Abstract
Summary
A performance algorithm can be successfully used by bone density technologists at the time of a bone density test to identify patients with an indication for vertebral fracture assessment (VFA). Doing so appropriately increases physician prescription of fracture prevention medication.
Introduction
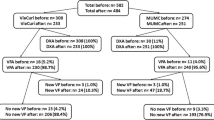
Densitometric spine imaging (vertebral fracture assessment, VFA) can identify prevalent vertebral fracture but is underutilized. We developed an algorithm by which DXA technologists identify patients for whom VFA should be performed. Following this algorithm, VFA was performed in patients whose lowest T-score (lumbar spine, total hip, or femoral neck) was between −1.5 and −2.4 inclusive and with one of the following: age, ≥65 years; height loss, ≥1.5 in.; or current systemic glucocorticoid therapy. Our main objectives were to assess change in VFA utilization at two other healthcare organizations after algorithm implementation, and to estimate the association of VFA results with prescription of fracture prevention medication.
Methods
The proportions of patients with an indication for VFA who had one performed before and after algorithm implementation were compared. Logistic regression was used to estimate the multivariable-adjusted association of VFA results with subsequent prescription of fracture prevention medication adjusted for healthcare organization (study site).
Results
After algorithm introduction, appropriate VFA use rose significantly Patients with a VFA positive for vertebral fracture had an odds ratio of 3.2 (95 % C.I., 2.1–5.1) for being prescribed new fracture prevention medication, adjusted for age, sex, prior clinical fracture, use of glucocorticoid medication, femoral neck bone mineral density T-score, and study site.
Conclusions
An algorithm to identify those for whom VFA is indicated can successfully be implemented by DXA technologists. Documentation of vertebral fracture increases prescription of fracture prevention medication for patients who otherwise lack an apparent indication for such therapy.

Similar content being viewed by others
References
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15:721–739
Black DM, Arden NK, Palermo L, Pearson J, Cummings SR (1999) Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of Osteoporotic Fractures Research Group. J Bone Miner Res 14:821–828
Ferrar L, Roux C, Felsenberg D, Gluer CC, Eastell R (2012) Association between incident and baseline vertebral fractures in European women: vertebral fracture assessment in the Osteoporosis and Ultrasound Study (OPUS). Osteoporos Int 23:59–65
Delmas PD, Genant HK, Crans GG, Stock JL, Wong M, Siris E, Adachi JD (2003) Severity of prevalent vertebral fractures and the risk of subsequent vertebral and nonvertebral fractures: results from the MORE trial. Bone 33:522–532
Melton LJ 3rd, Atkinson EJ, Cooper C, O'Fallon WM, Riggs BL (1999) Vertebral fractures predict subsequent fractures. Osteoporos Int 10:214–221
Siris ES, Genant HK, Laster AJ, Chen P, Misurski DA, Krege JH (2007) Enhanced prediction of fracture risk combining vertebral fracture status and BMD. Osteoporos Int 18:761–770
McCloskey EV, Vasireddy S, Threlkeld J, Eastaugh J, Parry A, Bonnet N, Beneton M, Kanis JA, Charlesworth D (2008) Vertebral fracture assessment (VFA) with a densitometer predicts future fractures in elderly women unselected for osteoporosis. J Bone Miner Res 23:1561–1568
Lindsay R, Silverman SL, Cooper C, Hanley DA, Barton I, Broy SB, Licata A, Benhamou L, Geusens P, Flowers K, Stracke H, Seeman E (2001) Risk of new vertebral fracture in the year following a fracture. Jama 285:320–323
Briggs AM, Greig AM, Wark JD (2007) The vertebral fracture cascade in osteoporosis: a review of aetiopathogenesis. Osteoporos Int 18:575–584
Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, Bauer DC, Genant HK, Haskell WL, Marcus R, Ott SM, Torner JC, Quandt SA, Reiss TF, Ensrud KE (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet 348:1535–1541
Melton LJ 3rd, Lane AW, Cooper C, Eastell R, O'Fallon WM, Riggs BL (1993) Prevalence and incidence of vertebral deformities. Osteoporos Int 3:113–119
Fink HA, Milavetz DL, Palermo L, Nevitt MC, Cauley JA, Genant HK, Black DM, Ensrud KE (2005) What proportion of incident radiographic vertebral deformities is clinically diagnosed and vice versa? J Bone Miner Res 20:1216–1222
Cooper C, Atkinson EJ, O'Fallon WM, Melton LJ 3rd (1992) Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985–1989. J Bone Miner Res 7:221–227
U.S. Preventive Services Task Force (2011) Screening for Osteoporosis: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med 154:356–364
National OF (2008) Clinician's Guide to Prevention and Treatment of Osteoporosis. In. National Osteoporosis Foundation
Leslie WD, Schousboe JT (2011) A review of osteoporosis diagnosis and treatment options in new and recently updated guidelines on case finding around the world. Curr Osteoporos Rep 9:129–140
Fuerst T, Wu C, Genant HK, von Ingersleben G, Chen Y, Johnston C, Econs MJ, Binkley N, Vokes TJ, Crans G, Mitlak BH (2009) Evaluation of vertebral fracture assessment by dual X-ray absorptiometry in a multicenter setting. Osteoporos Int 20:1199–1205
Hospers IC, van der Laan JG, Zeebregts CJ, Nieboer P, Wolffenbuttel BH, Dierckx RA, Kreeftenberg HG, Jager PL, Slart RH (2009) Vertebral fracture assessment in supine position: comparison by using conventional semiquantitative radiography and visual radiography. Radiology 251:822–828
Schousboe JT, Debold CR (2006) Reliability and accuracy of vertebral fracture assessment with densitometry compared to radiography in clinical practice. Osteoporos Int 17:281–289
Schousboe JT, Vokes T, Broy SB, Ferrar L, McKiernan F, Roux C, Binkley N (2008) Vertebral Fracture Assessment: the 2007 ISCD official positions. J Clin Densitom 11:92–108
Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC Jr, Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8:468–489
Greenspan SL, von Stetten E, Emond SK, Jones L, Parker RA (2001) Instant vertebral assessment: a noninvasive dual X-ray absorptiometry technique to avoid misclassification and clinical mismanagement of osteoporosis. J Clin Densitom 4:373–380
Schousboe JT, DeBold CR, Bowles C, Glickstein S, Rubino RK (2002) Prevalence of vertebral compression fracture deformity by X-ray absorptiometry of lateral thoracic and lumbar spines in a population referred for bone densitometry. J Clin Densitom 5:239–246
Olenginski TP, Newman ED, Hummel JL, Hummer M (2006) Development and evaluation of a vertebral fracture assessment program using IVA and its integration with mobile DXA. J Clin Densitom 9:72–77
Ostbye T, Yarnall KS, Krause KM, Pollak KI, Gradison M, Michener JL (2005) Is there time for management of patients with chronic diseases in primary care? Ann Fam Med 3:209–214
Bodenheimer T, Pham HH (2010) Primary care: current problems and proposed solutions. Health Aff (Millwood) 29:799–805
Yood RA, Mazor KM, Andrade SE, Emani S, Chan W, Kahler KH (2008) Patient decision to initiate therapy for osteoporosis: the influence of knowledge and beliefs. J Gen Intern Med 23:1815–1821
Solomon MD, Majumdar SR (2010) Primary non-adherence of medications: lifting the veil on prescription-filling behaviors. J Gen Intern Med 25:280–281
Solomon DH, Brookhart MA, Tsao P, Sundaresan D, Andrade SE, Mazor K, Yood R (2011) Predictors of very low adherence with medications for osteoporosis: towards development of a clinical prediction rule. Osteoporos Int 22:1737–1743
Silverman SL, Nasser K, Nattrass S, Drinkwater B (2012) Impact of bone turnover markers and/or educational information on persistence to oral bisphosphonate therapy: a community setting-based trial. Osteoporos Int 23:1069–1074
Kothawala P, Badamgarav E, Ryu S, Miller RM, Halbert RJ (2007) Systematic review and meta-analysis of real-world adherence to drug therapy for osteoporosis. Mayo Clin Proc 82:1493–1501
Schousboe JT, Davison ML, Dowd B, Thiede Call K, Johnson P, Kane RL (2011) Predictors of patients' perceived need for medication to prevent fracture. Med Care 49:273–280
Acknowledgments
This study was funded by the University of Minnesota and University of Clinical Translational Science Institutes T2 Partnership Collaborative Grant under grant number CTSI-OCEH-2010-001.
We would also like to acknowledge Derek E. Fuerbringer, CNMT, at the University of Wisconsin and Matthew K. Breitenstein, MS, at Park Nicollet Clinic for their work retrieving bone density and electronic health record data for this study.
Conflicts of interest
Dr. Schousboe is the president of the International Society for Clinical Densitometry; Dr. McKiernan received a research grant from OPKO Health, Alexion; Mr. Fuehrer has nothing to disclose; and Dr. Binkley received research support from Amgen, Lilly, Merck, OPKO. Advisory board, Merck, Lilly.
Author information
Authors and Affiliations
Corresponding author
Appendix: Diagnosis and procedure codes used to characterize the study population at all three institutions
Appendix: Diagnosis and procedure codes used to characterize the study population at all three institutions
Those who had a bone density test were identified in EHR billing record by a CPT-4 code for a bone density test using dual energy X-ray absorptiometry (76075 or 76076 between 1 July 2005 and 31 December 2006, and 77080 or 77081 between 1 January 2007 and 30 June 2010). Those who also had a VFA were identified from encounters that also had a CPT-4 billing code of 76077 (on or before 31 December 2006) or 77080 (after 1 January 2007).
Those who had a clinical vertebral fracture were identified by any outpatient encounter with the one of the following ICD-9 diagnosis codes, or any inpatient hospital stay with one of the following primary or secondary discharge codes;
-
(a)
Spine 805.2, 805.4, 805.8, 733.13
-
(b)
Hip 820–820.32, 733.14
-
(c)
Pelvis 805.6, 808.0, 808.2, 808.4x, 808.8
-
(d)
Proximal humerus 812.0x, 812.2x, 733.11
-
(e)
Distal radius 813.4x, 813.5x, 813.8x, 733.12.
Downstream utilization of additional spine imaging was identified in EHR billing records as any encounter with one of the following CPT-4 codes;
-
(a)
Thoracic spine radiographs: 72070, 72072,72074,72080
-
(b)
Lumbar spine radiographs: 72100, 72110, 72114, 72120
-
(c)
CT scan of thoracic spine: 72128, 72129, 72130,
-
(d)
CT scan of lumbar spine: 72131, 72132, 72133
-
(e)
MRI thoracic spine: 72146, 72147, 72157
-
(f)
MRI lumbar spine: 72148, 72149, 72158
Rights and permissions
About this article
Cite this article
Schousboe, J.T., McKiernan, F., Fuehrer, J.T. et al. Use of a performance algorithm improves utilization of vertebral fracture assessment in clinical practice. Osteoporos Int 25, 965–972 (2014). https://doi.org/10.1007/s00198-013-2519-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-013-2519-y