1995) Chronic low-dose treatment with perindopril improves cardiac function in stroke-prone spontaneously hypertensive rats by potentiation of endogenous bradykinin. 76(15):41E–45E
Gohlke P, Linz W, Schölkens BA, Kuwer I, Bartenbach S, Schnell A, Unger T (1994) Angiotensin-converting enzyme inhibition improves cardiac function. Role of bradykinin. Hypertension 23(4):411–418
Grempler R, Thomas L, Eckhardt M, Himmelsbach F, Sauer A, Sharp DE, Bakker RA, Mark M, Klein T, Eickelmann P (2012) Empagliflozin, a novel selective sodium glucose cotransporter-2 (SGLT-2) inhibitor: characterisation and comparison with other SGLT-2 inhibitors. Diabetes Obes Metab 14(1):83–90
Hayek T, Attias J, Coleman R, Brodsky S, Smith J, Breslow JL, Keidar S (1999) The angiotensin-converting enzyme inhibitor, fosinopril, and the angiotensin II receptor antagonist, losartan, inhibit LDL oxidation and attenuate atherosclerosis independent of lowering blood pressure in apolipoprotein E deficient mice. Cardiovasc Res 44:579–587
Heerspink HJ, Perkins BA, Fitchett DH, Husain M, Cherney DZ (2016) Sodium glucose cotransporter 2 inhibitors in the treatment of diabetes mellitus: cardiovascular and kidney effects, potential mechanisms, and clinical applications. Circulation. 134(10):752–772
Heidenreich P (2015) Heart failure prevention and team-based interventions. Heart Fail Clin 11(3):349–358
Joubert M, Jagu B, Montaigne D, Marechal X, Tesse A, Ayer A, Dollet L, Le May C, Toumaniantz G, Manrique A, Charpentier F, Staels B, Magré J, Cariou B, Prieur X (2017) The sodium-glucose cotransporter 2 inhibitor dapagliflozin prevents cardiomyopathy in a diabetic lipodystrophic mouse model. Diabetes 66(4):1030–1040
Kaplan A, Abidi E, El-Yazbi A, Eid A, Booz GW, Zouein FA (2018) Direct cardiovascular impact of SGLT2 inhibitors: mechanisms and effects. Heart Fail Rev 23(3):419–437 https://doi.org/10.1007/s10741-017-9665-9
Karpov AA, Ivkin DY, Dracheva AV, Pitukhina NN, Uspenskaya YK, Vaulina DD, Uskov IS, Eyvazova SD, Minasyan SM, Vlasov E, Buryakina AV, Galagudza MM (2014) Rat model of post-infarct heart failure by left coronary artery occlusion: technical aspects, functional and morphological assessment. Biomedicine 1:32–48
Kluger AY, Tecson KM, Lee AY, Lerma EV, Rangaswami J, Lepor NE, Cobble ME, McCullough PA (2019) Class effects of SGLT2 inhibitors on cardiorenal outcomes. Cardiovasc Diabetol 18(1):99
Konstam MA, Kramer DG, Patel AR, Maron MS, Udelson JE (2011) Left ventricular remodeling in heart failure: current concepts in clinical significance and assessment. JACC Cardiovasc Imaging 4(1):98–108
Kosiborod M, Cavender MA, Fu AZ, Wilding JP, Khunti K, Holl RW, Norhammar A, Birkeland KI, Jørgensen ME, Thuresson M, Arya N, Bodegård J, Hammar N, Fenici P (2017) CVD-REAL Investigators and Study Group. Lower risk of heart failure and death in patients initiated on sodium-glucose cotransporter-2 inhibitors versus other glucose-lowering drugs: the CVD-REAL study (comparative effectiveness of cardiovascular outcomes in new users of sodium-glucose cotransporter-2 inhibitors). Circulation 137(9):989–991
Kulikov AN, Okovityj SV, Ivkin DY, Karpov AA, Lisitsky DS, Lyubishin MM et al (2016) Effects of empagliflozin in an experimental model of chronic heart failure in normoglycemic rats. Russ Heart Fail J 17(6):454–460
Kulikov AA, Okovityi SV, Ivkin DY, Karpov AA, Lisitskyi DS, Lubishin MM, Alekseeva PA, Pitukhina NN, Smirnov AV, Kaiukov IG, Parusova EV (2017) Empagliflozin influence on the course of experimental heart failure in normoglycemic rats. Eur J Heart Fail 19–S1:165
Lee TM, Chang NC, Lin SZ (2017) Dapagliflozin, a selective SGLT2 inhibitor, attenuated cardiac fibrosis by regulating the macrophage polarization via STAT3 signaling in infarcted rat hearts. Free Radic Biol Med 104:298–310
Martens P, Mathieu C, Verbrugge FH (2017) Promise of SGLT2 inhibitors in heart failure: diabetes and beyond. Curr Treat Options Cardiovasc Med 19(3):23
McMurray JJV, DeMets DL, Inzucchi SE, Køber L, Kosiborod MN, Langkilde AM, Martinez FA, Bengtsson O, Ponikowski P, Sabatine MS, Sjöstrand M (2019) Solomon SD; DAPA-HF Committees and Investigators. The dapagliflozin and prevention of adverse-outcomes in heart failure (DAPA-HF) trial: baseline characteristics. Eur J Heart Fail 21(11):1402–1411
Natali A, Nesti L, Fabiani I, Calogero E, Di Bello V (2017) Impact of empagliflozin on subclinical left ventricular dysfunctions and on the mechanisms involved in myocardial disease progression in type 2 diabetes: rationale and design of the EMPA-HEART trial. Cardiovasc Diabetol 16(1):130
Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, Shaw W, Law G, Desai M, Matthews DR (2017) Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med 377(7):644–657
Nilsson KR, Duscha BD, Hranitzky PM, Kraus WE (2008) Chronic heart failure and exercise intolerance: the hemodynamic paradox. Curr Cardiol Rev 4(2):92–100
Okovityi SV, Beresneva ON, Parastaeva MM, Ivanova GT, Ivkin DY, Ivkina AS, Sipovsky VG, Zaraysky MI, Karpov AA, Kucher AG, Bogdanova EO, Sipovskaya EB, Kulikov AN, Kayukov IG (2018) Empagliflozin renal safety in normoglycemic rats failure. Nephrology (Saint-Petersburg) 22(1):83–90
Roger VL (2013) Epidemiology of heart failure. Circ Res 113(6):646–659
Santos-Gallego CG, Requena-Ibanez JA, San Antonio R, Ishikawa K, Watanabe S, Picatoste B, Flores E, Garcia-Ropero A, Sanz J, Hajjar RJ, Fuster V, Badimon JJ (2019) Empagliflozin ameliorates adverse left ventricular remodeling in nondiabetic heart failure by enhancing myocardial energetics. J Am Coll Cardiol 73(15):1931–1944
Vrhovac I, Balen Eror D, Klessen D, Burger C, Breljak D, Kraus O, Radović N, Jadrijević S, Aleksic I, Walles T, Sauvant C, Sabolić I, Koepsell H (2015) Localizations of Na(+)-D-glucose cotransporters SGLT1 and SGLT2 in human kidney and of SGLT1 in human small intestine, liver, lung, and heart. Pflugers Arch 467(9):1881–1898
Watanabe K, Ohta Y, Inoue M, Ma M, Wahed MI, Nakazawa M, Hasegawa G, Naito M, Fuse K, Ito M, Kato K, Hanawa H, Kodama M, Aizawa Y (2001) Bisoprolol improves survival in rats with heart failure. J Cardiovasc Pharmacol 38(Suppl 1):S55–S58
Xia A, Xue Z, Li Y, Wang W, Xia J, Wei T, Cao J, Zhou W (2014) Cardioprotective effect of betulinic acid on myocardial ischemia reperfusion injury in rats. Evid Based Complement Alternat Med 573745
Yurista SR, Sillje HHW, Oberdorf-Maass SU, Schouten EM, Pavez Giani MG, Hillebrands JL, van Goor H, van Veldhuisen DJ, de Boer RA, Westenbrink BD (2019) Sodium-glucose co-transporter 2 inhibition with empagliflozin improves cardiac function in non-diabetic rats with left ventricular dysfunction after myocardial infarction. Eur J Heart Fail 21(7):862–873 https://doi.org/10.1002/ejhf.1473
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, Broedl UC, Silvio E (2015) Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 373(22):2117–2128
Acknowledgments
We thank Kaiukov I.G., Beresneva O.N., and Galkina O.V. for their excellent technical assistance.
Funding
This work was supported by the St. Petersburg Chemical and Pharmaceutical University, Saint Petersburg, Russia.
Author information
Authors and Affiliations
Contributions
M. Krasnova: provision of study material, collection and assembly of data, data analysis and interpretation, and manuscript writing; A. Kulikov: conception and design, collection and assembly of data, data analysis and interpretation, and manuscript writing; S. Okovityi: conception and design, administrative support, data analysis, and interpretation; D. Ivkin: collection and assembly of data and data analysis; A. Smirnov: collection and assembly of data; A. Karpov: statistical data analysis and interpretation; E. Kaschina: data analysis and interpretation, manuscript writing advising, and final approval of manuscript. All authors read and approved the manuscript.
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Krasnova, M., Kulikov, A., Okovityi, S. et al. Comparative efficacy of empagliflozin and drugs of baseline therapy in post-infarct heart failure in normoglycemic rats. Naunyn-Schmiedeberg's Arch Pharmacol 393, 1649–1658 (2020). https://doi.org/10.1007/s00210-020-01873-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-020-01873-7