Abstract
Summary
Although the presence of metabolic syndrome (MetS) and increasing numbers of MetS components were associated with attenuated bone loss at various skeletal sites in postmenopausal women, this beneficial effect of MetS on bone mass can be mainly explained by higher mechanical loading in the affected subjects.
Introduction
Previous cross-sectional epidemiological studies reported the inconsistent results regarding the combined effects of MetS on bone mass. In our present report, we performed a large, longitudinal study to evaluate MetS in relation to annualized bone mineral density (BMD) changes in postmenopausal Korean women.
Methods
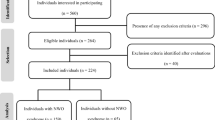
The study cohort consisted of 1,218 postmenopausal women who had undergone comprehensive routine health examinations with an average follow-up interval of 3 years. The BMD at the lumbar spine and proximal femur sites was measured with dual-energy X-ray absorptiometry using the same equipment at baseline and at follow-up.
Results
Following adjustment for age, baseline BMD, and lifestyle factors, the women with MetS had 21.7, 17.0, 26.7, and 31.1 % less bone loss at the total femur, femur neck, trochanter, and lumbar spine, respectively, compared with MetS-free women (P = 0.004 to 0.041). Consistently, the rates of bone loss at all skeletal sites were linearly attenuated with increasing numbers of MetS components (P = 0.004 to <0.001). Importantly, when weight and height were added as confounding factors, the differences and trends of annualized BMD changes according to the MetS status disappeared.
Conclusion
Our current results indicate that the beneficial effects of MetS on bone mass can be mainly explained by higher mechanical loading in the affected subjects. Consequently, MetS per se may not be a meaningful concept for predicting future bone loss and for explaining associations between osteoporosis and cardiovascular diseases.

Similar content being viewed by others
References
Kado DM, Browner WS, Blackwell T, Gore R, Cummings SR (2000) Rate of bone loss is associated with mortality in older women: a prospective study. J Bone Miner Res 15:1974–1980
von der Recke P, Hansen MA, Hassager C (1999) The association between low bone mass at the menopause and cardiovascular mortality. Am J Med 106:273–278
Tanko LB, Christiansen C, Cox DA, Geiger MJ, McNabb MA, Cummings SR (2005) Relationship between osteoporosis and cardiovascular disease in postmenopausal women. J Bone Miner Res 20:1912–1920
Szulc P, Garnero P, Claustrat B, Marchand F, Duboeuf F, Delmas PD (2002) Increased bone resorption in moderate smokers with low body weight: the Minos study. J Clin Endocrinol Metab 87:666–674
Fink HA, Ewing SK, Ensrud KE, Barrett-Connor E, Taylor BC, Cauley JA, Orwoll ES (2006) Association of testosterone and estradiol deficiency with osteoporosis and rapid bone loss in older men. J Clin Endocrinol Metab 91:3908–3915
Koh JM, Khang YH, Jung CH, Bae S, Kim DJ, Chung YE, Kim GS (2005) Higher circulating hsCRP levels are associated with lower bone mineral density in healthy pre- and postmenopausal women: evidence for a link between systemic inflammation and osteoporosis. Osteoporos Int 16:1263–1271
Almeida M, Han L, Martin-Millan M et al (2007) Skeletal involution by age-associated oxidative stress and its acceleration by loss of sex steroids. J Biol Chem 282:27285–27297
Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, Salonen JT (2002) The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA 288:2709–2716
Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, Taskinen MR, Groop L (2001) Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 24:683–689
Barrett-Connor E, Kritz-Silverstein D (1996) Does hyperinsulinemia preserve bone? Diabetes Care 19:1388–1392
Kinjo M, Setoguchi S, Solomon DH (2007) Bone mineral density in adults with the metabolic syndrome: analysis in a population-based U.S. sample. J Clin Endocrinol Metab 92:4161–4164
Hernandez JL, Olmos JM, Pariente E, Martinez J, Valero C, Garcia-Velasco P, Nan D, Llorca J, Gonzalez-Macias J (2010) Metabolic syndrome and bone metabolism: the Camargo Cohort study. Menopause 17:955–961
von Muhlen D, Safii S, Jassal SK, Svartberg J, Barrett-Connor E (2007) Associations between the metabolic syndrome and bone health in older men and women: the Rancho Bernardo Study. Osteoporos Int 18:1337–1344
Hwang DK, Choi HJ (2010) The relationship between low bone mass and metabolic syndrome in Korean women. Osteoporos Int 21:425–431
Ravn P, Cizza G, Bjarnason NH, Thompson D, Daley M, Wasnich RD, McClung M, Hosking D, Yates AJ, Christiansen C (1999) Low body mass index is an important risk factor for low bone mass and increased bone loss in early postmenopausal women. Early Postmenopausal Intervention Cohort (EPIC) study group. J Bone Miner Res 14:1622–1627
Smith BJ, Lerner MR, Bu SY, Lucas EA, Hanas JS, Lightfoot SA, Postier RG, Bronze MS, Brackett DJ (2006) Systemic bone loss and induction of coronary vessel disease in a rat model of chronic inflammation. Bone 38:378–386
Kim BJ, Yu YM, Kim EN, Chung YE, Koh JM, Kim GS (2007) Relationship between serum hsCRP concentration and biochemical bone turnover markers in healthy pre- and postmenopausal women. Clin Endocrinol (Oxf) 67:152–158
Grundy SM, Cleeman JI, Daniels SR et al (2005) Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 112:2735–2752
Ahmed LA, Schirmer H, Berntsen GK, Fønnebø V, Joakimsen RM (2006) Features of the metabolic syndrome and the risk of non-vertebral fractures: the Tromsø study. Osteoporos Int 17:426–432
Felson DT, Zhang Y, Hannan MT, Anderson JJ (1993) Effects of weight and body mass index on bone mineral density in men and women: the Framingham study. J Bone Miner Res 8:567–573
Edelstein SL, Barrett-Connor E (1993) Relation between body size and bone mineral density in elderly men and women. Am J Epidemiol 138:160–169
Stolk RP, Van Daele PL, Pols HA, Burger H, Hofman A, Birkenhager JC, Lamberts SW, Grobbee DE (1996) Hyperinsulinemia and bone mineral density in an elderly population: the Rotterdam Study. Bone 18:545–549
Nelson LR, Bulun SE (2001) Estrogen production and action. J Am Acad Dermatol 45:S116–S124
Ohta H, Ikeda T, Masuzawa T, Makita K, Suda Y, Nozawa S (1993) Differences in axial bone mineral density, serum levels of sex steroids, and bone metabolism between postmenopausal and age- and body size-matched premenopausal subjects. Bone 14:111–116
Reid I, Richards JB (2009) Adipokine effects on bone. Clin Rev Bone Miner Metab 7:240–248
Biver E, Salliot C, Combescure C, Gossec L, Hardouin P, Legroux-Gerot I, Cortet B (2011) Influence of adipokines and ghrelin on bone mineral density and fracture risk: a systematic review and meta-analysis. J Clin Endocrinol Metab 96:2703–2713
Yatagai T, Nagasaka S, Taniguchi A, Fukushima M, Nakamura T, Kuroe A, Nakai Y, Ishibashi S (2003) Hypoadiponectinemia is associated with visceral fat accumulation and insulin resistance in Japanese men with type 2 diabetes mellitus. Metabolism 52:1274–1278
Nakashima R, Kamei N, Yamane K, Nakanishi S, Nakashima A, Kohno N (2006) Decreased total and high molecular weight adiponectin are independent risk factors for the development of type 2 diabetes in Japanese-Americans. J Clin Endocrinol Metab 91:3873–3877
Badman MK, Flier JS (2007) The adipocyte as an active participant in energy balance and metabolism. Gastroenterology 132:2103–2115
Kern PA, Ranganathan S, Li C, Wood L, Ranganathan G (2001) Adipose tissue tumor necrosis factor and interleukin-6 expression in human obesity and insulin resistance. Am J Physiol Endocrinol Metab 280:E745–E751
Berg AH, Scherer PE (2005) Adipose tissue, inflammation, and cardiovascular disease. Circ Res 96:939–949
Gabay C, Kushner I (1999) Acute-phase proteins and other systemic responses to inflammation. N Engl J Med 340:448–454
Sivas F, Alemdaroglu E, Elverici E, Kulug T, Ozoran K (2009) Serum lipid profile: its relationship with osteoporotic vertebrae fractures and bone mineral density in Turkish postmenopausal women. Rheumatol Int 29:885–890
Yamaguchi T, Sugimoto T, Yano S, Yamauchi M, Sowa H, Chen Q, Chihara K (2002) Plasma lipids and osteoporosis in postmenopausal women. Endocr J 49:211–217
Xu S, Yu JJ (2006) Beneath the minerals, a layer of round lipid particles was identified to mediate collagen calcification in compact bone formation. Biophys J 91:4221–4229
Szulc P, Varennes A, Delmas PD, Goudable J, Chapurlat R (2010) Men with metabolic syndrome have lower bone mineral density but lower fracture risk–the MINOS study. J Bone Miner Res 25:1446–1454
Green S, Anstiss CL, Fishman WH (1971) Automated differential isoenzyme analysis. II. The fractionation of serum alkaline phosphatases into “liver”, “intestinal” and “other” components. Enzymologia 41:9–26
van Straalen JP, Sanders E, Prummel MF, Sanders GT (1991) Bone-alkaline phosphatase as indicator of bone formation. Clin Chim Acta 201:27–33
Acknowledgments
This study was supported by grants from the Korea Health Technology R&D Project and the National Project for Personalized Genomic Medicine, Ministry of Health & Welfare, Republic of Korea (project numbers A110536 and A111218-GM03, respectively).
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Figure 1
Annualized serum total ALP changes according to the MetS status. Multivariate-adjusted least-square mean (± standard error) annualized serum total ALP changes were generated by analysis of covariance (ANCOVA) after adjustment for confounders. The multivariable adjustment model included age, smoking and drinking habits, exercise habits, and dairy consumption. The final adjustment model included weight and height, as well as factors from the multivariable adjustment model. MetS, metabolic syndrome; ALP, alkaline phosphatase; Wt, weight; Ht, height. (JPEG 24 kb)
ESM 2
(DOCX 30 kb)
Rights and permissions
About this article
Cite this article
Kim, BJ., Ahn, S.H., Bae, S.J. et al. Association between metabolic syndrome and bone loss at various skeletal sites in postmenopausal women: a 3-year retrospective longitudinal study. Osteoporos Int 24, 2243–2252 (2013). https://doi.org/10.1007/s00198-013-2292-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-013-2292-y