Abstract
Introduction and hypothesis
Most synthetic meshes used in transvaginal surgery are made of polypropylene, which has a stable performance, but does not easily degrade in vivo. However, mesh-related complications are difficult to address and have raised serious concerns. A new biomaterial mesh with good tissue integration and few mesh-related complications is needed. To evaluate the effect of a new bacterial cellulose (BC) mesh on pelvic floor reconstruction following implantation in the vagina of sheep after 1 and 12 weeks.
Methods
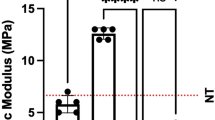
The meshes were implanted in the submucosa of the posterior vagina wall of sheep. At 1 and 12 weeks after surgery, mesh–tissue complex (MTC) specimens were harvested for histological studies and biomechanical evaluation. At 12 weeks after surgery, MTC specimens were biomechanically assessed by a uniaxial tension “pulley system”.
Results
The BC mesh elicited a higher inflammatory response than Gynemesh™PS at both 1 and 12 weeks after implantation. Twelve weeks after implantation, the BC mesh resulted in less fibrosis than Gynemesh™PS. Compared with the Gynemesh™PS group, the BC mesh group had increased mRNA expression of MMP-1, MMP-2, and MMP-9 (P < 0.05), but decreased expression of the anti-inflammatory factor IL-4 (P < 0.05). Twelve weeks after implantation, the ultimate load and maximum elongation percentage of the BC mesh were significantly lower than those of Gynemesh™PS.
Conclusions
The BC mesh could not be a promising biomaterial for pelvic floor reconstructive surgery unless the production process and parameters were improved.






Similar content being viewed by others
References
Amrute KV, Eisenberg ER, Rastinehad AR, Kushner L, Badlani GH. Analysis of outcomes of single polypropylene mesh in total pelvic floor reconstruction. Neurourol Urodyn. 2007;26(1):53–8.
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson Funk M. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201–6.
Barber MD, Brubaker L, Burgio KL, Richter HE, Nygaard I, Weidner AC, et al. Comparison of 2 transvaginal surgical approaches and perioperative behavioral therapy for apical vaginal prolapse. JAMA. 2014;311(10):1023.
Klosterhalfen B, Klinge U, Henze U, Bhardwaj R, Conze J, Schumpelick V. Morphologische Korrelation der funktioneuen Bauchwandmechanik nach Mesh-implantation. Langenbecks Arch Chir. 1997;382:87–94.
Margulies RU, Lewicky-Gaupp C, Fenner DE, Mcguire EJ, Clemens JQ. Complications requiring reoperation following vaginal mesh kit procedures for prolapse. Am J Obstet Gynecol. 2008;199(6):678.e1–4.
Baessler K, Maher CF. Mesh augmentation during pelvic-floor reconstructive surgery: risks and benefits. Curr Opin Obstet Gynecol. 2006;18(5):560–6.
Falconer C, Söderberg M, Blomgren B, Ulmsten U. Influence of different sling materials on connective tissue metabolism in stress urinary incontinent women. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(Suppl 2):S19–23.
Karlovsky ME, Thakre AA, Rastinehad A, Kushner L, Badlani GH. Biomaterials for pelvic floor reconstruction. Urology. 2005;66(3):469–75.
Shankaran V, Weber DJ, Reed RL, Luchette FA. A review of available prosthetics for ventral hernia repair. Ann Surg. 2011;253(1):16–26.
Lucyszyn N, Ono L, Lubambo AF, Woehl MA, Sens CV, de Souza CF, et al. Physicochemical and in vitro biocompatibility of films combining reconstituted bacterial cellulose with arabinogalactan and xyloglucan. Carbohyd Polym. 2016;151:889–98.
Phisalaphong M, Jatupaiboon N. Biosynthesis and characterization of bacteria cellulose-chitosan film. Carbohydr Polym. 2008;74:482–8.
Ma X, Zhang H, Chen SW. Feasibility of bacterial cellulose membrane as a wound dressing. J Clin Rehab Tissue Eng Res. 2010;14:2261–4.
Xu C, Ma X, Chen S, Tao M, Yuan L. Bacterial cellulose membranes used as artificial substitutes for Dural defection in rabbits. Int J Mol Sci. 2014;15(6):10855–67.
Zang S, Zhang R, Chen H, Lu Y, Zhou J. Investigation on artificial blood vessels prepared from bacterial cellulose. Mater Sci Eng C Mater Biol Appl. 2015;46:111–7.
Abramowitch SD, Feola A, Jallah Z, Moalli PA. Tissue mechanics, animal models, and pelvic organ prolapse: a review. Eur J Obstet Gynecol Reprod Biol. 2009;144:S146–58.
Krause H, Goh J. Sheep and rabbit genital tracts and abdominal wall as an implantation model for the study of surgical mesh. J Obstet Gynaecol Res. 2009;35(2):219–24.
Couri BM, Lenis AT, Borazjani A, Paraiso MFR, Damaser MS. Animal models of female pelvic organ prolapse: lessons learned. Expert Rev Obstet Gynecol. 2014;7(3):249–60.
Jackson R, Hilson RP, Roe AR, Perkins N, Heuer C, West DM. Epidemiology of vaginal prolapse in mixed-age ewes in New Zealand. N Z Vet J. 2014;62(6):328–37.
Hjort H, Mathisen T, Alves A, Clermont G, Boutrand JP. Three-year results from a preclinical implantation study of a long-term resorbable surgical mesh with time-dependent mechanical characteristics. Hernia. 2012;16(2):191–7.
Junqueira LC, Cossermelli W, Brentani R. Differential staining of collagens type I, II and III by Sirius red and polarization. Arch Histol Jpn. 1978;41(3):267–74.
Bellón JM, Contreras LA, Buján J, Palomares D, Carrera-San Mart NA. Tissue response to polypropylene meshes used in the repair of abdominal wall defects. Biomaterials. 1998;19(7):669–75.
Gigliobianco G, Roman Regueros S, Osman NI, Bissoli J, Bullock AJ, Chapple CR, et al. Biomaterials for pelvic floor reconstructive surgery: how can we do better? Biomed Res Int. 2015;2015:968087. https://doi.org/10.1155/2015/968087.
Moore RD, Lukban JC. Comparison of vaginal mesh extrusion rates between a lightweight type I polypropylene mesh versus heavier mesh in the treatment of pelvic organ prolapse. Int Urogynecol J. 2012;23(10):1379–86.
Patel H, Ostergard DR, Sternschuss G. Polypropylene mesh and the host response. Int Urogynecol J. 2012;23(6):669–79.
Amid PK. Classification of biomaterials and their related complications in abdominal wall hernia surgery. Hernia. 1997;1:15–21.
Miyamoto T, Takahashi S-i, Ito H, Inagak H. Tissue biocompatibility of cellulose and its derivatives. J Biomed Mater Res. 1989;23:125–33.
Helenius G, Backdahl H, Bodin A, Nannmark U, Gatenholm P, Risberg B. In vivo biocompatibility of bacterial cellulose. J Biomed Mater Res A. 2006;76(2):431–8.
Asarias JR, Nguyen PT, Mings JR, Gehrich AP, Pierce LM. Influence of mesh materials on the expression of mediators involved in wound healing. J Investig Surg. 2011;24(2):87–98.
Ulrich D, Edwards SL, Letouzey V, et al. Regional variation in tissue composition and biomechanical properties of postmenopausal ovine and human vagina. PLoS One. 2014;9(8):e104972.
Liang R, Abramowitch S, Knight K, Palcsey S, Nolfi A, Feola A, et al. Vaginal degeneration following implantation of synthetic mesh with increased stiffness. BJOG. 2013;120(2):233–43.
Chen B, Yeh J. Alterations in connective tissue metabolism in stress incontinence and prolapse. J Urol. 2011;186(5):1768–72.
Fan X, Wang Y, Wang Y, Xu H. Comparison of polypropylene mesh and porcine-derived, cross-linked urinary bladder matrix materials implanted in the rabbit vagina and abdomen. Int Urogynecol J. 2014;25(5):683–9.
Feola A, Abramowitch S, Jallah Z, Stein S, Barone W, Palcsey S, et al. Deterioration in biomechanical properties of the vagina following implantation of a high-stiffness prolapse mesh. BJOG. 2013;120(2):224–32.
Mazza E, Ehret AE. Mechanical biocompatibility of highly deformable biomedical materials. J Mech Behav Biomed Mater. 2015;48:100–24.
Mohammadi M, Dryden JR, Jiang L. Stress concentration around a hole in a radially inhomogeneous plate. Int J Solids Struct. 2011;48(3–4):483–91.
Acknowledgements
The animal study was conducted at Beijing Key Laboratory of Pre-clinical Research and Evaluation for Cardiovascular Implant Materials. The authors thank Bin Li, Boqing Yang, and Liujun Jia, who participated in the anesthesia procedure of the sheep.
Funding
This study received financial support from the National Natural Science Foundation of China (number: 81771561), and Strategic Priority Research Program of the Chinese Academy of Sciences (XDA16010102).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Details of ethics approval
The study was approved by the ethics committee of FUWAI Hospital, Chinese Academy of Medical Sciences (0079-2-36-HX(X)).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ai, FF., Mao, M., Zhang, Y. et al. Experimental study of a new original mesh developed for pelvic floor reconstructive surgery. Int Urogynecol J 31, 79–89 (2020). https://doi.org/10.1007/s00192-019-03947-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-03947-4