Abstract
Introduction and hypothesis
Posterior deep infiltrating endometriosis (DIE) has been associated with pelvic floor muscle (PFM) alteration and voiding dysfunction (VD). The aim of this study is to evaluate the correlation between the presence of VD and altered PFM morphometry, objectively evaluated using 3D/4D transperineal ultrasound at rest and during dynamic maneuvers, in patients with posterior DIE.
Methods
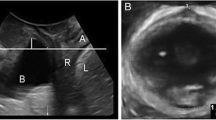
A prospective study was conducted on 108 symptomatic women scheduled for surgical removal of posterior DIE. The study population was divided in two groups according to presence or absence of VD on the Bristol Female Lower Urinary Tract Symptoms (BFLUTS). A 3D/4D transperineal ultrasound was performed to compare the following PFM morphometric parameters: levator hiatus area (LHA), antero-posterior (AP) and left-right (LR) diameters and levator ani muscle (LAM) coactivation. LAM coactivation was defined as the paradoxical contraction of the pelvic floor muscle during the Valsalva maneuver causing a smaller LHA than in the resting state.
Results
Forty-eight (45.2%) women presented VD, while 60 (54.8%) women did not report any voiding complaints. Baseline characteristics did not significantly differ between the two groups. We did not find any significant statistical differences in PFM parameters between the two groups, except for a higher rate of levator ani muscle coactivation in women with VD compared with women without VD [64.6% (31/48) versus 31.7% (19/60), respectively; p = < 0.001].
Conclusions
In women affected by posterior DIE, LAM coactivation at 3D/4D transperineal ultrasound seems to be more frequent in patients with than without VD.

Similar content being viewed by others
References
Vercellini P, Viganò P, Somigliana E, Fedele L. Endometriosis: pathogenesis and treatment. Nat Rev Endocrinol. 2014;10(5):261–75.
Chapron C, Fauconnier A, Vieira M, et al. Anatomical distribution of deeply infiltrating endometriosis: surgical implications and proposition for a classification. Hum Reprod. 2003;18:157–61.
Spagnolo E, Zannoni L, Raimondo D, Ferrini G, Mabrouk M, Benfenati A, et al. Urodynamic evaluation and anorectal manometry pre- and post-operative bowel shaving surgical procedure for posterior deep infiltrating endometriosis: a pilot study. J Minim Invasive Gynecol. 2014;21(6):1080–5.
Daräi E, Marpeau O, Thomassin I, Dubernard G, Barranger E, Bazot M. Fertility after laparoscopic colorectal resection for endometriosis: preliminary results. Fertil Steril. 2005;84:945–50.
Chapron C, Chopin N, Borghese B, Foulot H, Dousset B, Vacher-Lavenu MC, et al. Deeply infiltrating endometriosis: pathogenetic implications of the anatomical distribution. Hum Reprod. 2006;21(7):1839–45.
Serati M, Cattoni E, Braga A, Uccella S, Cromi A, Ghezzi F. Deep endometriosis and bladder and detrusor functions in women without urinary symptoms: a pilot study through an unexplored world. Fertil Steril. 2013;100(5):1332–6.
Riiskjaer M, Greisen S, Glavind-Kristensen M, Kesmodel US, Forman A, Seyer-Hansen M. Pelvic organ function before and after laparoscopic bowel resection for rectosigmoid endometriosis: a prospective, observational study. BJOG. 2016;123(8):1360–7.
de Lapasse C, Renouvel F, Chis C, Grosdemouge I, Panel P. Évaluation fonctionnelle urinaire et urodynamique préopératoire des patientes présentant une endométriose profonde pelviennechirurgicale: à propos de 12 cas. Gynécologie Obstétrique & Fertilité. 2008;36(3):272–7.
Ballester M, Dubernard G, Wafo E, Bellon L, Amarenco G, Belghiti J, et al. Evaluation of urinary dysfunction by urodynamic tests, electromyography and quality of life questionnaire before and after surgery for deep infiltrating endometriosis. Eur J Obstet Gynecol Reprod Biol. 2014;179:135–40.
Ballester M, Santulli P, Bazot M, Coutant C, Rouzier R, Daraï E. Preoperative evaluation of posterior deep-infiltrating endometriosis demonstrates a relationship with urinary dysfunction and parametrial involvement. J Minim Invasive Gynecol. 2011;18(1):36–42.
Anaf V, Simon P, El Nakadi I, Fayt I, Buxant F, Simonart T, et al. Relationship between endometriotic foci and nerves in rectovaginal endometriotic nodules. Hum Reprod. 2000;15(8):1744–50.
Howard FM. Endometriosis and mechanisms of pelvic pain. J Minim Invasive Gynecol. 2009;16(5):540–50.
Mohamed M, Diego R, Simona DF, et al. Pelvic floor muscle assessment at 3-and 4-dimensional transperineal ultrasound in women with endometriosis, with or without retroperitoneal infiltration: a step towards complete functional assessment: perineum and DIE. Ultrasound Obstet Gynecol. 2017. https://doi.org/10.1002/uog.18924.
Raimondo D, Youssef A, Mabrouk M, Del Forno S, Martelli V, Pilu G, et al. Pelvic floor muscle dysfunction on 3D/4D transperineal ultrasound in patients with deep infiltrating endometriosis: a pilot study: PFM dysfunction and DIE. Ultrasound Obstet Gynecol. 2017;50(4):527–32.
dos Bispo APS, Ploger C, Loureiro AF, Sato H, Kolpeman A, Girão MJBC, et al. Assessment of pelvic floor muscles in women with deep endometriosis. Arch Gynecol Obstet. 2016;294(3):519–23.
Kuo TLC, Ng LG, Chapple CR. Pelvic floor spasm as a cause of voiding dysfunction. Curr Opin Urol. 2015;25(4):311–6.
Faubion SS, Shuster LT, Bharucha AE. Recognition and management of nonrelaxing pelvic floor dysfunction. Mayo Clin Proc. 2012;87(2):187–93.
Artibani W, Cerruto MA. Dysfunctional voiding. Curr Opin Urol. 2014;24(4):330–5.
Youssef A, Montaguti E, Sanlorenzo O, Cariello L, Salsi G, Morganelli G, et al. Reliability of new three-dimensional ultrasound technique for pelvic hiatal area measurement. Ultrasound Obstet Gynecol. 2016;47(5):629–35.
Dietz HP. Pelvic floor ultrasound: a review. Clin Obstet Gynecol. 2017;60(1):58–81.
Jackson S, Donovan J, Brookes S, Eckford S, Swithinbank L, Abrams P. The Bristol female lower urinary tract symptoms questionnaire: development and psychometric testing. Br J Urol. 1996;77(6):805–12.
Brookes ST, Donovan JL, Wright M, Jackson S, Abrams P. A scored form of the Bristol female lower urinary tract symptoms questionnaire: data from a randomized controlled trial of surgery for women with stress incontinence. Am J Obstet Gynecol. 2004;191(1):73–82.
Raizada V, Bhargava V, Jung S-A, Karstens A, Pretorius D, Krysl P, et al. Dynamic assessment of the vaginal high-pressure zone using high-definition manometery, 3-dimensional ultrasound, and magnetic resonance imaging of the pelvic floor muscles. Am J Obstet Gynecol. 2010;203(2):172.e1–8.
Örnö AK, Dietz HP. Levator co-activation is a significant confounder of pelvic organ descent on Valsalva maneuver. Ultrasound Obstet Gynecol. 2007;30(3):346–50.
Panel P, Huchon C, Estrade-Huchon S, Le Tohic A, Fritel X, Fauconnier A. Bladder symptoms and urodynamic observations of patients with endometriosis confirmed by laparoscopy. Int Urogynecol J. 2016;27(3):445–51.
de Resende Júnior JAD, Crispi CP, Cardeman L, Buere RT, de Fonseca MF. Urodynamic observations and lower urinary tract symptoms associated with endometriosis: a prospective cross-sectional observational study assessing women with deep infiltrating disease. Int Urogynecol J. 2018;29(9):1349–58.
Bonneau C, Zilberman S, Ballester M, Thomin A, Thomassin-Naggara I, Bazot M, et al. Incidence of pre- and postoperative urinary dysfunction associated with deep infiltrating endometriosis: relevance of urodynamic tests and therapeutic implications. Minerva Ginecol. 2013;65(4):385–405.
FitzGerald MP, Kotarinos R. Rehabilitation of the short pelvic floor. I: Background and patient evaluation. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(4):261–8.
Butrick CW. Patients with chronic pelvic pain: endometriosis or interstitial cystitis/painful bladder syndrome? JSLS. 2007;11(2):182–9.
Groutz A, Blaivas JG. Non-neurogenic female voiding dysfunction. Curr Opin Urol. 2002;12(4):311–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mabrouk, M., Raimondo, D., Parisotto, M. et al. Pelvic floor dysfunction at transperineal ultrasound and voiding alteration in women with posterior deep endometriosis. Int Urogynecol J 30, 1527–1532 (2019). https://doi.org/10.1007/s00192-019-03963-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-03963-4