Abstract
Introduction and hypothesis
Low anesthetic bladder capacity has been shown to be a biomarker for bladder-centric interstitial cystitis/bladder pain syndrome (IC/BPS). The goal of this study was to determine if histopathological evidence from bladder biopsies supports anesthetic bladder capacity (BC) as a marker to distinguish a bladder-centric IC/BPS subtype.
Methods
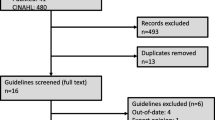
From a review of our large IC/BPS cohort of patients undergoing hydrodistention, we identified a total of 41 patients with low BC (≤ 400 ml); an additional 41 consecutive patients with BC > 400 ml were selected as the comparator group. The original bladder mucosal biopsy pathology slides were re-reviewed by a single pathologist (blinded to patient information) using a standardized grading scale developed for this study.
Results
Histologically, the low BC subjects exhibited higher levels of acute inflammation (p = 0.0299), chronic inflammation (p = 0.0139), and erosion on microscopy (p = 0.0155); however, there was no significant difference in mast cell count between groups (p = 0.4431). There was no significant gender difference between the groups; female patients were the majority in both groups (low BC: 94.12%, non-low BC: 100%; p = 0.1246). Individuals in the low BC group were older (p < 0.0001), had a higher incidence of Hunner’s lesions on cystoscopy (p < 0.0001), and had significantly higher scores, i.e., more bother symptoms, on two IC/BPS questionnaires (ICPI, p = 0.0154; ICSI, p = 0.0005).
Conclusions
IC/BPS patients with low anesthetic bladder capacity have histological evidence of significantly more acute and chronic inflammation compared with patients with a non-low bladder capacity. These data provide additional evidence to support low bladder capacity as a marker of a distinct bladder-centric IC/BPS phenotype.

Similar content being viewed by others
References
Walker SJ, Zambon J, Andersson K-E, et al. Bladder capacity is a biomarker for a bladder centric versus systemic manifestation in interstitial cystitis/bladder pain syndrome. J Urol. 2017;198(2):369–75.
Hanno PM, Erickson D, Moldwin R, Faraday MM. American urological association. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome: AUA guideline amendment. J Urol. 2015;193(5):1545–53.
Berry SH, Elliott MN, Suttorp M, et al. Prevalence of symptoms of bladder pain syndrome/interstitial cystitis among adult females in the United States. J Urol. 2011;186(2):540–4.
Hanno PM, Burks DA, Clemens JQ, et al. AUA guideline for the diagnosis and treatment of interstitial cystitis/bladder pain syndrome. J Urol. 2011;185(6):2162–70.
Barr S. Diagnosis and management of interstitial cystitis. Obstet Gynecol Clin N Am. 2014;41(3):397–407.
Quillin RB, Erickson DR. Management of interstitial cystitis/bladder pain syndrome. Urol Clin North Am. 2012;39(3):389–96.
Hohenfellner M, Black P, Linn JF, Dahms SE, Thüroff JW. Surgical treatment of interstitial cystitis in women. Int Urogynecol J Pelvic Floor Dysfunct. 2000;11(2):113–9.
Colaco M, Koslov DS, Keys T, et al. Correlation of gene expression with bladder capacity in interstitial cystitis/bladder pain syndrome. J Urol. 2014;192(4):1123–9.
Tomaszewski JE, Landis JR, Russack V, et al. Biopsy features are associated with primary symptoms in interstitial cystitis: results from the interstitial cystitis database study. Urology. 2001 Jun 1;57(6):67–81.
O’Leary MP, Sant GR, Fowler FJ, Whitmore KE, Spolarich-Kroll J. The interstitial cystitis symptom index and problem index. Urology. 1997;49(5A Suppl):58–63.
Parsons CL, Dell J, Stanford EJ, et al. Increased prevalence of interstitial cystitis: previously unrecognized urologic and gynecologic cases identified using a new symptom questionnaire and intravesical potassium sensitivity. Urology. 2002;60(4):573–8.
Mazeaud C, Rigaud J, Levesque A, et al. Stratification of patients with interstitial cystitis/bladder pain syndrome according to the anatomical bladder capacity. Urology. 2018.
Buckley M, Walls AF. Identification of mast cells and mast cell subpopulations. Methods in molecular medicine 2008; 285–97.
Walls AF, Amalinei C. Detection of mast cells and basophils by immunohistochemistry. 2014; 117–34.
Atiakshin D, Samoilova V, Buchwalow I, Boecker W, Tiemann M. Characterization of mast cell populations using different methods for their identification. Histochem Cell Biol. 2017;147(6):683–94.
Sant GR, Kempuraj D, Marchand JE, Theoharides TC. The mast cell in interstitial cystitis: role in pathophysiology and pathogenesis. Urology. 2007;69(4):S34–40.
Kim A, Han J-Y, Ryu C-M, et al. Histopathological characteristics of interstitial cystitis/bladder pain syndrome without Hunner lesion. Histopathology. 2017;71(3):415–24.
Logadottir Y, Delbro D, Lindholm C, Fall M, Peeker R. Inflammation characteristics in bladder pain syndrome ESSIC type 3C/classic interstitial cystitis. Int J Urol. 2014;21:75–8.
Larsen MS, Mortensen S, Nordling J, Horn T. Quantifying mast cells in bladder pain syndrome by immunohistochemical analysis. BJU Int. 2008;102(2):204–7.
Kastrup J, Hald T, Larsen S, Nielsen VG. Histamine content and mast cell count of detrusor muscle in patients with interstitial cystitis and other types of chronic cystitis. Br J Urol. 1983;55(5):495–500.
Patnaik SS, Laganà AS, Vitale SG, et al. Etiology, pathophysiology and biomarkers of interstitial cystitis/painful bladder syndrome. Arch Gynecol Obstet. 2017;295(6):1341–59.
Gamper M, Regauer S, Welter J, Eberhard J, Viereck V. Are mast cells still good biomarkers for bladder pain syndrome/interstitial cystitis? J Urol. 2015;193(6):1994–2000.
Richter B, Hesse U, Hansen AB, et al. Bladder pain syndrome/interstitial cystitis in a Danish population: a study using the 2008 criteria of the European Society for the Study of interstitial cystitis. BJU Int. 2010;105(5):660–7.
Liu H-T, Shie J-H, Chen S-H, Wang Y-S, Kuo H-C. Differences in mast cell infiltration, e-cadherin, and zonula occludens-1 expression between patients with overactive bladder and interstitial cystitis/bladder pain syndrome. Urology. 2012;80(1):225.e13–8.
Hanno P, Levin RM, Monson FC, et al. Diagnosis of interstitial cystitis. J Urol. 1990;143(2):278–81.
Akiyama Y, Homma Y, Maeda D. Pathology and terminology of interstitial cystitis/bladder pain syndrome: a review. Histol Histopathol 2018;18028.
Akiyama Y, Maeda D, Morikawa T, et al. Digital quantitative analysis of mast cell infiltration in interstitial cystitis. Neurourol Urodyn. 2018;37(2):650–7.
Acknowledgements
The authors thank the study participants. Funding for this study was provided, in part, by the Interstitial Cystitis Association (2014 Pilot Research Program Grant Award; SJW) and the NIDDK (R21DK106554-01; SJW).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schachar, J.S., Evans, R.J., Parks, G.E. et al. Histological evidence supports low anesthetic bladder capacity as a marker of a bladder-centric disease subtype in interstitial cystitis/bladder pain syndrome. Int Urogynecol J 30, 1863–1870 (2019). https://doi.org/10.1007/s00192-019-04038-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-04038-0