Abstract
Introduction and hypothesis
Resident involvement in complex surgeries is under scrutiny with increasing attention paid to health care efficiency and quality. Outcomes of urogynecological surgery with resident involvement are poorly described. We hypothesized that resident surgical involvement does not influence perioperative outcomes in minimally invasive abdominal sacrocolpopexy (ASC).
Methods
Using the 2006–2012 National Surgical Quality Improvement Program database, we identified 450 cases of laparoscopic or robotic ASC performed with resident involvement. Resident operative participation was stratified by experience (junior [PGY 1–3] vs senior level [PGY ≥4]). The primary outcome was operative time, and multinomial logistic regression was used to determine the effects of resident involvement and experience. Chi-squared analyses were used to assess the relationship between resident participation with length of stay (LOS) and 30-day complications and readmissions.
Results
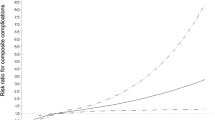
Residents participated in 74% (n = 334) of these surgeries, and these cases were significantly longer (median 220 vs 195 min, p = 0.03). On multivariate analysis, senior level resident involvement was associated with longer operative times across all time intervals compared with <2 h (2 to ≤4 h relative risk reduction [RRR] 4.1, p = 0.007, CI 1.47–11.40; 4 to ≤6 h RRR 6.6, p = 0.001, CI 2.23–19.44; ≥6 h RRR 4.7, p = 0.020, CI 1.28–17.43). Resident participation was not associated with LOS, readmissions, or complications.
Conclusions
Senior level resident involvement in minimally invasive ASC is associated with longer operative times, with no association with LOS or adverse perioperative outcomes. The educational benefit of surgical training does not adversely affect patient outcomes for ASC.


Similar content being viewed by others
References
Iglehart JK. Revisiting duty-hour limits—IOM recommendations for patient safety and resident education. N Engl J Med. 2008;359(25):2633–5. https://doi.org/10.1056/NEJMp0808736.
Ferraris VA, Harris JW, Martin JT, Saha SP, Endean ED. Impact of residents on surgical outcomes in high-complexity procedures. J Am Coll Surg. 2016;222(4):545–55. https://doi.org/10.1016/j.jamcollsurg.2015.12.056.
Castleberry AW, Clary BM, Migaly J, Worni M, Ferranti JM, Pappas TN, et al. Resident education in the era of patient safety: a nationwide analysis of outcomes and complications in resident-assisted oncologic surgery. Ann Surg Oncol. 2013;20(12):3715–24. https://doi.org/10.1245/s10434-013-3079-2.
Matulewicz RS, Pilecki M, Rambachan A, Kim JY, Kundu SD. Impact of resident involvement on urological surgery outcomes: an analysis of 40,000 patients from the ACS NSQIP database. J Urol. 2014;192(3):885–90. https://doi.org/10.1016/j.juro.2014.03.096.
Davis SS Jr, Husain FA, Lin E, Nandipati KC, Perez S, Sweeney JF. Resident participation in index laparoscopic general surgical cases: impact of the learning environment on surgical outcomes. J Am Coll Surg. 2013;216(1):96–104. https://doi.org/10.1016/j.jamcollsurg.2012.08.014.
Igwe E, Hernandez E, Rose S, Uppal S. Resident participation in laparoscopic hysterectomy: impact of trainee involvement on operative times and surgical outcomes. Am J Obstet Gynecol. 2014;211(5):484.e1–7. https://doi.org/10.1016/j.ajog.2014.06.024.
Committee on the Governance and Financing of Graduate Medical Education; Board on Health Care Services; Institute of Medicine; Eden J, Berwick D, Wilensky G (eds) Graduate medical education that meets the nation's health needs. Washington, DC: National Academies Press. 2014. https://doi.org/10.17226/18754
Gonzalez CM, McKenna P. Challenges facing academic urology training programs: an impending crisis. Urology. 2013;81(3):475–9. https://doi.org/10.1016/j.urology.2012.12.004.
Hwang CS, Wichterman KA, Alfrey EJ. The cost of resident education. J Surg Res. 2010;163(1):18–23. https://doi.org/10.1016/j.jss.2010.03.013.
Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter HE, et al. Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstet Gynecol. 2014;123(1):141–8. https://doi.org/10.1097/aog.0000000000000057.
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300(11):1311–6. https://doi.org/10.1001/jama.300.11.1311.
Rortveit G, Brown JS, Thom DH, Van Den Eeden SK, Creasman JM, Subak LL. Symptomatic pelvic organ prolapse: prevalence and risk factors in a population-based, racially diverse cohort. Obstet Gynecol. 2007;109(6):1396–403. https://doi.org/10.1097/01.aog.0000263469.68106.90.
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson Funk M. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201–6. https://doi.org/10.1097/aog.0000000000000286.
Maher C, Feiner B, Baessler K, Schmid C (2013) Surgical management of pelvic organ prolapse in women. The Cochrane database of systematic reviews (4):Cd004014. https://doi.org/10.1002/14651858.CD004014.pub5.
Paraiso MF, Jelovsek JE, Frick A, Chen CC, Barber MD. Laparoscopic compared with robotic sacrocolpopexy for vaginal prolapse: a randomized controlled trial. Obstet Gynecol. 2011;118(5):1005–13. https://doi.org/10.1097/AOG.0b013e318231537c.
American College of Surgeons. About ACS NSQIP. Available at https://www.facs.org/quality-programs/acs-nsqip/about. Accessed 28 April 2016.
PUF Data Dictionary Items | National Cancer Data Base—Data Dictionary PUF 2013. Available at http://ncdbpuf.facs.org/node/259. Accessed 25 April 2016.
American College of Surgeons National Surgical Quality Improvement Program: user guide for the 2012 ACS NSQIP participant use data file. October 2013. Available at https://www.facs.org/~/media/files/qualityprograms/nsqip/ug12.ashx. Accessed 28 April 2016.
Papandria D, Rhee D, Ortega G, Zhang Y, Gorgy A, Makary MA, et al. Assessing trainee impact on operative time for common general surgical procedures in ACS-NSQIP. J Surg Educ. 2012;69(2):149–55. https://doi.org/10.1016/j.jsurg.2011.08.003.
Gorgun E, Benlice C, Corrao E, Hammel J, Isik O, Hull T, et al. Outcomes associated with resident involvement in laparoscopic colorectal surgery suggest a need for earlier and more intensive resident training. Surgery. 2014;156(4):825–32. https://doi.org/10.1016/j.surg.2014.06.072.
Harrington DT, Roye GD, Ryder BA, Miner TJ, Richardson P, Cioffi WG. A time-cost analysis of teaching a laparoscopic entero-enterostomy. J Surg Educ. 2007;64(6):342–5. https://doi.org/10.1016/j.jsurg.2007.06.009.
Saliba AN, Taher AT, Tamim H, Harb AR, Mailhac A, Radwan A, et al. Impact of resident involvement in surgery (IRIS-NSQIP): looking at the bigger picture based on the American College of Surgeons-NSQIP database. J Am Coll Surg. 2016;222(1):30–40. https://doi.org/10.1016/j.jamcollsurg.2015.10.011.
D'Souza N, Hashimoto DA, Gurusamy K, Aggarwal R. Comparative outcomes of resident vs attending performed surgery: a systematic review and meta-analysis. J Surg Educ. 2016;73(3):391–9. https://doi.org/10.1016/j.jsurg.2016.01.002
Patel HD, Ball MW, Cohen JE, Kates M, Pierorazio PM, Allaf ME. Morbidity of urologic surgical procedures: an analysis of rates, risk factors, and outcomes. Urology. 2015;85(3):552–9. https://doi.org/10.1016/j.urology.2014.11.034.
Allen RW, Pruitt M, Taaffe KM. Effect of resident involvement on operative time and operating room staffing costs. J Surg Educ. 2016;73(6):979–85. https://doi.org/10.1016/j.jsurg.2016.05.014.
Mattar SG, Alseidi AA, Jones DB, Jeyarajah DR, Swanstrom LL, Aye RW, et al. General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann Surg. 2013;258(3):440–9. https://doi.org/10.1097/SLA.0b013e3182a191ca.
De Win G, Van Bruwaene S, Kulkarni J, Van Calster B, Aggarwal R, Allen C, et al. An evidence-based laparoscopic simulation curriculum shortens the clinical learning curve and reduces surgical adverse events. Adv Med Educ Pract. 2016;7:357–70. https://doi.org/10.2147/amep.s102000.
Finan MA, Clark ME, Rocconi RP. A novel method for training residents in robotic hysterectomy. J Robot Surg. 2010;4(1):33–9. https://doi.org/10.1007/s11701-010-0179-x.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
SP Kim is funded by a career development award from the Conquer Cancer Foundation of the American Society of Clinical Oncology (ASCO) and the NIH from MD12–003.
AK Hijaz is a member of the Astellas, Inc. Speaker’s Bureau.
ST Mahajan is a member of the Astellas, Inc. Speaker’s Bureau and receives grant funding from Allergan, Inc.
EA Slopnick, JW Henderson, and CT Nguyen do not have any conflicts of interest.
Author participation
EA Slopnick: project development, data management, data analysis, manuscript writing and editing; AK Hijaz: project development, manuscript editing; JW Henderson: manuscript editing; ST Mahajan: project development, manuscript editing; CT Nguyen: data management; SP Kim: data management, data analysis, manuscript writing/editing.
Rights and permissions
About this article
Cite this article
Slopnick, E.A., Hijaz, A.K., Henderson, J.W. et al. Outcomes of minimally invasive abdominal sacrocolpopexy with resident operative involvement. Int Urogynecol J 29, 1537–1542 (2018). https://doi.org/10.1007/s00192-018-3578-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3578-6